Background: Children with a solitary kidney are at risk of developing hypertension due to decreased nephron number with a consequence of hyperfiltration of the remnant. In patients with high-risk conditions, ambulatory blood pressure monitoring (ABPM), which records blood pressure (BP) for 24 hours, is helpful in detecting hypertension.
Objectives: To investigate the prevalence of hypertension in children with solitary kidney using 24-h ABPM and comparing with the office blood pressure (OBP).
Methods: Twenty-three patients aged 5-18 years-old were enrolled. Demographic, anthropometric and biochemical data were collected. OBP measurement with sphygmomanometer was recorded at the out-patient clinic, and patients were given a 24-h ABPM automatically records BP every 20 minutes during the day and every 30 minutes at night.
Results: Mean age of the subjects was 9.5 ± 3.9 years-old. Eleven patients (47.8%) were diagnosed with hypertension using 24-h ABPM, while only 6 patients (26.1%) were hypertensive using OBP measurement. Among 11 hypertensive patients in the ABPM group, 63.6% are considered to have masked hypertension. Subgroup analysis showed that obese had mean systolic BP load higher than non-obese, 48.1 ± 22.3% and 28.1 ± 17.3% respectively.
Conclusion: Hypertension in children with solitary kidney is seen more often if based on ABPM than on OBP measurement. Using 24-h ABPM in a high-risk group should be implemented in out-patient settings to early detect hypertension.
Ambulatory blood pressure monitoring, Solitary kidney, Hypertension
Prevalence of clinical hypertension in children is 3.28-4.32% [1]. There are many chronic conditions associated with high blood pressure including obesity, sleep disorders, history of prematurity and chronic kidney diseases [2]. The leading causes are renal problems accounting for approximately 90% of secondary hypertension [3]. Solitary kidney is one of the potential causes of developing hypertension later in life [4]. Prevalence of congenital unilateral agenesis is 4:10,000 at birth [5]. Similar to nephron under dosing hypothesis described in intrauterine growth retardation [6], renal mass reduction in solitary kidney can cause glomerular hyperfiltration and increased glomerular pressure which leads to the development of arterial hypertension and renal insufficiency [7]. Adaptive phenomenon in the remaining nephron called compensatory renal hypertrophy is also demonstrated [8]. There are evidences in animal models supported this pathogenesis [9].
Routine performing of an ambulatory blood pressure monitoring (ABPM) in high risk patients including chronic kidney disease has been recommended lately to early detect hypertension and masked hypertension [9]. Using ABPM can classify blood pressure into white coat hypertension (WCH), masked hypertension (MH), prehypertension and ambulatory hypertension. WCH is stress-induced elevated blood pressure inside the clinical setting [10]. It represents a stage between normotension and hypertension. MH is elevated ambulatory blood pressure but normotension by office blood pressure (OBP) measurement. The prevalence of MH is 7.6% in children [11].
The objective is to investigate the prevalence of hypertension and ABPM profile in solitary kidney patients, both congenital and acquired, as well as the ability of ABPM to detect hypertension when compared to usual OBP measurement.
A cross-sectional descriptive study of children with solitary kidney aged 5-16 years was conducted at King Chulalongkorn Memorial Hospital between 2020 and 2021. Patients with previously diagnosed hypertension, abnormality of the remaining kidney and abnormal renal function, eGFR < 60 ml/min/1.73 m2 calculated by Schwartz equation [12] were excluded. The study was approved by the Institutional Research Ethics Review Board of the Faculty of Medicine, Chulalongkorn University. Informed consent was obtained from participants and their parents.
Demographic data, clinical characteristic and laboratory results were recorded. OBP measurements were performed by means of the auscultatory method, using sphygmomanometer. All participants were monitored with the TM-2430 ABPM (A&D Company). Cuff size was chosen appropriately according to the patient arm width. The ABPM was recorded every 20 minutes during the day and every 30 minutes during night over a 24-h monitoring period. Recorded blood pressure values were calculated into mean systolic blood pressure (SBP) and diastolic blood pressure (DBP), pressure loads and dipping status. Calculated results were interpreted using age- and sex-specific percentile data as a reference [13]. Mean SBP or DBP higher than the 95th percentile indicate ambulatory hypertension [13]. BP load exceed 25% are considered abnormal [14] and BP dipping which is a declining of BP from daytime to nighttime should be more than 10% [15]. BP classification in 24-h ABPM includes WCH, MH, prehypertension and ambulatory hypertension. WCH is defined as hypertension by OBP measurement but normal blood pressure during 24-hs ABPM [10]. MH is an ambulatory hypertension but normal OBP.
