In March 2020, New York City encountered its first official case of COVID-19 (coronavirus disease 2019). This novel coronavirus, referred to as SARS-COV 2, originated in Wuhan, China in December 2019. Within a short amount of time, hundreds of thousands of cases were diagnosed around the world and the United States, causing the World Health Organization to announce it as an official infectious disease pandemic on January 30, 2020.
COVID-19 is spread by respiratory droplets, and healthcare professionals are mandated to wear personal protective equipment (PPE) for a prolonged period of time when caring for COVID-19 patients.
Healthcare professionals report side effects of prolonged use of PPE when caring for COVID-19 patients. This study delves into various adverse effects of prolonged mask use and provides recommendations to ease the burden on healthcare professionals.
This is a cross sectional study among healthcare professionals, primarily located in New York City, who worked in the hospital during the COVID-19 pandemic. All respondents completed an anonymous survey consisting of twenty one questions regarding adverse effects of PPE, medical history, and demographics.
A total of 343 healthcare professionals on the COVID-19 front lines participated in this study. The majority were female (n = 315) and 227 were located in New York City. 225 respondents identified as White, 34 as Hispanic, 23 as African American, and 61 as "other" ethnicity. 314 respondents reported adverse effects from prolonged mask use with headaches being the most common complaint (n = 245). Skin breakdown was experienced by 175 respondents, and acne was reported in 182 respondents. Impaired cognition was reported in 81 respondents. Previous history of headaches (n = 98), skin sensitivity (n = 164), and acne (n = 121) were found in some respondents. Some respondents experienced resolved side effects once masks were removed, while others required physical or medical intervention.
Prolonged use of N95 and surgical masks by healthcare professionals during COVID-19 has caused adverse effects such as headaches, rash, acne, skin breakdown, and impaired cognition in the majority of those surveyed. As a second wave of COVID-19 is expected, and in preparation for future pandemics, it is imperative to identify solutions to manage these adverse effects. Frequent breaks, improved hydration and rest, skin care, and potentially newly designed comfortable masks are recommendations for future management of adverse effects related to prolonged mask use.
Surgical mask, N95 mask, PPE, COVID-19, Coronavirus, Virus, Pandemic
In March 2020, New York State encountered its first official case of COVID-19. This novel coronavirus, referred to as SARS-COV 2, originated in Wuhan, China in December 2019. Within a short amount of time, hundreds of thousands of cases were diagnosed around the world, causing the World Health Organization to announce it as an infectious disease pandemic on January 30, 2020. New York City quickly became the epicenter of the United States COVID-19 pandemic due to its tremendous number of cases.
COVID-19 is spread by respiratory droplets, and healthcare professionals are mandated to wear PPE when caring for COVID-19 patients. PPE includes gowns, gloves, masks, and face shields. Aside from a major shortage of PPE across the United States causing stress to hospital administrators and healthcare professionals on the front lines, many expressed added stress from adverse effects of prolonged PPE usage.
The last incidence of prolonged use of PPE among healthcare professionals was during the SARS (severe acute respiratory syndrome) outbreak in 2003-2004 which originated in Guangdong, China. Studies focusing on effects of prolonged use of PPE during the SARS outbreak were published in subsequent years. A study by Lim, et al. focused on headaches related to mask use [1], and another study by Foo, et al. discussed adverse skin reactions such as rashes, acne, and itching from mask use [2].
The CDC and WHO recommend wearing N95 masks during care of patients with highly transmissible diseases such as tuberculosis, SARS, and COVID-19. The N in N95 stands for NIOSH, the National Institute for Occupational Safety and Health of the United States and 95 indicates filter efficiency of particles. Thus, an N95 mask is 95% effective at filtering airborne particles including very small ones. In comparison, while surgical masks provide a barrier against large respiratory particles, they are ineffective at providing protection from smaller particles. Surgical masks also do not prevent leakage around the mask when the user inhales. Therefore, surgical masks are ineffective and do not provide enough protection when performing direct care for patients with COVID-19 [3].
To prevent the spread of COVID-19, hospitals required their employees and visitors to wear a mask at all times when in the facility. Generally, employees and visitors wore surgical masks, and when providing direct care for COVID-19 patients, the employees donned N95 masks.
