Disordered cognition, commonly but inaccurately referred to as "psychosis", is a challenging symptom to evaluate and manage in the critical care or emergency department setting. Although exacerbation of a primary psychiatric disorder may indeed be associated with psychosis, a large number of medical illnesses may present similarly. Often, there is no single test to establish a definitive diagnosis. As history is usually limited in critically ill patients, a wide differential diagnosis may be the most important tool utilized by the clinician. In addition, the presence of multiple comorbidities not only makes a medical cause more likely but also complicates subsequent management. Although the use of antipsychotics may prove successful in addressing symptoms, failure to treat the underlying medical cause may lead to increased morbidity and mortality. Incorporating a wide differential diagnosis, establishing the primary cause, and intervening in a goal-oriented manner are the keys to successful management of critical care psychosis.
Psychiatric complaints are not just limited to the psychiatry ward, but are commonly encountered in the emergency department. Psychosis in critical care settings is usually not a disease in and of itself, but rather is usually diagnostic of delirium [1]. The incidence of delirium has been reported as high as 80% in critically ill patients [2].
Given the high prevalence of delirium, it is important for the emergency department physician to recognize the numerous medical diseases that may present with psychiatric overtones. The presence of psychosis often creates a substantial diagnostic challenge, as misdiagnosis of delirium is associated with longer lengths of stay and higher mortality [1,2]. In addition, treatment for mental status changes due to a medical condition is often quite different than treatment of a primary psychiatric disorder.
This paper will discuss three medical mimics of psychiatric illness that may prove diagnostically challenging to the clinician: Alcohol withdrawal syndrome, anti-NMDA-receptor encephalitis, and serotonin syndrome. Furthermore, this manuscript will discuss methods for diagnosis, clinical pearls, and guidelines for management of these conditions.
Alcohol remains a commonly used and abused drug worldwide, despite its association with over 200 medical conditions, including liver disease, cancer, and accidental injury. In 2012, 5.9% of global deaths were attributed to alcohol use [3]. In the United States, as many as 40% of hospitalized patients have alcohol-related medical conditions [4]. Up to 25% of admitted patients with alcohol use disorder will develop acute withdrawal, often requiring admission due to complications such as respiratory failure, delirium tremens (alcohol withdrawal delirium), infection, cirrhosis, and gastrointestinal bleeding [5,6].
The central effect of alcohol in the body is mediated through two main pathways. Gamma-aminobutyric acid (GABA) is a major inhibitory neurotransmitter that binds to GABA receptors. Ingestion of alcohol enhances the effect of GABA, although the mechanism is currently unknown [7]. Glutamate is a major excitatory neurotransmitter acting primarily through NMDA receptors; the presence of alcohol inhibits ion flux through the NMDA receptor, suppressing activity [8]. The effect of alcohol on these two pathways has a synergistic effect on the central nervous system and is responsible for the clinical manifestations of alcohol intoxication, namely, sedation and anxiolysis [9]. Long-term use of alcohol leads to upregulation of NMDA receptors and downregulation of GABA receptors to maintain equilibrium [10]. These alterations in receptor expression persist after alcohol cessation. Increased NMDA activation and loss of GABA inhibition leads to the autonomic excitation and agitation seen in alcohol withdrawal.
Alcohol withdrawal syndrome (AWS) is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) as a recent decrease in or cessation of heavy or prolonged alcohol use and the presence of at least two of the following: Autonomic dysfunction, hand tremor, insomnia, nausea or vomiting, hallucinations, anxiety, agitation, or seizures [11]. The clinical spectrum of alcohol withdrawal generally includes four stages of increasing severity; autonomic hyperactivity, hallucinations, neuronal excitation, and delirium tremens [12]. However, the progression of symptoms varies greatly between patients, often skipping milder stages before the development of severe withdrawal.