Subgroup analysis was also done based on their body mass index (BMI), birth weight, etiology, dipping status and renal hypertrophy. Renal hypertrophy was defined as renal length greater than +2SD for age [16]. BMI divided, according to WHO BMI-for-age chart, into non-obese (underweight and healthy BMI) and obese subgroups (overweight and obesity BMI) [17].
The statistical analysis was performed using statistical package for social sciences (SPSS) program version 21.0. Continuous variables with a normal distribution were presented as mean and standard deviation (SD). Assessment of normality of data was determined using normality plots and the Kolmogorov-Smirnov test. Categorical variables were compared using Chi-square test. The differences of continuous variables between groups were analyzed by unpaired T-test for two groups. A p-value < 0.05 was considered statistically significant in all analyses.
Twenty-three patients were recruited to the study. The demographic, anthropometric and clinical characteristics are shown in Table 1. There were 15 patients with a congenital solitary kidney including renal agenesis, multicystic dysplastic kidney and atrophic kidney. Eight patients were solitary kidney by acquired cause such as Wilms' tumor, cystic dysplastic kidney and vesicoureteral reflux with severe hydronephrosis. Mean duration after nephrectomy was 72.8 ± 40.9 months. Renal hypertrophy was found in 9 patients. Two patients who have incomplete ABPM results were excluded.
Table 1: Demographic data, anthropometric data, renal function parameters and kidney length. View Table 1
Mean office SBP and DBP were 103.4 ± 11.7 and 64.1 ± 8.7 mmHg. From 23 patients, 6 patients (26.1%) were considered hypertension, 2 patients (8.7%) were elevated blood pressure and 15 patients (65.2%) were normotension (Table 2).
Table 2: Blood pressure categories in OBP measurement and ABPM. View Table 2
ABPM results were divided into 24-h, daytime and nighttime as shown in Table 3 and Figure 1. Mean 24-h SBP was 116.7 ± 11.3 which are significantly higher than mean office SBP (p-value < 0.001). Both mean daytime SBP and daytime DBP which are 122.3 ± 12.1 and 71.5 ± 6.1 are significantly higher than mean office SBP and DBP (p-value < 0.001 and 0.001 respectively). In contrast, mean nighttime DBP, 59.8 ± 7.4 was significantly lower than mean office DBP, 64.1 ± 8.7 suggested a physiologic BP dipping at nighttime. There are 7 patients who has daytime and nighttime BP different less than 10% also called non-dippers.
