Bronchiolitis is a viral respiratory infection that is usually mild in infants less than one-year-old but can be serious and fatal in children with underlying heart disease. Our objective was to describe the epidemiological - clinical, therapeutic and evolutionary aspect of the bronchiolitis and heart disease association seen at the Tsaralalàna mother child hospital center.
This was a retrospective case-control study over a 5-year period from January 2016 to January 2021; 1 case was matched to 2 controls according to age and gender.
Seventy-five cases and 150 controls were included. Bronchiolitis associated with congenital heart disease accounted for 1% of admissions. The mean age was 4.03 months ± 2.9 with a sex ratio of 1.5. in 81.3% of cases, episodes of bronchiolitis were the mode of discovery of heart disease, the most frequent type of which was isolated ventricular septal defect (n = 34; 45.3%). Half of the cases presented a severe form. There was a statistically significant association between the severity of bronchiolitis (p = 0.00066; or = 2.66), treatment with oxygen therapy (p = 0.00000001; or = 22.37), duration of hospitalization (p = 0.00000007; or = 6.3), the progressive mode (p = 0.00001; or = 25.6) and the existence of an associated cardiopathy. The mortality rate was 14.7%.
Bronchiolitis is common in children with congenital heart disease. Thus, in the face of an episode of bronchiolitis and particularly in the severe forms, think about the possibility of an associated congenital heart disease.
Bronchiolitis, Congenital heart disease, Ventricular septal defect
Bronchiolitis is an epidemic and seasonal respiratory viral infection of infants under one year of age [1,2]. This pathology is now one of the most frequent causes of consultation and hospitalization in pediatric settings [3]. Bronchiolitis particularly affects infants aged 2 to 8 months, with a peak in frequency at 4 months during epidemics [1]. This pathology is usually benign and has a favorable prognosis [4,5]. It is fundamental to identify the criteria for clinical severity in bronchiolitis. However, some known factors would expose the infant to an increased risk of developing a severe form, especially in vulnerable children with underlying heart disease [6,7]. In Madagascar, heart defects are the most commonly found among congenital malformations with an estimated hospital prevalence of 8.65% in 2018, and most of these heart defects were diagnosed before the age of 12 months [8]. Children with congenital heart disease are also at significant risk of severe RSV infection. For those hospitalized, 3.4% had an intensive care unit stay and a higher mortality rate. The main objective is to describe the epidemiological, clinical, therapeutic and evolutionary profile of bronchiolitis in hospitalized children with heart disease and secondarily to determine the influence of congenital heart disease on bronchiolitis.
We carried out the present study at the Centre Hospitalier Universitaire Mère Enfant Tsaralalana (Chumet). It is a retrospective case-control study, carried out over a period of 5 years, from January 2016 To January 2021. The study population is made up of children aged less than 12 months admitted to Chumet with a diagnosis of bronchiolitis.
The criteria for inclusion were: Cases were defined as all patients less than 12 months of age admitted to chumet with a diagnosis of bronchiolitis and an associated congenital heart disease (regardless of the type of heart disease). Controls were defined as patients admitted for bronchiolitis without associated heart disease. Thus, two controls were matched to each case by age and gender.
The exclusion criteria were:
• Children aged 12 months and older
• A 3rd episode of bronchiolitis
• A 2nd hospitalization at chumet for the same reason
• Children suspected of having a congenital heart disease not confirmed by cardiac ultrasound
• Children discharged without medical advice
• Children transferred to another hospital
• Those whose medical observation form is incompletely completed
Bronchiolitis was diagnosed clinically in our study, we followed the diagnostic criteria of the HAS (Haute Autorité De Santé) [1].
Data were entered on Microsoft word and excel. Chi-square and student's t tests were used for data analysis with a significance level for a P value < 0.05.
During our study period, 11778 children were hospitalized at chumet, of which 2835 were bronchiolitis, or 24%. 120 children, or 1%, were admitted for bronchiolitis associated with congenital heart disease during the 5-year study period, of which 45 were excluded. We included 75 children in this study (Figure 1).
