A Matter of Balance (MOB) is a national community-based fall prevention program focusing on cognitive restructuring to manage concerns about falling, though does not include a balance-training component. A dual-task balance challenge (DTBC) comprising weight transfer using fixed and random ordering of ankle-reaching balance tasks was added to MOB, to determine if this would lead to reduced fall risk. The study aims were to assess acceptance, satisfaction, safety and adherence to the interventions, examine changes in fall risk, and monitor incident falls for 3-months post-intervention.
A single-blind, two-group, randomized pilot study with community-dwelling older adults assigned to MOB (2-hours, twice/week for 4 weeks) with 15 minutes of social time or MOB plus DTBC (15 minutes of fixed and random ordering of ankle-reaching balance tasks). Acceptability and satisfaction obtained by self-report, safety and adherence monitored during class by study staff. Fall risk included objectively assessed balance and gait (LEGSys™, BioSensics, LLC), and fear of falling (Falls Efficacy Scale International). Monthly fall calendars with phone follow-ups for incident falls.
At high fall risk older adults (n = 16, mean age = 74 ± 8 years), mainly retired (95%), women (88%), with > 13 years education (81%), completed the study (drop-outs, n = 1). Acceptability and satisfaction (mean score = 9.0 ± 1.3, 1 = least, 10 = most) were high, no safety issues, and very high adherence rates (> 94%), regardless of group assignment. The MOB group (n = 7) had no within group changes in fall risk post-intervention (p > 0.05). Conversely, the MOB plus DTBC group (n = 9) had significant improvements in balance (p < 0.05) and gait (p < 0.05) with less fear of falling (p = 0.04) post-intervention, when compared to baseline.
Reducing fall risk factors and preventing falls are essential for older adults, to ensure that they continue to live safely and independently. The addition of DTBC to the nationally-used MOB curriculum may enhance both balance and gait, and lead to reduced fall risk.
Accidental fall, Fall prevention, Fall risk, Older adults
AP: Anterior/Posterior; AzAHEC: Arizona Area Health Education Centers; COM: center of mass; DTBC: Dual-Task Balance Challenge; EC: Eyes-Closed; El Rio: El Rio Community Health Center; EO: Eyes-Open; FES-I: Falls Efficacy Scale International; LEGSys: Locomotion Evaluation and Gait System; ML: Mediolateral; MMSE: Mini-Mental Status Exam; MOB: Matter of Balance; PHQ-9: Patient Health Questionnaire
Fall injuries are responsible for significant health care utilization, disability, loss of independence, and high costs among community-dwelling older adults [1,2]. Impaired postural control (balance) is one of the major risk factors for falling, and methods to improve balance can be integrated into existing fall prevention programs. Fall prevention interventions among community-dwelling older adults are essential [3]. A Matter of Balance (MOB) [4,5] is one of the most commonly used community-based fall prevention interventions nationally, and is considered the 'fall prevention standard of care'. MOB programs are targeted to reduce the fear of falling and promote physical activity among all older community-dwelling adults. Despite its name, MOB focuses on cognitive restructuring to manage concerns about falling and does not include a balance-training component. While evidence indicates that the MOB program leads to small, sustained decreases in older adults' perceived fear of falling, [5,6] there is no evidence of improvement measured by objective balance and gait tests. Among community-dwelling older adults, intact balance and concomitant attention ("dual-tasking") are essential to prevent falls, and dual-task balance training components are now a requisite according to evidence-based fall prevention intervention guidelines [7-9].
This single-blind, two-group, randomized pilot study was conducted at a nonprofit Community Health Center, between September 2017 and January 2018.
Community-dwelling older adults from all sex/gender and racial/ethnic groups, aged ≥ 60 years, at high fall risk (Fall Risk Questionnaire score > 4), [14] and living in the greater Tucson, AZ area were invited to participate. Older adults who were currently attending MOB or other fall prevention classes (e.g. Fall Proof), having a severe mobility disorder (e.g., unable to walk 15 feet with an assistive device), or having a severe visual or hearing impairment were excluded. Further, non-English speaking adults, those with a lack of decision-making capacity, unable to provide informed consent, serious psychiatric disorder (e.g., schizophrenia), moderately-severe depression (PHQ-9 = Patient Health Questionnaire ≥ 15), [15] cognitive impairment (MMSE = Mini-Mental Status Exam ≤ 23), [16] or serious medical condition (e.g., cancer treatments) were excluded from study participation.