An early or mild presentation can sometimes manifest with autonomic symptoms only, including anxiety, nausea/vomiting, tremor, or diaphoresis. Generally, mild presentations do not involve alterations in sensorium [9]. Consequently, these symptoms can easily be misinterpreted as anxiety, especially if the patient minimizes their drinking history to clinicians. On the more severe end, alcoholic hallucinations may occur with alcohol withdrawal. These hallucinations are most often visual and tactile, including the sensation of insects crawling on the skin, or formication. Auditory hallucinations are less common and may point to an alternate cause [13]. Seizures associated with withdrawal are typically brief and tonic-clonic in nature, and they often occur without autonomic symptoms or hallucinations [14]. Persistent alterations in mental status in patients with a heavy alcohol-use history should never be ascribed to a primary psychiatric cause without further investigation. In these patients, diagnostic consideration should include hyperammonemia, spontaneous bacterial peritonitis secondary to underlying liver disease, beer potomania, or Wernicke's encephalopathy. Unfortunately, a noncontrast CT scan of the head in insensitive for these conditions, but can be valuable in excluding tumor or mass effect [15].
Approximately 5% of patients experiencing alcohol withdrawal in the inpatient setting will progress to delirium tremens [13]. Clinical manifestations include delirium or altered sensorium coupled with autonomic hyperactivity and often hallucinations [16]. The associated hypertension, tachycardia, and hyperventilation leads to increases in cardiac output and oxygen consumption, and subsequently, decreased cerebral blood flow [17]. This alteration in physiologic state leads to major complications, including electrolyte abnormalities, arrhythmias, pneumonia, and respiratory failure [12]. The significance of this stage is not only due to difficulties in patient care; it is also associated with a mortality rate up to 15% [18].
The treatment of alcohol withdrawal syndrome (AWS) varies widely due to its spectrum of severity. Supportive care is usually sufficient to treat mild withdrawal symptoms that are typically temporary and self-limited. Intravenous fluids and antiemetics can be used to address nausea/vomiting and dehydration. In alcohol withdrawal syndromes that are severe enough to prompt admission, benzodiazepines have long been considered the mainstay of therapy. All benzodiazepines have been shown to improve signs and symptoms of withdrawal [16]. Additionally, use of benzodiazepines contributes to a lower incidence of seizures and delirium tremens when compared with chlorpromazine, hydroxyzine, thiamine, or placebo [19]. Longer-acting agents (valium, chlordiazepoxide) may be more effective than short-acting agents in preventing alcohol withdrawal seizures and delirium tremens, but they may also pose an increased risk of oversedation [20,21].
Although there is less evidence, several additional agents have also been studied for use as adjuvant therapy for alcohol withdrawal. For benzodiazepine-resistant delirium tremens, intubation is often required, and continuous propofol infusion been utilized with some success [22,23]. Anticonvulsants, including carbamazepine and valproic acid, may raise the seizure threshold but are ineffective as single agents in management of alcohol withdrawal [24,25]. Few small studies have suggested phenobarbital is as effective as lorazepam for treatment of mild withdrawal; however, systematic reviews do not show any additional benefit over benzodiazepines [26-28]. Phenytoin and the newer antiepileptic oxcarbazepine have not been shown to be useful in preventing withdrawal seizures [29,30]. β-blockers and other adrenergic agents are often used to treat autonomic symptoms, but their utilization risks masking the severity of withdrawal and may lead to undertreatment [31]. Neuroleptic agents, including phenothiazines and haloperidol, are often used for symptom control but, similarly to adrenergic agents, may cause masking and under treatment. Also, side effects including hypotension, decreased seizure threshold, and QT-prolongation should limit their use as single-agents in withdrawal patients already at risk for those complications [19].
Though the diagnosis of AWS is largely based on history and physical exam findings, a validated assessment tool for the severity of withdrawal is often utilized during inpatient hospitalizations. The Clinical Institute Withdrawal Assessment for Alcohol (CIWA-A) is a questionnaire developed in 1981 which includes 15 sections to grade withdrawal severity; a shortened, revised scale was later developed (CIWA-Ar) which includes 10 items [32]. Utilization of the CIWA scale for symptom-driven treatment allows for lower total doses of benzodiazepines and shorter treatment duration compared to fixed-dosing [33,34].