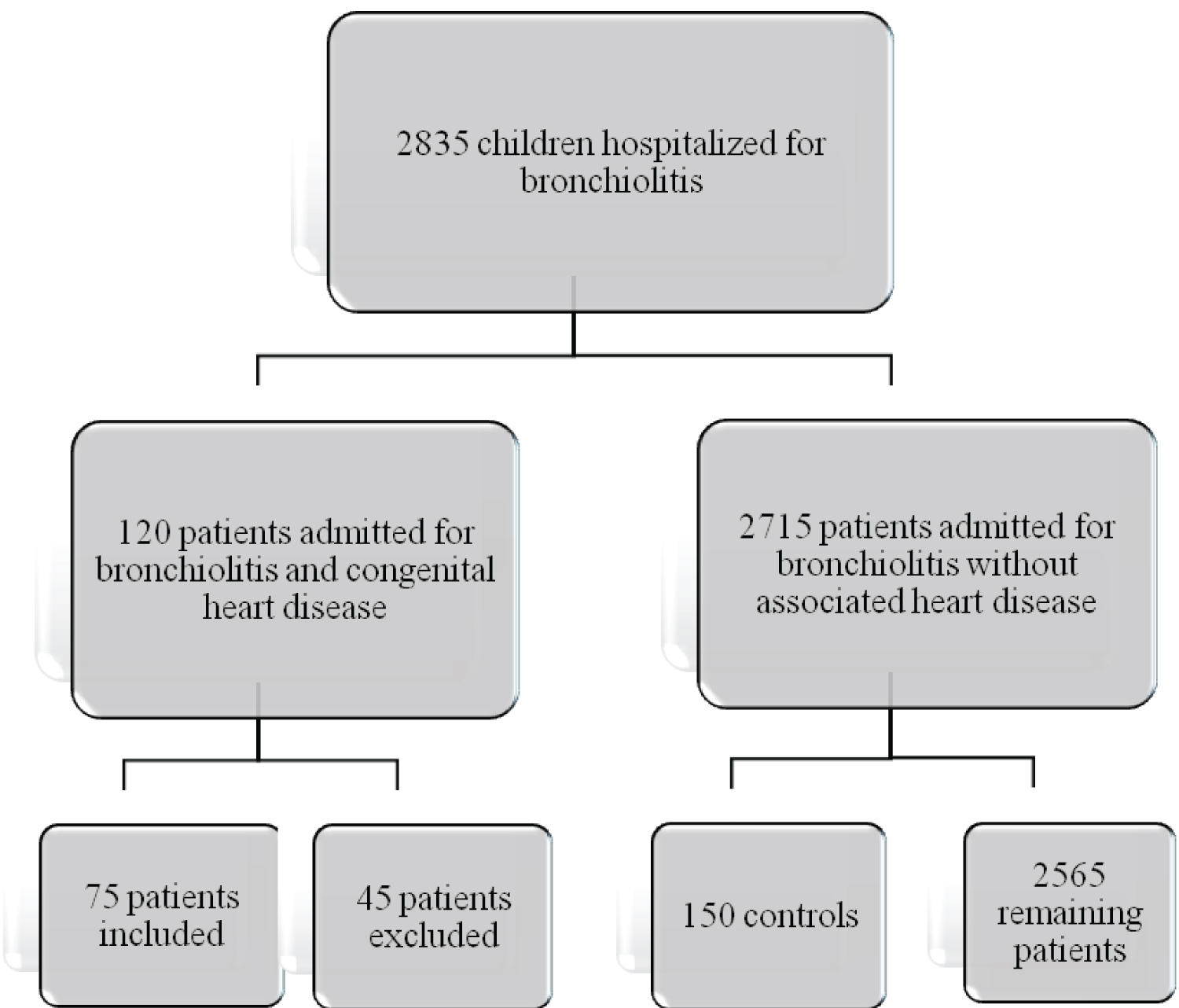 Figure 1: Study flow-chart: Selection of study data.
View Figure 1
Figure 1: Study flow-chart: Selection of study data.
View Figure 1
The mean age of our population is 4.03 ± 2.96 months, with a minimum of d9 and a maximum of 11 months. The majority of the children were less than 6 months of age with a sex ratio of 1.5.