Study participants were recruited from an underserved population of community-dwelling older adults at high fall risk, who were partaking in services provided by El Rio Community Health Center (El Rio). Older adults interested in participating in the study contacted the study staff, who screened for eligibility using a standardized checklist, and obtained written informed consent. Approval to conduct the study was obtained from the Institutional Review Boards at the University of Arizona and El Rio in Tucson, AZ. The investigation was carried out according to the principles outlined in the Declaration of Helsinki, including written informed consent from all participants. The study was registered on ClinicalTrials.gov (Identifier: NCT03176511), National Library of Medicine (Bethseda, MD).
Following baseline assessments, participants self-selected to attend either Monday/Thursday classes or Tuesday/Friday classes to accommodate their preferences and schedules, in order to promote intervention adherence and study retention. After all participants enrolled in the study and completed baseline assessments, the study investigator "flipped a coin" to determine which class would provide the MOB or the MOB plus DTBC interventions. Participants were unaware of which study intervention they received, until the first day of class. Study outcome assessors were blind to group allocation.
All data collection and study interventions were conducted in a quiet, private room at El Rio. Trained and certified staff at El Rio provided the study interventions.
Participants that were randomly assigned to MOB attended classes, used the course materials developed by Maine Health's Partnering for Healthy Aging (https://mainehealth.org/healthy-communities/healthy-aging/matter-of-balance). MOB is a structured group-based fall prevention education course specifically designed for older adults, and uses cognitive restructuring to manage concerns about falling [4-6]. During the MOB classes, a variety of strategies are used, such as restructuring misconceptions to promote a view of fall risk and fear of falling as controllable, setting realistic goals for increasing activity, changing the environment to reduce fall risk, and learning range of motion exercises to aid in fall prevention [4]. Classes were held twice a week for 4 weeks, with 2-hour sessions, as is routine. An additional 15 minutes of social time followed each class, to provide equivalent time and attention, accounting for the 15-min DTBC training provided in the other intervention. Pima Council on Aging (https://www.pcoa.org) provides educational programs each year, including MOB, and provided two experienced and certified MOB instructors for this study.
In addition to MOB described above, participants that were randomly assigned to MOB plus DTBC received a 15-min DTBC intervention each class, i.e., ankle-reaching balance tasks using either their right to left foot to tap differently colored 9-inch round vinyl markers. Three colored markers (e.g., green, blue, red) were placed on the ground in an arc, with the fourth maker (e.g., yellow) placed a neutral position behind the arc (Figure 1). A chair can be placed in front of the color pattern, as needed for safety. To enhance balance, participants stand with both feet in the neutral position 12 inches behind the pattern, and then perform an ankle-reaching balance task to the colors in the pattern by tapping a foot to the color and then tapping back to neutral (center position); first using a fixed order (green, blue, red) beginning left-to-right each time; then done in reverse order. Cognitively challenging ordering of tasks were then added by calling out randomly selected colors to increase difficulty. This was performed for 15 minutes during each class period. El Rio provided two experienced and certified MOB instructors, with additional training in providing the DTBC intervention, for this study.
 Figure 1: Dual-task balance challenge set-up (photo used with permission). View Figure 1
Figure 1: Dual-task balance challenge set-up (photo used with permission). View Figure 1
Immediately post-intervention, participants completed a short survey on the acceptability and satisfaction with the interventions [17]. On a scale from 1 to 10, participants were asked to rate their level of intervention acceptability (1 = least acceptable, 10 = most acceptable) and satisfaction (1 = least satisfied, 10 = most satisfied). In addition, they provided yes/no responses to six questions pertaining to classes being offered at a convenient time, difficulty following the instructor, gaining any personal benefit, if their health got better or worse, and if they would recommend the interventions to others. Study staff were present at all classes to monitor participants' safety and were instructed to report any adverse events. In addition, intervention adherence rates were monitored, with study staff recording class attendance.
