COVID-19 infection has shown cardiovascular involvement, particularly when it has a moderate to severe presentation. This alteration has been manifested in arrhythmias, myocarditis, and acute myocardial infarction, among others; persistence of these cardiovascular alterations in the short and medium term has been documented. In Latin America there are no reports of long-term cardiovascular sequelae. We present the case of a 46-year-old female with no previous history of cardiovascular disease who developed a severe COVID-19 infection, positive by PCR, requiring prolonged orotracheal intubation. Treatment was based on steroids, antibiotic therapy, and anticoagulants. Transthoracic echocardiography (TTE) confirmed pericarditis during the acute phase, with persistent sequelae of cardiac dysfunction. Follow up by the cardiology service was done with echocardiography, manifesting myocardial dysfunction up to 2 years after the acute event. This case shows that severe infection by COVID-19 can cause cardiovascular alterations in addition to producing potentially permanent and disabling sequelae.
COVID-19, Cardiomyopathy, Cardiovascular Sequelae, TTE
WHO: World Health Organization; ACE2: Angiotensin Receptor 2; TTE: Transthoracic Echocardiography; LVEF: Left Ventricular Ejection Fraction; PCR: Polymerase Chain Reaction
At the end of 2019, the first cases of pneumonia of unknown etiology were identified in Wuhan, China [1]. Different health emergency departments began to see outbreaks in neighboring countries and in travelers [2,3]. The WHO declared a public health emergency of international significance in January 2020 and confirmed a pandemic in March 2020. From the first cases to July 7, 2022, more than 558 million people have been confirmed infected and more than 6.3 million deaths have occurred globally [4,5]. Currently, the COVID-19 disease has been one of the deadliest viral infections of the respiratory type that humanity has faced. From the beginning of the disease, little was known about the pathophysiological outcomes that it could produce, and perhaps future effects remain to be discovered [4,6]. One of the first challenges was understanding the natural history of COVID-19 disease. Initial reports described the initial symptoms as those of a common viral infection, similar to that of influenza, but with a possible fatal outcome of acute respiratory distress syndrome accompanied by cardiac alterations and shock [7,8]. Gupta A, et al. described that COVID-19 can cause extrapulmonary manifestations. These could include thrombotic complications, myocardial dysfunction and arrhythmia, and acute coronary syndromes, among others [9]. Researchers defined virus entry through ACE2 as the mechanism of multi-organ damage since ACE2 is expressed in multiple tissues, particularly cardiac and endothelial tissue [10,11].
Two studies published in JAMA Cardiology had a detailed report on cardiovascular complications in patients infected with COVID-19. Shi, et al. reported the presence of cardiac injury among hospitalized patients secondary to COVID-19 in Wuhan, China, and its association with a higher risk of hospital mortality. Guo, et al. showed that myocardial injuries were significantly associated with fatal outcomes in COVID-19 [12,13]. A relationship was observed between COVID-19 infection and myocardial injury, cardiac dysfunction, and possible development of chronic heart disease. Researchers proposed inflammation and cytokine storm as a pathophysiological mechanism that produces myocardial injury and induces permanent alterations resulting from the high affinity of SARS-CoV-2 to ACE2 expressed in the heart [14-16]. COVID-19 has generated interest in the international cardiology community due to its apparent link to cardiovascular disease and the development of heart disease in previously healthy subjects. Early in the pandemic, patients with cardiovascular comorbidities were shown to be more vulnerable to viral infection with a higher rate of complications and admission to intensive care units [17,18]. In a study of 44,672 confirmed cases, higher case fatality rates were observed in patients with pre-existing cardiovascular problems (10.5%) than in diabetes (7.3%) and hypertension (6%) [19].