In conclusion, alcohol withdrawal can present with psychiatric overtones. Clinicians are generally able to distinguish this from a primary psychiatric disorder due to the presence of autonomic symptoms (increased heart rate, respiratory rate, fever) and tremors. However, milder cases may be misdiagnosed as anxiety. Clinicians should carefully inquire about alcohol use history, especially if the symptoms begin within 24-48 hours of admission and if the patient has no previous history of anxiety or other mood disorder. The intensity of treatment should mirror the spectrum of clinical severity. Admission should be considered in severe or refractory cases, especially when multiple co-morbid conditions are present.
Encephalitis, or an inflammatory process involving the brain, may be more common in children with an estimated incidence of 10.5-13.8 per 100,000 in children compared to 2.2 per 100,000 in adults [35]. Though encephalitis is most commonly attributed to a viral infection, as many as 60% of cases have no identified source [36,37]. Although no precise number exists, anti-N-methyl-D-aspartate receptor (NMDA-R) encephalitis, a recently characterized autoimmune cause, may be responsible for more cases of encephalitis than common viral agents, particularly in patients less than 30 years of age [38].
First identified in 2005, anti-NMDA-R encephalitis was predominantly considered a paraneoplastic syndrome, found in previously healthy young females with an associated ovarian teratoma [39,40]. Since the first report, however, the disease has since been observed in both males and females of varying ages without associated neoplasm [41]. The disease process involves autoantibodies that bind to the NMDA receptor in the brain. Internalization of the complex ensues, leading to decreased expression of the receptor. Decreased NMDA receptor function has been attributed to some of the physical manifestations of the disease [42].
The clinical presentation of NMDA-R encephalitis is highly variable. Classically, patients experience a pattern involving two stages of illness, often preceded by a non-specific viral syndrome [43]. The first stage primarily involves psychiatric symptoms, including paranoia, hallucinations, and agitation. Isolated psychosis is rare, but if present, may be falsely attributed to a primary psychiatric disorder [44]. The disease then typically progresses to a second stage that includes catatonia, unresponsiveness, and autonomic instability. Seizures may occur and are more closely associated with anti-NMDA-R encephalitis than other causes [45]. Hypoventilation is not uncommon and may require intubation and assisted ventilation [39,46].
Initial evaluation is often limited by the patient's presentation, making definitive diagnosis difficult. Imaging studies, including CT and MRI, are of limited utility, as a majority will be normal [47]. When present, significant MRI findings include T2 hyperintensity in the cerebral and cerebellar cortex, hippocampus, frontobasal, or insular regions. MRI findings are often transient in nature [43]. Electroencephalography is often abnormal but usually reveals non-specific, generalized slowing [46,47]. Definitive diagnosis requires cerebrospinal fluid analysis with an immunoassay, as antibodies to the NMDA-R are present in most patients [43]. A lymphocytic pleocytosis in the CSF is more common early in the disease course but may normalize over time [41].
Management of anti-NMDA-R encephalitis generally involves treatment with steroids, along with IVIG or plasma exchange [43,48]. Resection of an associated tumor has been associated with improved outcome when combined with immune therapy [43]. Second-line agents include rituximab and cyclophosphamide and are typically reserved for patients with insufficient response, worsening of condition, or subsequent episodes [48]. There is little evidence regarding the effective treatment of psychiatric symptoms. Both first-generation and second-generation antipsychotics have been utilized for agitation and aggression, but they pose a theoretical risk of worsening dystonia and movement disorders [49]. Benzodiazepines, clonidine, and trazodone have been shown to improve abnormalities in sleep-wake cycle [49]. Catatonia may be treated with scheduled benzodiazepines, while electroconvulsive therapy is reserved for resistant cases [48].