Balance was assessed using LEGSys™ (Locomotion Evaluation and Gait System, BioSensics LLC), a wearable sensor [18]. This system uses five sensors attached to right and left anterior shins, right and left anterior thighs, and to the posterior lower back. Each sensor includes a triaxial accelerometer, magnetometer, and gyroscope (sample frequency 100 Hz), to estimate three-dimensional angles of the hip and ankle joints. A two-link inverted-pendulum model calculates the center of mass from mediolateral (ML) and anterior/posterior (AP) angles of legs (lower link-ankle rotation) and upper-body (upper link-hip rotation) and participants' anthropometric data. Balance measures assessed included changes in sway of ankle, hip, and center of mass (COM) in both ML and AP directions while standing, with feet parallel and in semi-tandem positions, during eyes-open (EO) and eyes-closed (EC) conditions (30 seconds/test) [11,19].
Gait was assessed over a distance of 20 meters using the LEGSys™ wearable sensors. The system estimates spatiotemporal gait parameters based on the participant's height (used to estimate leg length) and a two-link inverse pendulum model described above, including: velocity, stride length, stride time, double support, single support, and stride-to-stride variability, and gait initiation [19,20]. COM range of motion during walking was calculated based on the data from the sensor attached to the lower back. Gait was assessed under usual and maximal walking speeds [19].
Fear of Falling was defined as concerns about falling. The Falls Efficacy Scale International (FES-I) scale was used, a self-report measure that assesses concerns about falling for 16 commonly performed activities at home and in community settings (e.g. get in/out of chair, walk in crowded places) [12,21].
3-month incident fall rates: Participants were provided with monthly fall calendars and asked to mark it daily (X = no fall, F = Fall) and record details of any fall injury/hospitalization on the back of the monthly sheet [13,22]. A fall was defined as: an unexpected event in which the person comes to rest on the ground, floor, or lower level [23]. Participants were provided with pre-paid, self-addressed envelopes to return the fall calendars to the study staff each month. Reminder phone calls to participants were instituted for late or missing fall calendars [13,22].
Descriptive statistics were calculated for all variables, including range-checking and inspection of missing values. To determine participants' intervention acceptability, satisfaction, adherence and safety (adverse events), t-tests for continuous variables and Fisher's exact test for categorical variables were used. The sample size in this pilot study limited the statistical power and it was not possible to detect any significant differences in fall risk factors between groups. To compare changes in balance, gait and fear of falling from pre- to post-intervention within each group, we used paired t-tests. The number of falls and fallers in the 3-month post-intervention period were recorded as frequencies and percentages.
A total of 72 older adults were assessed for study eligibility, 28 were pre-screened, and 17 agreed to participate, providing a response rate of 24%. The flow of participants in the study including enrollment, group allocation, follow up, and analysis is presented in Figure 2. Participants were on average 74-years-old, mainly retired (95%, n = 16), women (88%, n = 15) with > 13 years education (81%, n = 13), who were at high fall risk (average FRQ score > 6). Participants self-reported medical history included diabetes (25%, n = 4), dyslipidemia (70%, n = 12), and hypertension (63%, n = 10). There were no statistically significant between group differences, apart from the MOB plus DTBC group having more Hispanics than the MOB group (p = 0.03) (Table 1).
