Cavernous sinus thrombosis is a life-threatening condition that arises as a complication of facial infection, sinusitis, orbital cellulitis, pharyngitis, or otitis of fungal or bacterial origin or after traumatic injury or surgery. Rhinocerebral mucormycosis is an aggressive infection that, depending on its level of extension, affects nasal passages, paranasal sinuses and the orbital region and, in the worst-case scenario, invades the brain. Infections that spread into the cranial cavity can lead to cavernous sinus thrombosis. We present the case of a patient with Cavernous Sinus Thrombosis diagnosed with Rhinocerebral Mucormycosis.
Cavernous sinus, Thrombosis, Mucormycosis
Cavernous sinus thrombosis is a life-threatening infection with a mortality rate of 30% to 40% caused by retrograde spread infection from the upper dentition or paranasal sinuses through the valveless ophthalmic venous system to the cavernous sinus [1]. The development of thrombosis within the cavernous sinuses causes decreased drainage of the superior and inferior ophthalmic veins, resulting in periorbital edema, ptosis, proptosis, chemosis, ophthalmoplegia, and vision loss [2].
Mucormycosis is a fungal infection caused by fungi belonging to the order Mucorales [3]. Rhino-orbito-cerebral mucormycosis can occur at any age and in patients of any race, sex, especially in diabetic or severely immunocompromised patients [4,5]. These infections are becoming more common and are associated with very low survival rates [5]. The clinical hallmark of invasive mucormycosis is tissue necrosis as a result of angioinvasion and subsequent thrombosis.
The ongoing COVID-19 pandemic has caused a sudden increase in cases of mucormycosis associated with COVID19, mainly in developing countries [6]. Cavernous sinus thrombosis, secondary to fungal involvement, is rarely found [7] and there are few reported cases. A case of cavernous sinus thrombosis is presented in a patient with Rhinocerebral Mucormycosis associated with Covid.
This paper reports the case of a 51-year-old male patient who attend to the Maxillofacial Surgery service of the University Hospital of Maracaibo with a diagnosis of Rhinocerebral mucormycosis with 4 months of evolution with a history of type II diabetes mellitus and survivor of Covid 19. Clinical Extraoral examination showed volume increase in the right orbital region with total palpebral occlusion, fluctuating on palpation, non-reactive right pupil, loss of vision, ophthalmoplegia, chemosis and ipsilateral proptosis (Figure 1). Intraoral clinical examination evidenced mobility of the anterior and lateral segment on the right side of the maxilla. The imaging examination through CT of the Face showed changes in the densities of the Maxilla compatible with bone resorption that extended to the walls of the orbit and temporal bone on the right side. Mucosal thickening of the bilateral maxillary sinus, obstruction of the osteomeatal complex and involvement of the sphenoid sinus were observed (Figure 2). Clinical and imaging findings confirmed unilateral cavernous sinus thrombosis.