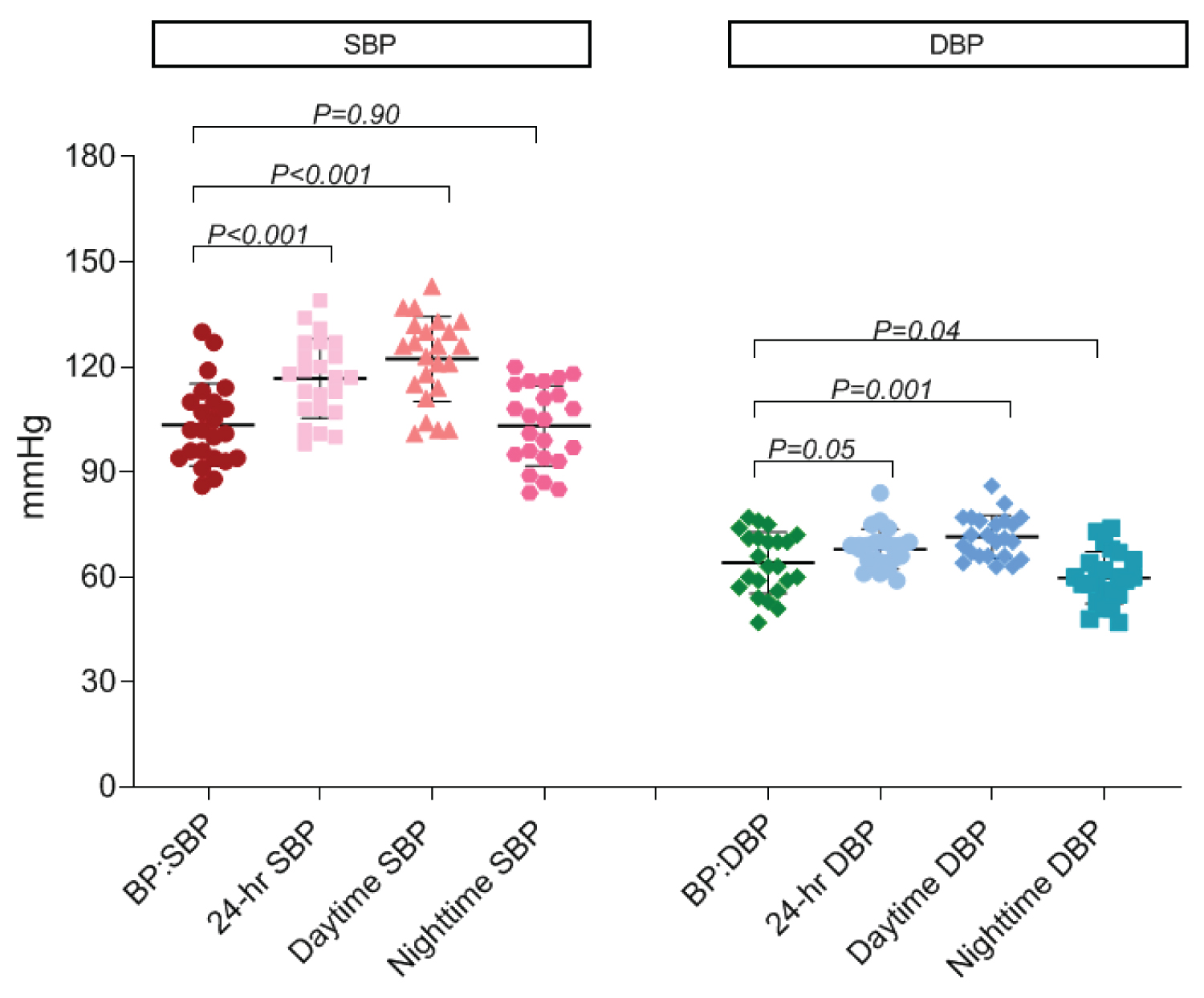 Figure 1: Compare mean of SBP and DBP between OBP and ABPM using paired t-test.
View Figure 1
Figure 1: Compare mean of SBP and DBP between OBP and ABPM using paired t-test.
View Figure 1
Table 3: Compare ABPM parameter and OBP measure. View Table 3
From 23 patients, there were 11 patients (47.8%) diagnosed with hypertension using 24-h ABPM, while only 26.1% were hypertensive using OBP. Among 11 hypertensive patients in ABPM group, 7 patients (63.6%) were considered masked hypertension. The study showed that more solitary kidney patients were diagnosed with hypertension by using ABPM.
Other factors that might associated with ABPM profiles were analyze in subgroup analysis. According to WHO BMI-for-age chart, BMI was divided into non-obese and obese subgroups as shown in Table 4. In non-obese group of 18 patients, mean 24-h SBP was 114.6 ± 11 mmHg and mean 24-h DBP was 67.2 ± 4 mmHg. In obese group which has 5 patients, mean 24-h SBP was 124.2 ± 9.8 mmHg and mean 24-h DBP was 70.6 ± 9.8 mmHg. There was no statistically significant difference in mean 24-h SBP and DBP between BMI subgroups (p-value 0.09, 0.25 respectively). However, SBP load has a significant difference between these 2 subgroups. Mean SBP load in non-obese group was 28.1 ± 17.3% and 48.1 ± 22.3% in obese group (p-value 0.04).
Table 4: ABPM profiles in non-obese and obese. View Table 4
Birth weight was also divided into two subgroups consisting of 19 normal birth weight patients (more than 2500 g) and 3 low birth weight patients (less than 2500). In normal birth weight group, mean 24-h SBP was 118.11 ± 10.9 mmHg and mean 24-h DBP was 68.47 ± 5.91 mmHg. Comparing with low birth weight group, mean 24-h SBP was 111 ± 14.73 mmHg and mean 24-h DBP was 64.33 ± 4.16 (p-value 0.33). Statistical significance in ABPM profiles difference could not be identified between birth weight subgroups.