Autoantibody production against the NMDA receptor is an under-recognized cause of encephalitis. The diagnosis should especially be considered in young patients with new onset hallucinations, delusions, or alterations in sensorium. CSF testing is required for diagnosis, and treatment includes immune therapy with steroids, IVIG, plasma exchange, and resection of an associated tumor, if present. Additional therapy with anti-psychotics has not been proven to be of benefit.
Despite the fact that serotonin syndrome was infamously responsible for the death of Libby Zion more than 20 years ago, the exact prevalence of serotonin syndrome remains controversial. Some studies have reported an incidence of 0.4 per 1000 cases [50]. However, these estimates may be too conservative, as mild to moderate symptoms often remain unrecognized. The true incidence is currently unknown [51].
Serotonin syndrome is a condition that predictably results from an excess of serotonin in the central nervous system [50]. Serotonin is a neurotransmitter derived from L-tryptophan that activates 5-hydroxytryptamine (5-HT) receptors in both the central and peripheral nervous system. These receptors are responsible for various physiologic effects, including mood and sexual behavior, thermoregulation, motor and vascular tone, intestinal motility, and emesis [50]. Excessive serotonergic activity is most often medication-induced, either intentionally or unintentionally. There are countless commonly prescribed serotonergic agents, including selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), and serotonin receptor (5-HT) agonists [52]. SSRIs and SNRIs are antidepressants that work by prolonging serotonin activity in the neuronal synapse; MAOIs work with similar clinical effect by prevention of intracellular serotonin breakdown [53].
Neurologic symptoms of excessive serotonin were first described in humans in 1960, when tryptophan was given to patients receiving an MAOI [54]. Serotonin syndrome was formally described in 1982 after two patients received a single dose of clomipramine, a tricyclic antidepressant, after exposure to clorgyline, an MAOI [55]. The syndrome has since been associated with single, sequential, and combination therapy with serotonergic medications. There are also numerous medication classes with significant interactions with SSRIs, including antibiotics, opiate analgesics, anticonvulsants, antipsychotics, anti-emetics, cough suppressants, drugs of abuse, and herbal medications, that may contribute to development of the syndrome [50,52,56]. Some interactions have also been attributed to inhibition of cytochrome P450 enzymes, altering the hepatic breakdown of SSRIs [57]. Please see Figure 1.
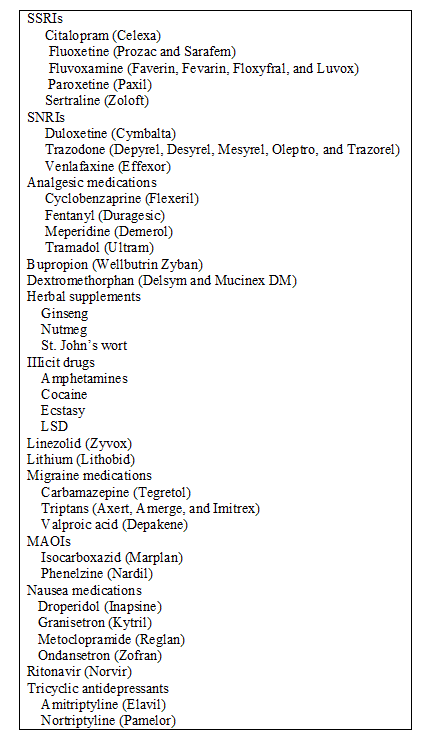 Figure 1: Medications associated with serotonin syndrome [52].
Figure 1: Medications associated with serotonin syndrome [52].
LSD: Lysergic acid Diethylamide; MAOI: Monoamine Oxidase Inhibitor; SNRI: Serotonin-Norepinephrine Reuptake Inhibitor; SSRI: Selective Serotonin Reuptake Inhibitor.
*All trademarked medications remain property of their respective manufactures. View Figure 1
Clinical symptoms of serotonin syndrome exist on a spectrum and range from mild and self-limited to severe and potentially life-threatening. Symptoms can be arranged in 3 categories, which include autonomic instability, neuromuscular changes, and changes in mental status [58,59]. Autonomic signs may include shivering, fever, diaphoresis, tachycardia, tachypnea, and blood pressure lability. Neuromuscular symptoms include rigidity, clonus, and hyperreflexia, which is usually most pronounced in the lower extremities [53]. Mental status changes can range from mild disorientation to confusion, agitation, and even coma.