 Figure 1: Imaging show chemosis and eye ball proptosis.
View Figure 1
Figure 1: Imaging show chemosis and eye ball proptosis.
View Figure 1
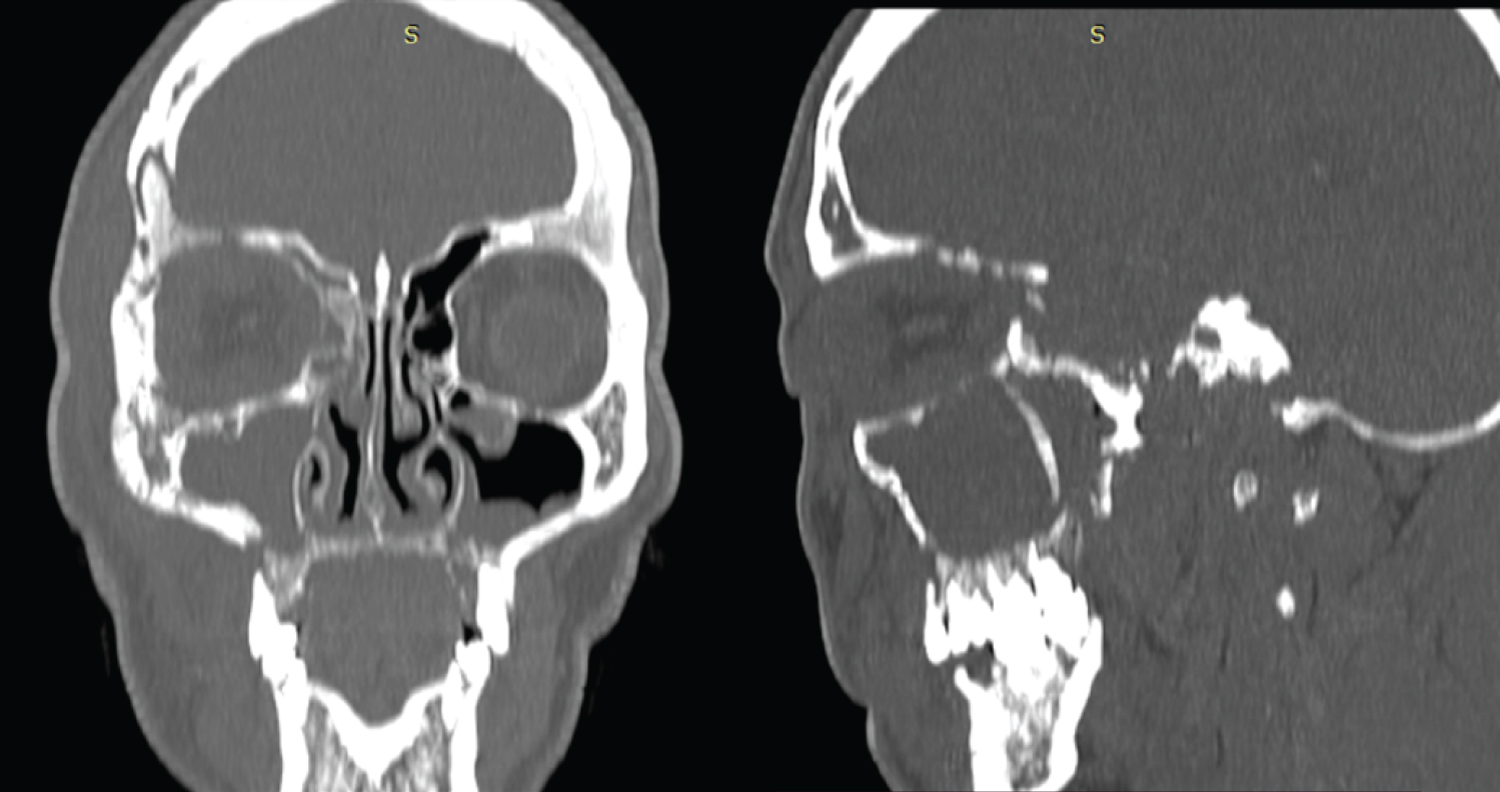 Figure 2: TC show changes in the densities of the maxilla compatible with bone resorption that extended to the walls of the orbit and temporal bone on the right side.
View Figure 2
Figure 2: TC show changes in the densities of the maxilla compatible with bone resorption that extended to the walls of the orbit and temporal bone on the right side.
View Figure 2
Cavernous sinus thrombosis is a life-threatening condition that, if recognized early, can reduce morbidity and mortality [8]. Septic cavernous sinus thrombosis is a thrombophlebitic process that typically arises from paranasal sinus infections and, with less frequently, otogenic, odontogenic and pharyngeal sources [9]. Cavernous sinus thrombosis can affect individuals of all ages, but occurs more frequently in young adults [10].
The clinical symptoms of cavernous sinus thrombosis arise from obstruction of the venous drainage of the cavernous sinus and compression of the associated cranial nerves [11]. Venous drainage and arterial blood supply to the orbits and sinuses lends itself to spread of bacterial and fungal pathogens to the cavernous sinus in a retrograde manner through the superior and inferior ophthalmic veins [8]. Ophthalmoplegia, an easy finding during clinical examination, is the result of dysfunction of cranial nerves III, IV, and VI. In the present study, orbital edema, vision loss, ophthalmoplegia, chemosis, and ipsilateral proptosis were the relevant clinical findings during the evaluation.
Mucormycosis is a fungal infection contracted by inhalation of Mucor and Rhizopus spores in the atmosphere, mainly affecting immunocompromised patients. Symptoms vary depending on the anatomical area involved; however, poorly controlled diabetic patients present more frequently a rhinocerebral infection [12]. The angioinvasive nature of Mucor leads to vasculitis and thrombosis that progress to tissue infarction and necrosis [13].
The diagnosis of cavernous sinus thrombosis is made on clinical grounds, with appropriate radiological imaging to confirm the diagnosis. Magnetic resonance imaging (MRI) is the most sensitive imaging modality; however, contrast-enhanced CT may be preferred as it is easier to obtain, more cost-effective, and effective when it comes to identify the integrity of the bony structures and/or the underlying source of infection. Computed tomography may reveal several subtle abnormalities, such as dilation of the superior and/or inferior ophthalmic veins, bulging of the lateral margins of the cavernous sinus, exophthalmos, and possibly the presence of sphenoid or ethmoid sinusitis, or mass lesions near the gland. sphenoid or pituitary [14].
Cavernous sinus thrombosis may be difficult to detect by CT or MR imaging in the early phase of the disease, Therefore, astute clinical examination with a high index of suspicion for cavernous sinus thrombosis, supported by known risk factors of diabetes, malignancy and immunosuppression, can lead to a diagnosis.