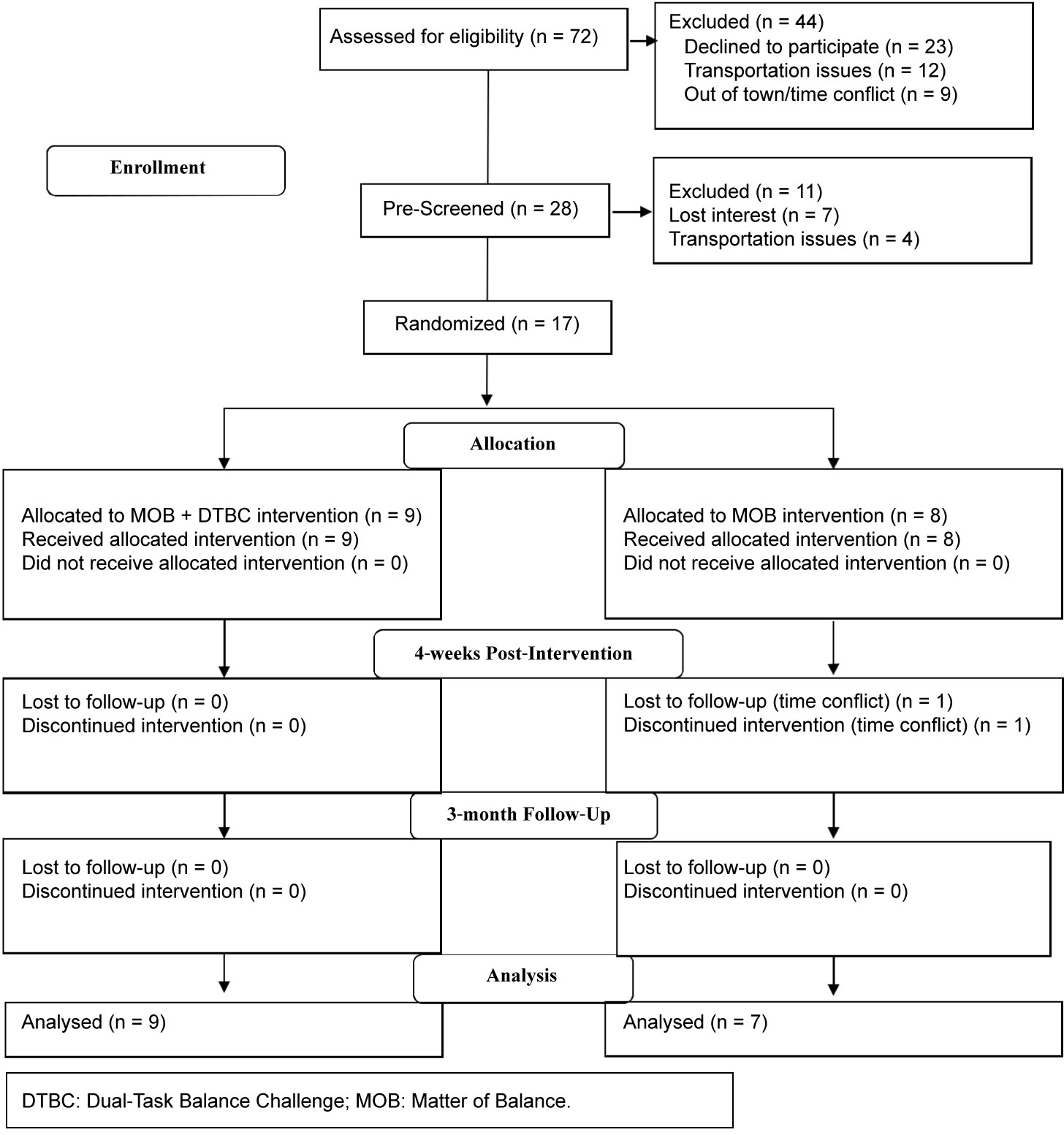 Figure 2: Fall prevention in older adults study flow diagram. View Figure 2
Figure 2: Fall prevention in older adults study flow diagram. View Figure 2
Table 1: Participant baseline characteristics. View Table 1
Participants reported that the study interventions were mostly acceptable (average score > 9) (Table 2). Similarly, participants reported that the study interventions were mostly satisfactory (average score > 9). There were no significant differences between groups in terms of the interventions' acceptability or satisfaction (all p-values > 0.20). All participants reported that the interventions were conducted at a convenient time (100%, n = 16), that they gained personal benefits, and would recommend these interventions to others (100%, n = 16). No participants reported that they had any difficulty following the instructor (0%, n = 16). There were no safety issues or adverse events during any of the classes. Participants in both groups had very high intervention adherence, attending ≥ 94% of classes (Table 2).
Table 2: Intervention acceptability, satisfaction, safety, and adherence. View Table 2
Given the statistical power in this pilot study, within group changes for the balance and gait parameters, and fear of falling were examined (Table 3). Participants in the MOB group had no significant within group changes in any of the fall risk factors post-intervention. Conversely, participants in the MOB plus DTBC group had significant improvements in balance (eyes open test = ankle sway, p = 0.02; eyes closed test = hip sway, p = 0.03 and center of mass (AP), p = 0.01) and gait (fast pace = stride time, p = 0.04 and double support, p = 0.02), with less fear of falling (p = 0.04) after the 4-week intervention (Table 3). While the MOB plus DTBC had a 23% reduction in fear of falling, the MOB group had only 4% reduction. Compared to the MOB group, there were more 3-month incident falls and fallers in the MOB plus DTBC group. Fall injuries were reported as either none (n = 3) or minor (n = 7), not requiring medical assistance. The reported reasons for falling were: rapid ambulation, reaching, slipping, and tripping (Table 4).