The clinical studies that showed the involvement of SARS-CoV-2 and cardiovascular clinical manifestations generated research to describe the pathophysiology. The mechanism of intracellular entry was discovered. The viral envelope expresses a protein called SPIKE (protein S), which contains a receptor-binding region that binds ACE2 on the human extracellular membrane with high affinity. In addition, internalization of ACE2 by the entry mechanism results in the loss of ACE2 on the cell surface. This abolishes a key pathway for the cell to degrade ANG II and generate the cardiovascular disease-protective ANG-1-7. Therefore, explaining the main mechanism of cardiovascular injury and possible persistence afterwards [20,21]. The myocardial damage caused by COVID-19 further consolidated the cardiovascular implications seen during the post-covid phase [22]. A study by Veteran's Affairs Healthcare revealed a relationship between arrhythmias, ischemic heart disease, heart failure, and thrombotic disorders between 30 days and 12 months after infection [23,24]. Cardiac magnetic resonance imaging was used to address the cardiovascular involvement of SARS-CoV-2 and determine the acute and chronic consequences. The new technology has managed to characterize the structural changes after COVID-19 infection in the myocardium [25,26]. Follow-up studies have been carried out, using this new technology, for 2 to 3 months, where it has been shown that a significant percentage of patients who recovered from infection showed abnormalities on cardiac MRI, with more than half of them showing evidence of inflammation, focal scarring, and pericardial enhancement [26,27]. Thus, explaining the increase in patients with de novo heart disease after COVID-19 and the increase in hospitalizations for cardiac pathologies associated with post-COVID sequelae [27,28].
The objective of this study is to present the case of a patient with persistent cardiac sequelae two years after suffering from severe COVID.
A 46-year-old woman who presented in the emergency department with a severe COVID-19 infection required advanced airway management from her admission on May 3 until June 5, 2020. She presented a positive PCR test and compatible chest tomography for SARS-CoV infection. During the acute phase, the patient presented suspicion of myocarditis (Figure 1). Pericarditis was confirmed by the cardiology service with TTE after discharge. Among her family history, she mentioned a mother with type 2 diabetes and hypertension. Mentioning a personal history of type 2 diabetes with five years of diagnosis and treatment with glimepiride 2 mg daily. During hospitalization, the