Wearing masks for a prolonged amount of time causes a host of physiologic and psychologic burdens and can decrease work efficiency. Activity cannot be performed as long or as efficiently while wearing masks as compared to when masks are not worn. Additionally, the timeframe that an activity can be sustained is decreased when wearing masks and PPE [4]. Prolonged use of N95 and surgical masks causes physical adverse effects such as headaches, difficulty breathing, acne, skin breakdown, rashes, and impaired cognition. It also interferes with vision, communication, and thermal equilibrium.
Headaches related to prolonged mask use can be attributed to mechanical factors, hypercapnia, and hypoxemia. Tight straps and pressure on superficial facial and cervical nerves are mechanical features causing headaches [1]. Cervical neck strain from donning PPE, sleep deprivation, irregular mealtimes, and emotional stress are other sources of headaches among healthcare professionals during prolonged mask use [5]. Tight fitting masks cause inadequate ventilation and increased levels of carbon dioxide (CO2) known as hypercapnia. As CO2 is a known respiratory stimulant, a buildup of exhaled CO2 between the mask and face will cause increased lung ventilation and respiratory activity. Symptoms of hypoxemia such as chest discomfort and tachypnea are also noted in healthcare professionals with prolonged mask use. Exhaled CO2 builds up between the mask and face, and increased levels of CO2 cause confusion, impaired cognition, and disorientation [4].
A hot and humid environment found in the facial region covered by masks, causes discomfort and hyperthermia. This may create a situation where the healthcare professional is unable to recognize dangers and perform manual tasks, and it also significantly affects motor skills [4]. The moist environment and pressure from tight fitting masks also block facial ducts. This can explain the increase of acne with prolonged mask use [2].
Frequent PPE and mask changes may cause shearing and breakdown of the skin, and breakdown on the bridge of the nose and cheek bones can be attributed to tight fitting masks and goggles that put pressure on these specific areas [6].
Urticaria and contact dermatitis can occur from sensitivity to components of masks and PPE. Formaldehyde is a chemical used in PPE that some are sensitive and/or allergic to. Others may react to thiuram which is found in the ear loops of surgical masks [7].
This anonymous, twenty-one question survey was distributed electronically at the beginning of May 2020 to healthcare professionals on the front lines of the COVID-19 pandemic. The majority of survey respondents were females (91.8%, n = 315) and were located in New York City (66.2%, n = 227). 9.3% (n = 32) were located in New York State (outside New York City), 7.3% (n = 25) in New Jersey, and the remaining 17.2% (n = 59) outside these two states. About half of the respondents work at New York Presbyterian Hospital (47.8%, n = 164). 65.6% (n = 225) identified as White, 9.9% (n = 34) as Hispanic, 6.7% (n = 23) as African American, and 17.8% (n = 61) as other ethnicities. Age of respondents ranged from 20 to 50+ years of age. 31.7% (n = 108) were ages 20-29, 38.1% (n = 130) ages 30-39, 15.5% (n = 53) ages 40-49, and 14.7% (n = 50) 50 years and older.
Of the 343 participants of this survey, 59.2% (n = 203) primarily wear a N95 mask and 40.8% (n = 140) wear a surgical mask throughout their shift. Reported side effects include headache, acne, skin breakdown, and impaired cognition. The majority of respondents (91.5%, n = 314) report one or more of these adverse effects while 8.5% (n = 29) report none of these adverse effects (Figure 1). Some found specific brands such as 3M, Kimberly Clark, Halyard, Medline, and Argaman causing these side effects while others reported no difference from one brand to another.