Respiratory difficulty was the most common reason for hospitalization in 76% of cases, followed by refusal to nurse in 17%.
None of our patients received the RSV vaccine.
The majority of congenital heart disease was discovered during an episode of acute bronchiolitis. Isolated ventricular septal defect (VSD) was the most represented lesion with a rate of 43.33% (n = 34), followed by atrial canal persistence (PCA) with a rate of 29.33% (n = 22) and atrial septal defect (ASD) with a rate of 6.67% (n = 0.6). Eight (8) children had associated lesions i.e., 10.66%, the most frequent associations were VSD and ASD i.e., 8% (n = 6) (Figure 2).
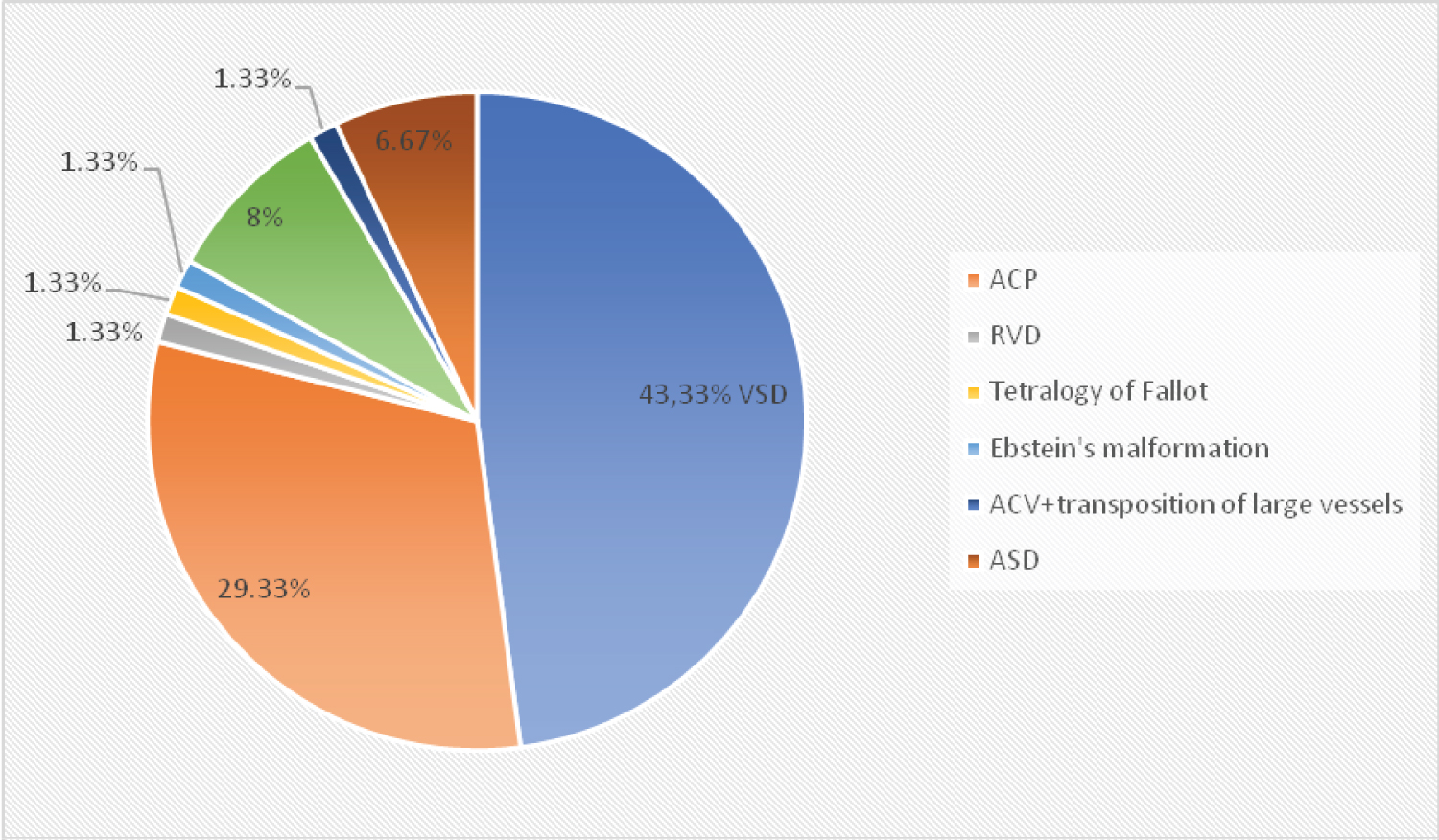 Figure 2: The different types of cardiopathy.