patient presented torpid evolution with infection associated with mechanical ventilation at the expense of Streptococcus pneumoniae, persistent hypotension, and tracheostomy due to prolonged intubation. Acute phase treatment was based on pulses of parenteral methylprednisolone 1g every 24 hours for five cycles; parenteral dexamethasone 8 mg every 24 hours for seven days; an initial antibiotic with parenteral ceftriaxone 1g every 24 hours; subsequent escalation to meropenem 1g parenteral every 8 hours; and anticoagulation with enoxaparin 60 mg subcutaneously every 12 hours.
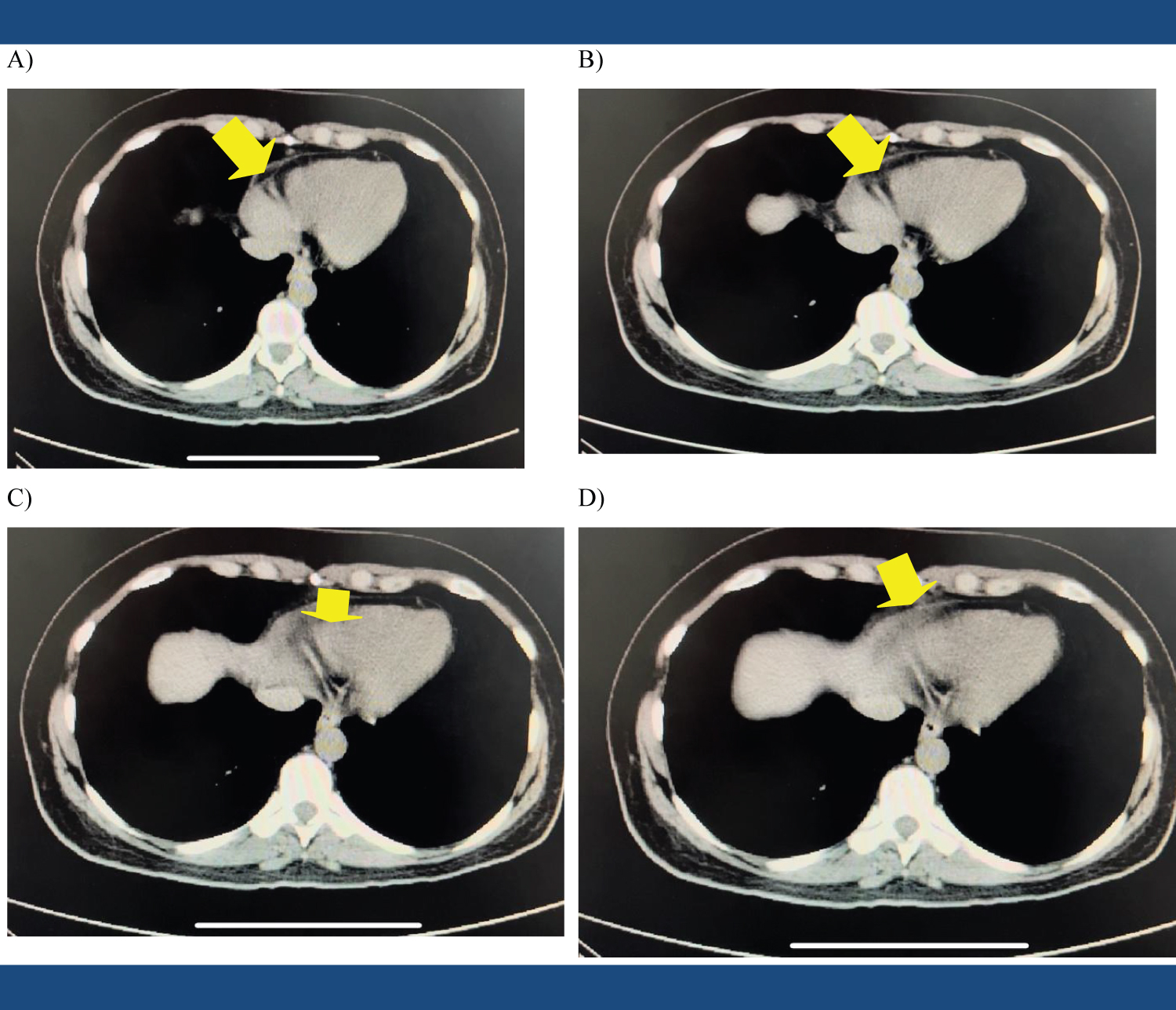 Figure 1: Thorax CT scan: Mediastinal phase with presence of myocardial thickening and pericardial effusion.
View Figure 1
Figure 1: Thorax CT scan: Mediastinal phase with presence of myocardial thickening and pericardial effusion.
View Figure 1
The patient was discharged on June 5, 2020 with persistent dyspnea as an expected sequelae. The PCR test was negative on June 15, 2020. On June 25, 2020, the cardiology service performed TTE (Table 1) that reported a non-hypertrophic, non-dilated left ventricle with a preserved LVEF of 62% by Teicholz and 58% by Modified Simpson, mild diastolic dysfunction. The right ventricle's systolic function is preserved. A non-dilated left atrium and right atrium, both without intracavitary thrombi. Normal functioning valves. The posterior pericardium appeared hyper refractory. Diagnostic impression by TTE: Pericarditis. The patient continued with outpatient management and was sent for monthly check-ups with the family doctor. In January 2021, the patient was diagnosed with systemic arterial hypertension and was reassessed by cardiology, who started management with telmisartan 40 mg orally every 24 hours and hydrochlorothiazide 25 mg orally every 24 hours. TTE was performed on February 4 (Table 2), concluding: Non-hypertrophic, non-dilated left ventricle with borderline LVEF of 52% by Teicholz and 51% by Modified Simpson, slight diastolic dysfunction, and preserved right ventricular systolic function. Normal functioning valves. The patient was referred to the cardiologist in August 2022 for reporting dyspnea with large efforts when walking a kilometer and adding oppressive pain in the neck, sensations of dyspnea, dizziness, and fainting when performing physical activity such as climbing a floor through the stairs, which improved with rest. The patient also reported palpitations during the early morning hours of seconds in duration, four times a month, as well as edema of the lower limbs, predominantly symmetrical in the evening. NYHA functional class II was determined.