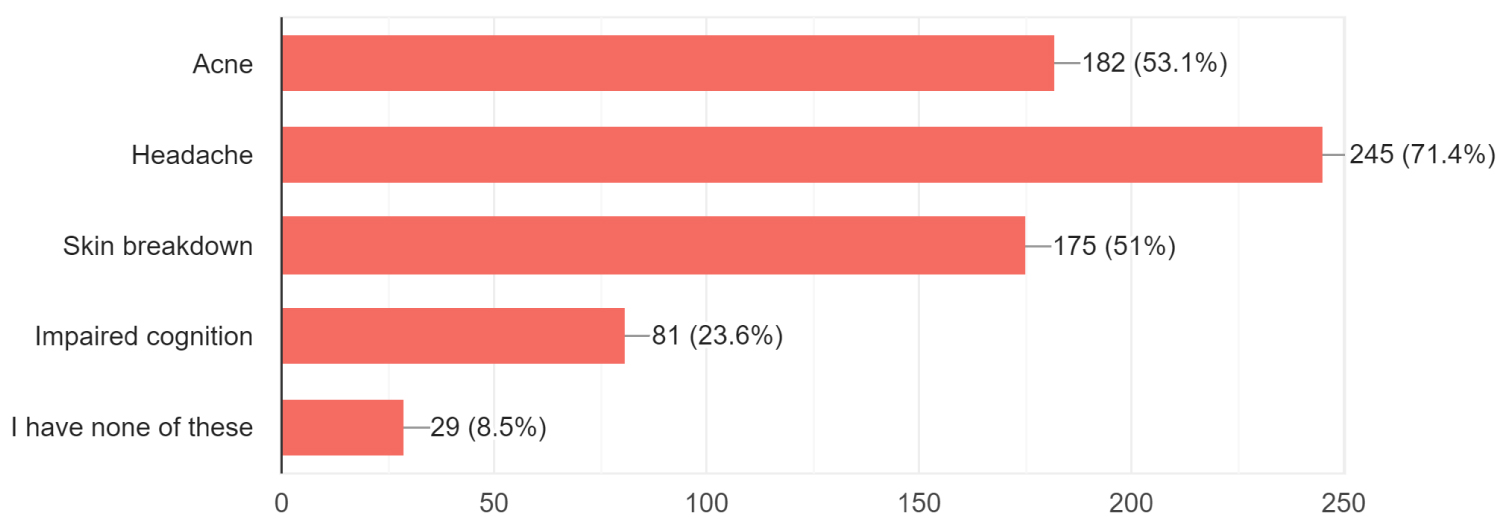 Figure 1: Adverse effects after wearing a mask for a full shift.
View Figure 1
Figure 1: Adverse effects after wearing a mask for a full shift.
View Figure 1
The highest reported side effect was headaches with 71.4% respondents (n = 245) reporting this adverse effect. 15.2% (n = 52) stated their headaches occured within 1 hour of wearing the mask, 30.6% (n = 105) after 1 hour of wearing the mask, and 29.7% (n = 102) after 3 hours or more of wearing the mask. 24.5% (n = 84) reported no headaches at all from prolonged mask use (Figure 2). The majority of survey respondents (71.4%, n = 245) have no prior history of headaches.
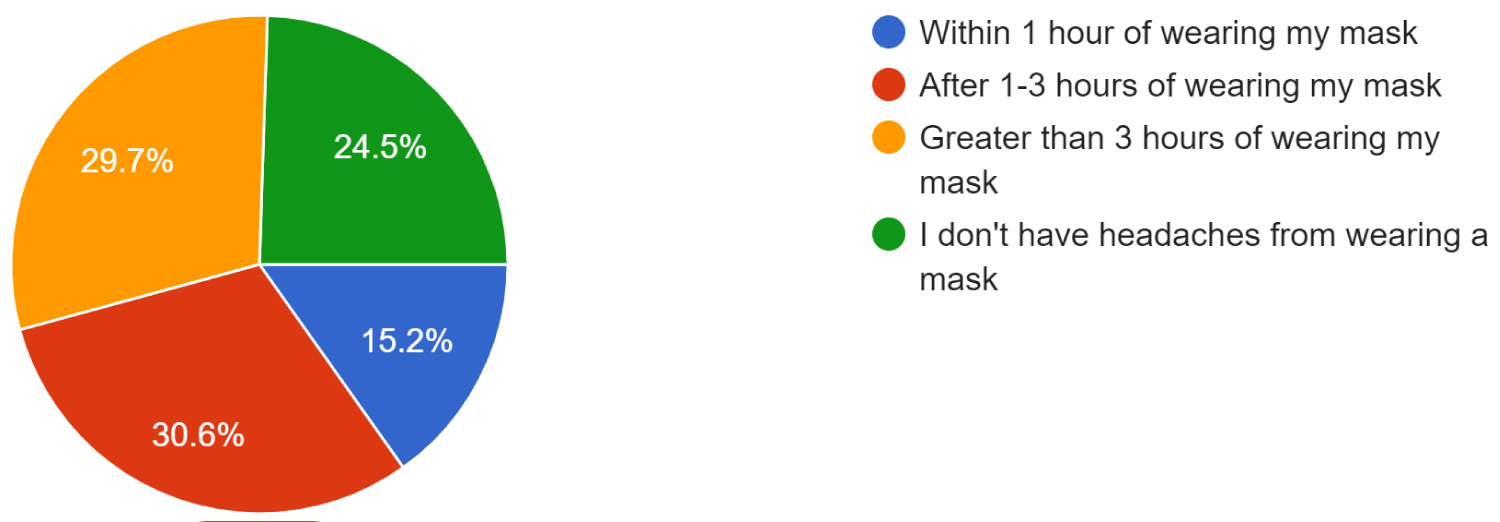 Figure 2: After how many hours of wearing a mask does the survey respondent experience a headache.