Figure 2: The different types of cardiopathy.
ASD: Atrial Septal Defect; ACP: Atrial Canal Persistence; VSD: Ventricular Septal Defects; TLV: Transposition of Large Vessels; RVD: Right Ventricle Double Outlet
View Figure 2
Bronchiolitis was severe with a Wang score higher than 8 in 53.3% of cases, with oxygen saturation lower than 90% in 97% of cases.
Treatment was dominated by antibiotic therapy (88%), oxygen therapy in 97% of cases. The average duration of oxygen therapy was 7.46 ± 8.20 days for the cases. The death rate was 14.67%.
The relationship between congenital heart disease and bronchiolitis is shown in Table 1.
Table 1: Factors influencing the course of bronchiolitis in children with heart disease. View Table 1
The hospital prevalence of bronchiolitis in the present study was 24%.
The association of bronchiolitis with congenital heart disease was 1%; largely lower than those reported in other studies which are 11.7% in the United States [9] and 7.8% in Austria [10]. This difference can be explained by the small size of our sample but also by the under-diagnosis of heart disease due to lack of resources.
The mean age of infants with bronchiolitis in our study was 4 ± 2 months which was slightly younger compared to that found by Bogne, et al. whose mean age was 8 months with a peak in infants from 2 to 4 months [11] but close to the value found by Resh, et al. with a mean age of 02 months. The peak frequency of bronchiolitis was from 03 to 06 months.
We note a male predominance in our study population, which is in line with the literature [11] with a sex ratio equal to 1.3. This could be due to the fragility of the male gender.
Bronchiolitis was severe in 53.3% of cases. This was slightly lower than 63% [9] and slightly higher than 49% in Korea [12] and 30% in the USA [13]. This is explained by the fact that underlying congenital heart disease is already a major vulnerability criterion for a small infant with bronchiolitis, especially for heart disease that has not yet been operated on as in our case [1].
The ventricular septal defect represented 47.3% of all heart diseases in our study, which differs from the literature where the interventricular septal defect represented only 4.7% of all heart diseases and with predominance for ventricular septal defects at 17.4% [14]. This difference could be explained by the fact that cardiac surgery is easily accessible in developed countries, especially for non-complex heart diseases such as ventricular septal defects.
On the therapeutic level, the need for oxygen therapy was 97% of the cases in our study with a mean duration of 7.4 days ± 8.2 days which was largely superior to that of the literature with a mean duration of 1 day and 50% of the children did not need oxygen therapy [10]. This difference could be explained by the fact that the children are not taken by the parents until the advanced stage of the disease resulting in a restriction of oxygen therapy.
The death rate was 14.7% in our study which was three times higher (4.4%) than that found by Jon WJ, et al. because in Korea they had introduced a protocol of prevention by Palizuvimab for fragile children such as carriers of congenital heart disease during the seasons of bronchiolitis epidemic [12].
Bronchiolitis is often a mode of discovery of congenital heart disease. The increased oxygen requirement increases with associated heart disease. Bronchiolitis was severe in more than half of the cases. The death rate was not negligible.
Palivizumab belongs to a class of drugs called monoclonal antibodies. Antibodies are cells that play a protective role against infections. Palivizumab is used to prevent serious respiratory tract (lung) infections caused by a virus called respiratory syncytial virus or RSV. It is given to babies and children who have risk factors for serious RSV lung infection, such as those born prematurely or those with heart or lung disease.
Perspectives: Use with easy access to Palivizumab to decrease the death rate in our country.
The authors declare no conflict of interest.
I would like to thank all the authors for their collaboration, their precious help, their patience, their proofreading and corrections.
All authors contributed to the conduct of this work. All authors also declare that they have read and approved the final version of the manuscript.