Diagnosis of serotonin syndrome is difficult, owing to the wide range and severity of symptoms. The differential diagnosis is as extensive as it is severe, including anticholinergic toxicity, dystonia, encephalitis, malignant hyperthermia, meningitis, neuroleptic malignant syndrome, non-convulsive status epilepticus, pheochromocytoma, rabies, sympathomimetic intoxication, tetanus, and thyroid storm [52]. Several diagnostic criteria have been developed in order to assist clinicians. The first was described by Sternbach in 1991 [60]. Since that time, several studies have attempted to improve upon Sternbach's criteria, further characterizing serotonin syndrome on a scale of severity [61,62]. The Hunter criteria were described in 2003, including only 7 clinical features organized into six steps in a decision tree, and were found to be simpler, more sensitive, and more specific than Sternbach's criteria [59]. Please see Table 1.
Table 1: Hunter criteria for diagnosis of serotonin toxicity [59]. View Table 1
Management of serotonin syndrome should begin with cessation of any inciting medications. Supportive therapy comprises the basis of treatment, with goals to address abnormal vital signs and control agitation and autonomic symptoms. Mild symptoms (tremor, hyperreflexia) typically resolve in 24 hours with conservative management [63]. More severe symptoms, including agitation and altered mental status, should be addressed with benzodiazepines. Hyperthermia should be managed with sedation, orotracheal intubation, and muscle paralysis, as significant elevations in temperature are largely attributed to increased muscle tone [50].
Targeted pharmacotherapy with serotonin receptor antagonists remains a controversial option in serotonin syndrome management. Cyproheptadine, a non-specific antihistamine, has been effective at controlling symptoms in some cases, though improvement in patient outcomes has not been proven [64,65]. It is available in an oral preparation, which may be crushed and administered via nasogastric tube to intubated and sedated patients. Dosing varies, with one suggested regimen including a 12-mg initial dose, with 8 mg every 12 hours as maintenance therapy [50].
Chlorpromazine, a typical antipsychotic, has also been utilized and is available as a parenteral agent. However, side-effects may include hypotension, hyperthermia, dystonia, and development of neuroleptic malignant syndrome, thus limiting its usefulness [66].
There is controversy as to restarting offending agents after the syndrome is fully treated. It is generally held that one should restart necessary agents (e.g. antipsychotics for a patient with schizophrenia) at low doses, with slow titration. Polypharmacy should be monitored closely.
Serotonin syndrome is most often medication-induced, when single or multiple serotonergic medications cause excess neurotransmitter activity in the CNS. Categories of symptoms include autonomic instability, neuromuscular changes, and changes in mental status. Diagnosis is based purely on history and clinical findings; as a result, several diagnostic criteria have been developed to assist clinicians. Management is directed at withdrawing the causative agents in addition to supportive care. Hyperthermia should be managed with intubation, sedation, and paralysis to relax the muscle rigidity responsible for elevated temperatures. Though cyproheptadine has been described and used as a potential antidote, there is limited evidence to support improved patient outcomes.
Critical care psychosis or delirium occurs often in critically ill patients and may sometimes mimic psychosis secondary to a primary psychiatric disorder. Distinguishing medical causes of delirium can be difficult but is an essential skill for those practicing in a critical care setting. Three potential non-infectious causes of delirium include alcohol withdrawal syndrome, anti-NDMA receptor encephalitis, and serotonin syndrome. These syndromes usually present with hyperactive delirium - agitation and hyperactivity - but can progress to coma. The necessary workup and treatment varies for each. With a better understanding of these common illnesses, appropriate therapies can be initiated which may lessen the duration and severity of symptoms and improve overall outcomes in the critically ill.
The authors have no pertinent financial disclosures or conflicts of interest.