View Figure 2
Figure 2: After how many hours of wearing a mask does the survey respondent experience a headache.
View Figure 2
After removing the mask, headaches resolved in 14% of respondents (n = 48) within 30 minutes, 33.8% (n = 116) after 1 hour, while 28% (n = 96) needed medication for treatment to resolve the headache. Medications such as tylenol, motrin, and NSAIDs were used for those who needed medication to resolve their headache.
Prior history of sensitive skin was reported in 47.8% (n = 164) of respondents. 51% of survey respondents (n = 175) reported skin breakdown as an adverse effect of prolonged mask use (Figure 3).
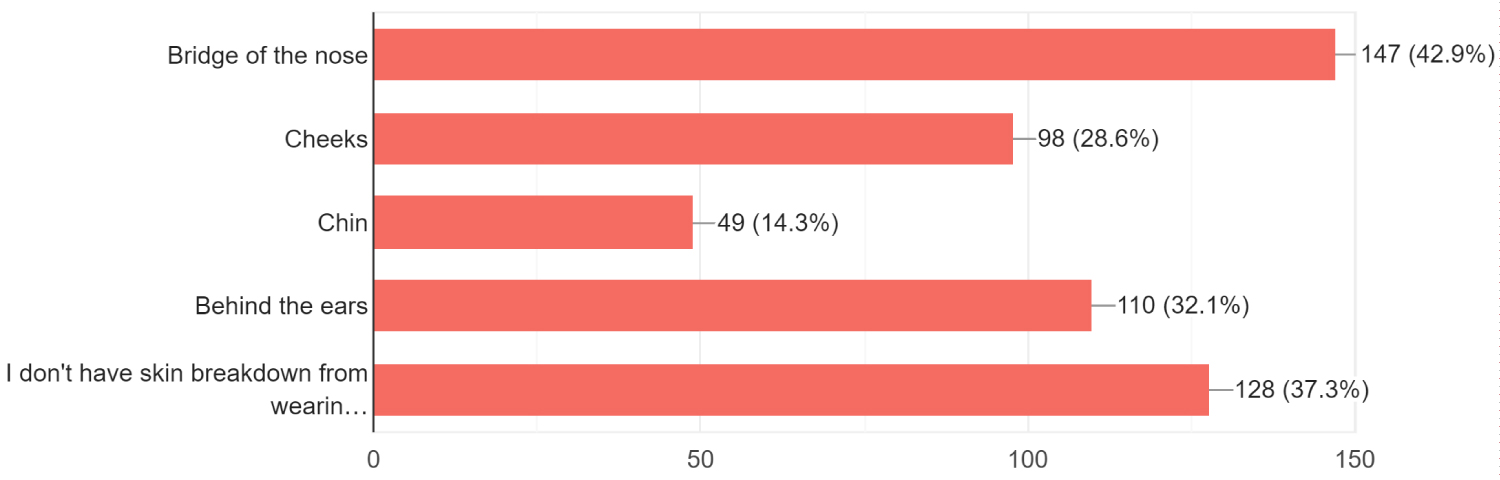 Figure 3: Locations of skin breakdown from wearing a mask.