In congenital and acquired solitary kidney consisting of 15 and 8 patients, the mean 24-h SBP was 114.1 ± 11.2 and 121.5 ± 10.5 mmHg respectively, and the mean 24-h DBP was 68.4 ± 6.5 and 67.1 ± 4.1 mmHg. There was no significant in mean blood pressure between these two groups. The numbers of congenital solitary kidney patients defined as hypertension using ABPM were 7/15 (46.7%) and 4/8 (50%) in the congenital and acquired groups but it was not statistically significant.
The dipping status was divided into 15 dippers and 8 non-dippers. The results showed differences in nighttime SBP which is 99.2 ± 10.7 mmHg in dippers and 110.5 ± 9.49 mmHg in non-dippers (p-value 0.02) and nighttime DBP which is 57.4 ± 7.1 mmHg in dippers and 64.25 ± 6.11 mmHg in non-dippers (p-value 0.03). There was no difference in mean 24-h blood pressure and other parameters. Six patients (40%) in the dipper group were considered hypertension and 5 patients (62.5%) in the non-dipper group had hypertension as well.
In subgroup of renal size, 14 patients had normal renal size and 9 patients had renal hypertrophy. Mean nighttime SBP was 109.11 ± 9.41 mmHg in hypertrophy group which were significantly higher than 99.29 ± 11.26 mmHg in normal renal size group (p-value 0.04). No significant difference in other BP profiles was found.
When using Pearson correlation to study ABPM parameters and risk factors for hypertension including BMI, birth weight, eGFR and kidney length, it was found that among these potential factors, kidney length was the only factor inversely correlated with 24-h DBP and daytime DBP (p-value 0.01 and 0.01), as shown in Figure 2 and Figure 3.
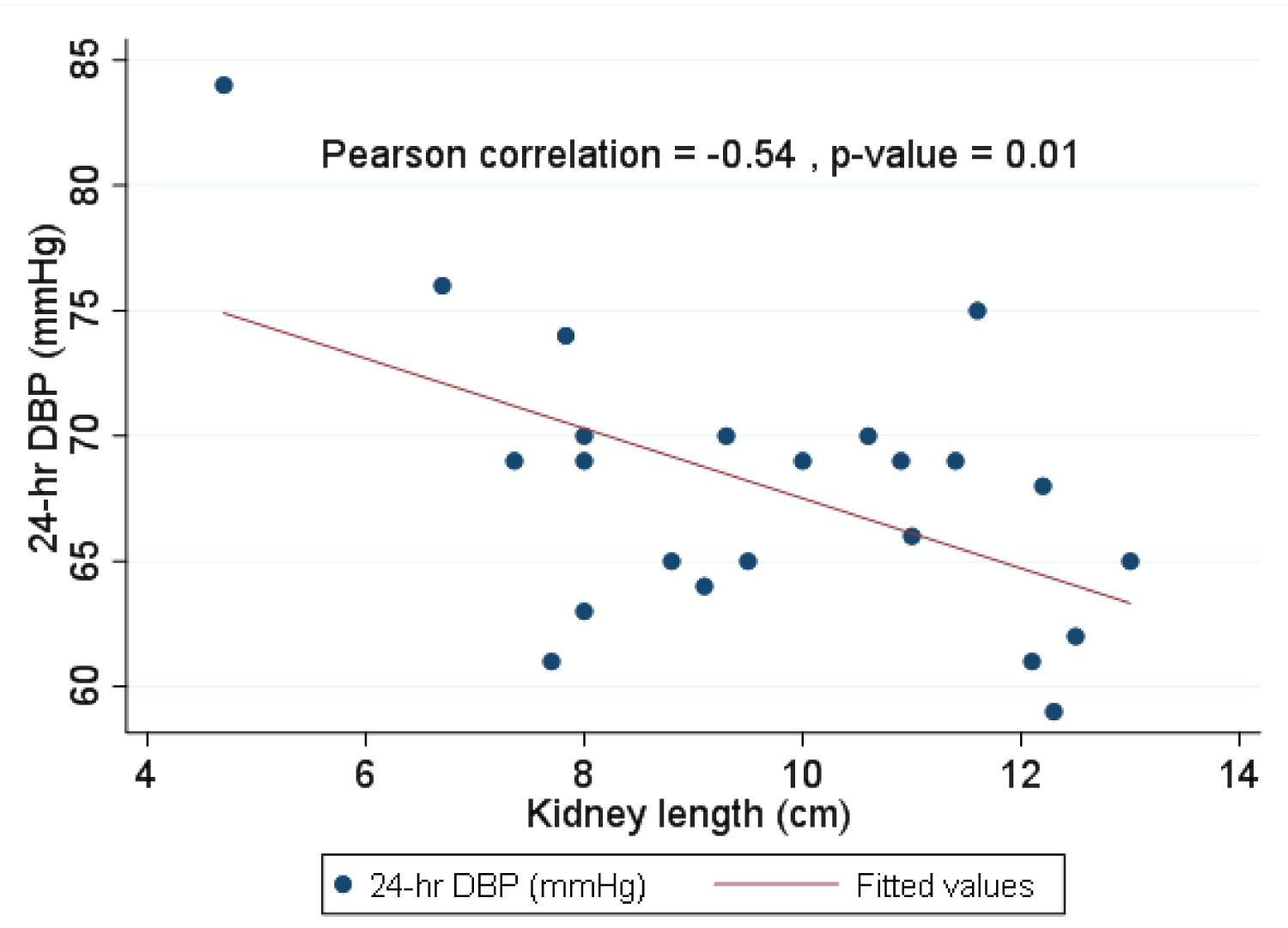 Figure 2: Pearson correlation for 24-h DBP and kidney length.
View Figure 2