Table 3: Intervention effects on fall risk factors, within group changes. View Table 3
Table 4: Incident falls 3-months post-intervention. View Table 4
This was the first study, to our knowledge, to integrate a DTBC with the nationally-used MOB program curriculum. Community-dwelling older adults in this pilot study reported high levels of acceptability and satisfaction of the interventions, there were no safety issues, and participants had very high adherence rates, regardless of group assignment. In this pilot study, participants in the MOB plus DTBC group had significant improvements in balance and gait, with less fear of falling post-intervention, when compared to baseline. Our findings are similar to other dual-task intervention studies conducted among older adults, reporting improvements in balance, [24,25] gait, [24,26,27] and less fear of falling [27]. Balance improvements among the participants in the MOB plus DTBC group indicated they had a better ability to maintain their balance as their body moved and swayed while standing in a neutral position, with their eyes open (ankle sway) and eyes closed (hip sway and anteroposterior center of mass). While the improvements in gait at a fast pace indicated a faster stride time (i.e. time between two footsteps for the same foot), and velocity (i.e. how fast waked a specified distance) and less double support. A reduction in double support while walking indicated that participants did less "shuffling" on both feet between steps, and likely felt more stable when walking. The MOB plus DTBC participants reported a 23% reduction in fear of falling, after the intervention.
Participants in the MOB group in this pilot study had no significant within group changes in balance, gait, or fear of falling. These findings are in contrast to other MOB intervention studies reporting significant improvements in balance, [28] gait, [29] and fear of falling [5] post-intervention. In this pilot study, static balance was assessed, whereas Chen and colleagues, [28] assessed dynamic balance, which may in part explain the differences in the findings obtained. In another study, Smith and colleagues [5] reported significant reductions in the fear of falling among older women (mean age = 76 years) following a MOB intervention. In this study, participants had high intervention adherence rates, yet only reported a 4% decrease in the fear of falling after the MOB intervention. Further, incident fall rates following a MOB intervention in prior studies have reported mixed findings, with either fewer incident falls [5,28] or no change in fall rates [29]. In this pilot study, there was one recurrent faller in both the MOB and the MOB plus DTBC groups. The most common reason for falling was due to tripping, suggesting that home safety assessments may be needed in addition to the fall prevention classes [1].
This study had several strengths. First, both interventions used the standardized MOB curriculum, which is nationally recognized and aimed at preventing falls among older adults living in the community. There were two certified and trained instructors at each class, and there were different instructors teaching the MOB and MOB plus DTBC classes. Finally, balance and gait were assessed objectively using wearable sensors, providing more precise measurements of these fall risk indicators. Study limitations included the sample size, which limited the statistical power, and it was not possible to detect any significant differences in fall risk factors or incident falls between groups. In addition, participants were recruited from one Community Health Center, limiting generalizability.
Future studies with a larger sample size and longer follow-up period are needed, to determine the effects of MOB plus DTBC compared to MOB only on fall risk factors and incident fall rates. Future studies may like to consider comparing different types of DTBC activities that community-dwelling older adults enjoy and are likely to engage in, such as dancing or Tai Chi; as these types of activities require thinking and moving simultaneously.
Reducing fall risk factors and preventing falls are essential for community-dwelling older adults, to ensure that they continue to live safely and independently. Community-based programs that raise awareness about falls, help older adults to increase their strength and balance, and address the fear of falling are the most effective. The addition of DTBC to the nationally-used standard MOB curriculum may enhance both balance and cognitive function, and lead to reduced fall risk among community-dwelling older adults.
Special thanks to the study participants, study staff (Caroline Sutherland Mills, Coco Tirambulo, and Emily Taylor), the MOB Instructors (Tom Pylman and Barbara Benesch), the MOB plus DTBC Instructors (Shelley Whitlatch and Nancy Schulte), Pima Council on Aging, and El Rio Community Health Center.
This study was funded by a grant from the Arizona Area Health Education Centers (AzAHEC) Program (grant number: RG 2017-13, Taylor-Piliae, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of AzAHEC.
The authors declare no conflicts of interest.