View Figure 3
Figure 3: Locations of skin breakdown from wearing a mask.
View Figure 3
18.1% (n = 62) reported skin breakdown within 1-3 hours of mask use and 44% (n = 151) after 3 hours or more of mask use. For those who had skin breakdown, the most common area was the bridge of the nose (42.9%, n = 147) and cheeks (28.6%, n = 98). Other areas of skin breakdown are chin (14.3%, n = 49) and behind the ears (32.1%, n = 110). To alleviate skin breakdown, 35.6% (n = 122) used lotions or creams such as bacitracin, aquaphor, Kiehl's, aloe, Cetaphil, aloe, shea butter, Jergens, skin prep, and cavalon. 8.7% (n = 30) used dressings such as mepilex, duoderm, and band aid.
Acne accounted for 53.1% (n = 182) of participants with 11.1% (n = 38) reporting acne within 1-3 hours of mask use and 47.8% (n = 164) after 3 hours of mask use. A history of acne was reported in 35.3% (n = 121) of the respondents while the others reported no history of acne.
Impaired cognition was the least reported adverse effect with 23.6% (n = 81) reporting impaired cognition from prolonged mask use. Of those who experienced this side effect, 2.9% (n = 10) were cognitively impaired within 1 hour of mask use, 9% (n = 31) within 1-3 hours of mask use, and 16.6% (n = 57) after 4 hours of mask use.
A profound number of healthcare professionals who participated in this survey reported adverse reactions to prolonged mask use during COVID-19. Headaches, skin breakdown, acne, and impaired cognition were all recognized as common adverse effects. As we are still amidst the pandemic, and second waves are predicted in the future, tips and recommendations for enduring prolonged mask use are vital for the health and comfort of healthcare professionals.
Recommendations have previously been addressed in the literature. The first is frequent work breaks to be incorporated into work shifts to allow for shorter duration of mask use and reduction of PPE exposure [1,8]. A second recommendation is preventative measures such as applying moisturizers, emollients, and barrier creams to prevent skin breakdown [9]. Caution should be taken that dressings, moisturizers, and lotions do not interfere with the seal of the mask thereby causing decreased protection against COVID-19 particles. A third recommendation is improved mask design with a focus on safety, comfort, and tolerability [4].
To prevent headaches and impaired cognition, survey respondents recommend frequent short breaks, neck massage, increased hydration especially before start of the shift, alternating between surgical and N95 masks (if possible), wearing an N95 mask with a filter to allow for better ventilation, and wearing a mask that fits one's face best.
To manage acne, survey respondents recommend moisturizing skin and lips before and after shifts, avoiding facial makeup, and using facial cleanser wipes throughout the shift to cleanse the skin. Lastly, to prevent skin breakdown, survey respondents recommend using an ear saver, paper clip, or a headband with buttons to allow ear straps to rest on these items instead of behind the ears. The use of tegaderm, tape, or a dressing on the bridge of the nose, and using a clean, fresh mask for each shift are also recommended by the survey respondents to address skin breakdown.
While this survey captured the experiences of many health care professionals working on the front lines during COVID-19, there are some limitations to this study. First, preexisting conditions such as high BMI, asthma, and other conditions were not assessed in this survey, and these could be impacting or increasing the adverse effects addressed in this survey. Second, issues such as stress level and quality sleep were also not included in this survey, and these important factors could also attribute to adverse effects in the survey respondents.
This study identified various adverse effects of prolonged mask use experienced by healthcare professionals during the COVID-19 pandemic. While healthcare professionals and the world at large wish this pandemic to end, and never return, various recommendations are presented for future prevention and management of these adverse effects.
The author declares no conflict of interest.
I would like to thank all the anonymous healthcare professionals who participated in this survey. This data will be crucial for the current COVID-19 pandemic as well as future outbreaks involving prolonged use of masks and PPE among healthcare professionals.
No funding was received for this survey.