Figure 2: Pearson correlation for 24-h DBP and kidney length.
View Figure 2
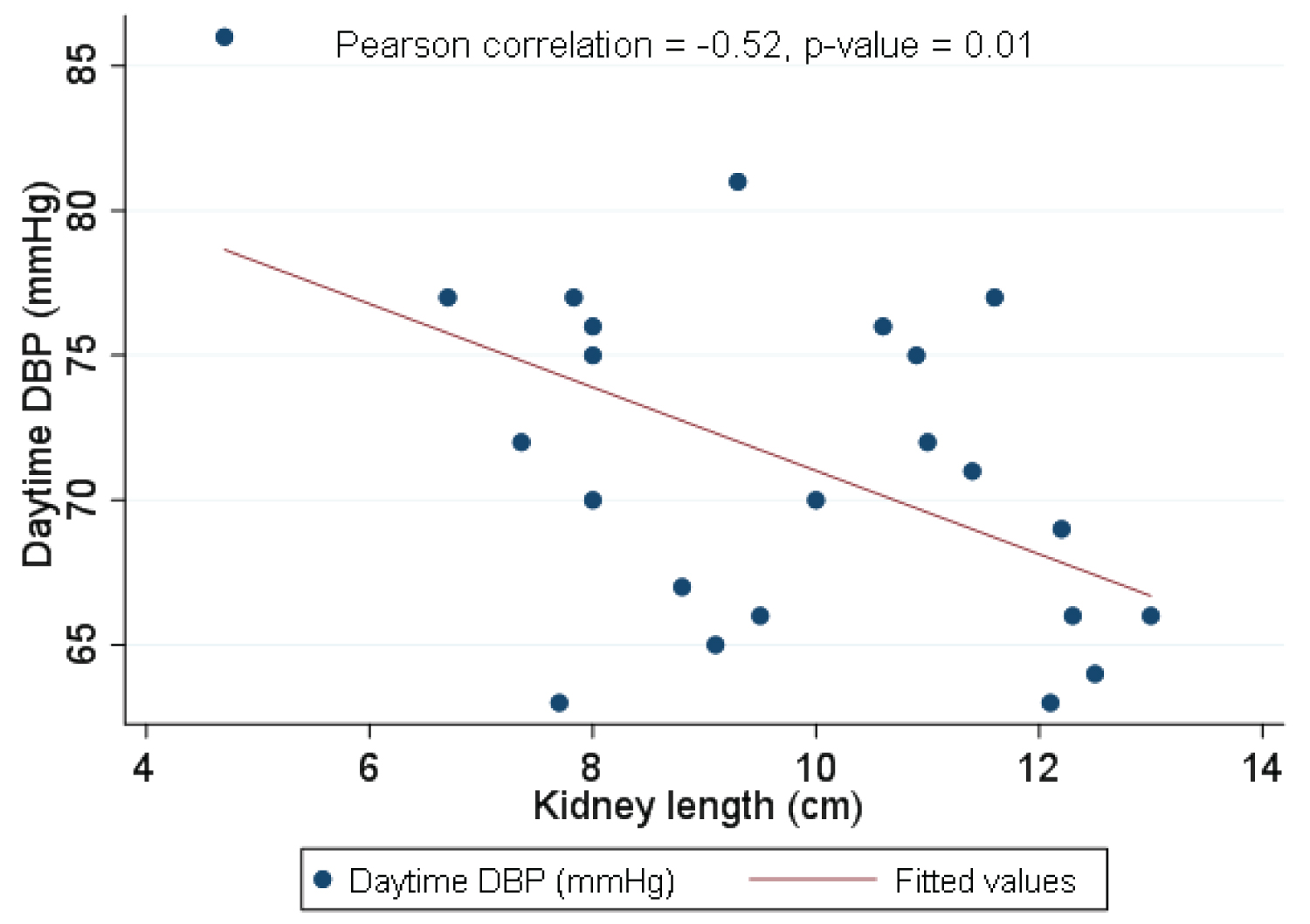 Figure 3: Pearson correlation for daytime DBP and kidney length.
View Figure 3
Figure 3: Pearson correlation for daytime DBP and kidney length.
View Figure 3
In our study, using 24-h ABPM showed that solitary kidney patients had hypertension 47.8%. Both congenital and acquired group showed higher prevalence of hypertension at 46.67% and 50%. The results supported a hypothesis of nephron under dosing that reduction in renal mass associated with hypertension, even though the renal mass reduction occurs later in life [18]. Solitary kidney patients were diagnosed with hypertension more often when comparing ABPM to OBP measurement (47.83% and 26.09% respectively). Among 11 hypertensive patients in ABPM group, 7 patients (63.6%) are not diagnosed as hypertension by OBP. This group of patients are called masked hypertension. This finding showed a possibly significant role of ABPM in unmasking hypertension in solitary kidney patients [19].
Obesity is known to be a major risk factor for hypertension and other co-morbidities. This study showed that obesity patients have significantly higher SBP load than non-obesity. BP load reflects the proportion of BP that is higher than normal value and could be associated with higher end-organ damage [20].
Previous study demonstrated an association of non-dipping BP profile and target organ damages [21]. In this current study only showed significant higher of nighttime SBP and DBP between non-dippers and dippers but did not demonstrate a difference in mean 24-h BP. A further study is needed to evaluate the dipping status and severity of cardiovascular abnormalities.