Table 1: TTE Initial (June 25, 2020). View Table 1
Table 2: TTE subsequent (4th of February 2021). View Table 2
Multiple investigations have been carried out where there is a presence of long-term cardiological complications due to COVID-19, and these are more evident due to the passage of time and the collection of new data [26,29]. In Latin America, there are few reports of myocardial injury secondary to infection by SARS-CoV-2 and almost no reports of medium-to long-term sequelae after infection. This is a report of heart disease confirmed by alterations in the TTE, secondary to COVID-19 infection, that persists after two years from the onset of symptoms. International studies have shown that patients infected with SARS-CoV-2, in the context of pre-existing cardiovascular disease, have an increased risk of severe illness and death [12,13]. One study demonstrated an 8% risk of acute cardiac injury in COVID-19 patients, with a 13-fold higher incidence in critically ill patients [30]. Several investigators have proposed that the altered inflammatory response during the acute phase of COVID-19 and the alteration of the immunomodulatory system could be a pathophysiological mechanism related to the presence of myocardial injury [14-16]. The very mechanism of cellular entry, by the viral coat protein, to the ACE 2 cell membrane receptor conditions its internalization, which cancels a key pathway for the cell to degrade ANG II and generate Ang-(1-7), a mechanism for innate cardiovascular cytoprotection [20,21]. Once the relationship between myocardial damage and SARS-CoV-2 was established, subsequent reports during the pandemic consolidated the post covid cardiovascular sequelae seen, such as myocarditis, stress cardiomyopathy, acute myocardial infarction, and arrhythmias [22].
In the long term, this could indicate an increase in new heart problems and a higher rate of hospitalizations for cardiac pathologies associated with post-COVID sequelae. In addition, it would imply a direct relationship between infection by SARS-Covid-19 and an increase in cardiovascular risk in previously healthy patients [26-28]. Despite advances, doubts remain regarding long-term cardiac deleterious effects. Arévalos V, et al. designed a multicenter, observational, retrospective study protocol to be carried out in 17 centers with the objective of reporting cardiovascular mortality 1 year after SARS-CoV-2 infection and the incidence of acute myocardial infarction, stroke, hospitalization for heart failure, pulmonary embolism, and serious cardiac arrhythmias per year [29]. These types of studies are needed to understand the clinical implications of COVID-19 and its persistent cardiovascular effects and to demonstrate how this may progress during the lifetime of patients.
Finally, this case report aims to help introduce the Latin American medical community to possible specific cardiac sequelae in previously healthy patients. Identify the outcomes, from the onset of persistent cardiac symptoms caused by COVID-19 to significant implications for patient well-being. The goal is to pave the way for more research, improve the knowledge of doctors, reorganize medical guidelines and concepts of the health system, and prevent harmful economic and social effects. The cardio pathological evidence in this report and its persistence after COVID-19 infection is consistent with international reports. This case is a clear example of how the COVID-19 infection produced significant inflammation at the myocardial level, evidenced by the initial diagnostic imaging tests and showing clinical persistence two years later, together with imaging evidence of a 10-percent reduced LVEF by TTE at nine months.
The reduction in the ejection fraction shown in this patient not only aggravates functionality and work capacity but also increases the risk of cardiovascular mortality according to what has already been reported [16]. The clinician should consider a high level of suspicion of possible cardiovascular alteration in patients with moderate to severe acute SARS-CoV-2 infection and request appropriate images to rule out or confirm it, so that therapy can be started to prevent long-term complications. In addition to this, this report could be a good example of the need for early cardiovascular surveillance in COVID-19 infection.
Our case demonstrates that, in the context of the progression of severity due to COVID-19, cardiac alterations should be readily considered based on the international evidence. This patient's clinical manifestations and the torpid evolution probably represented a severe COVID-19 infection that led to cardiac involvement due to the presence of hypotension and persistence of dyspnea at discharge. Severe COVID infection, without prevention or suspicion of extrapulmonary alterations, allowed the development of myocarditis that finally resulted in long-term cardiac alteration. Physicians must be vigilant in recognizing the COVID-19 infection, its possible acute cardiovascular complications, as well as its long-term complications.
A deliberate search for myocardial involvement should be suspected and performed in patients with severe COVID-19 infection. COVID-19 causes myocarditis, acute coronary syndrome, and alterations in myocardial electrical conduction. Imaging studies to determine the etiology of cardiovascular symptomatology can serve as a critical branch point in patient care decisions during acute infection and help to account for the cardiac alteration's potential permanence.
The authors declare no conflict of interest in this clinical case presentation.
The authors declare that they have the written permission of the patient so that all the material of the clinical history, images, and any other type of information about the patient is published in a medical journal or congress that the authors consider relevant for scientific and educational purposes. Trying, as much as possible, to maintain the anonymity of the identity in the text and in the images. This authorization includes publication in Spanish and its translation into English, in print, in electronic format on the journal's website, and in any other format used by the scientific journal now and in the future.
The authors received no funding for this case presentation.