The Pearson correlation showed the inverse correlation between kidney length and DBP (24-h and daytime). However, the causal effect of compensatory hypertrophy and hypertension cannot be demonstrate in this study. It could be inversely associated because compensatory hypertrophy of the remaining kidney implies that there are compensatory processes for a low nephron number [22]. Insufficient compensatory renal hypertrophy is an important risk factor for renal dysfunction. The utility of renal hypertrophy to predict the developing of hypertension is needed further investigations.
In congenital and acquired subgroup, no significant difference in BP profile was found. However, there were some limitations in this current study. First, the sample size was small due to the COVID-19 situation in the hospital. Some of the appointment had been postponed or cancelled. Second, this study was designed as a cross-sectional study so the timing of developing hypertension could not be determined. It might take time to develop hypertension in acquired solitary kidney group. Third, the correlation between kidney length and hypertension might be inaccurate because the normal kidney's size vary by patients' age.
Our study demonstrated that prevalence of hypertension in children with solitary kidney is high. 24-h ABPM is better than OBP to detect hypertension. Using 24-h ABPM has a role in unmasking hypertension. Implementing the use of 24-h ABPM in high risk group patients in out-patient settings could help physician detect hypertension earlier.
The authors would like to thank all solitary kidney patients and their families for participating in this study, and Nuanpan Siripen from pediatric nephrology unit for her assisting in collecting the data.
The authors report no conflict of interest.