The purpose of this study is to examine the effects of the COVID-19 pandemic on the social life, mental health and physical performance of the elderly and to compile studies on this subject.
A literature review of the studies examining the subjects of the elderly and COVID-19 was conducted. PubMed and Web of Science databases were used for the analysis. The search period was planned to cover the dates 15 March 2020 and 15 February 2021. The PRISMA guideline was conducted 60 out of 463 studies were examined according to the research criteria.
60 of the 463 studies found in accordance with the research criteria were examined and common results were given from these studies. Most of the studies have been conducted via online survey due to COVID-19 measures. There are also studies conducted through telephone surveys and social media. Especially as of the second half of 2020, significant increase in the number of studies determined.
Due to the fragile nature of the elderly and secondary reasons, COVID-19 infection affected the elderly more severely. In addition to physical effects, there are also social and psychological effects on the elderly. In most countries, elderly people have been forced to either forced or voluntary isolation at home due to restrictions. This not only brought about social and psychological problems, but also caused a change in their physical capacities. The elderly, who have to change their normal lifestyle in an abnormal way, are exposed to the negativity brought about by the pandemic.
COVID-19, Elderly, Life quality, Pandemic, Physiotherapy, Psychotherapy
A new SARS-CoV-2 infection has been identified as the cause of a series of pneumonia cases in Wuhan, China. It spread rapidly and caused an epidemic throughout China, and then followed by increases in cases in other countries around the world. In February 2020, the World Health Organization named this viral infection as COVID-19 disease, which stands for 2019 Coronavirus disease [1]. Among symptomatic COVID-19 patients, cough, myalgia, and headache are the most frequently reported symptoms. Other features such as diarrhea, sore throat, and smell or taste abnormalities have been noted as other symptoms that may be seen in patients. In infection that turns into pneumonia, findings such as fever, cough, shortness of breath and ground glass appearance on radiological imaging are the most common serious findings [2]. Although some clinical symptoms, especially smell or taste disturbances, distinguish COVID-19 from other viral respiratory infections, there are no specific symptoms or signs that can reliably differentiate COVID-19 [3]. However, the development of dyspnea about a week after onset symptoms may suggest COVID-19. Among those with risk factors for severe disease symptoms; advanced age and some underlying medical comorbidities can be listed. Specific demographic features and laboratory abnormalities have also been associated with this serious disease. Several estimation methods have been proposed to identify patients with a higher likelihood of developing severe disease based on epidemiological, clinical and laboratory characteristics; however, studies evaluating these methods have not been clinically confirmed [4]. Individuals of all ages can become infected with SARS-CoV-2, but adults of middle age and older are the most affected. The elderly is more likely to have the disease and the symptoms [5,6]. Older age is also associated with increased mortality. According to the China Center for Disease Control and Prevention, it has been reported that the mortality rate of all cases is 2.3%, while the mortality rate between the ages of 70 and 79 is 8%, and those aged 80 and over are 15% [7]. In an analysis conducted in the United Kingdom, the risk of death of individuals aged 80 and over was found to be 20 times higher than the death risk of individuals aged 50 to 59 [8]. In the United States, 67% of 2449 patients diagnosed with COVID-19 between February 12 and March 16 in 2020 were older than 45. Similar to the findings in China, the death rate was the highest among older people, with 80% of deaths occurring among older people. In a research conducted; individuals aged 18 to 34 years were reported to account for only 5% of adults hospitalized for COVID-19, with a death rate of 2.7%. Morbid obesity, hypertension and male gender were reported to be highly associated with these deaths [9,10]. In the elderly, due to age-related physiological changes, the immune system weakens and insufficient response occurs.
Increased risk of invasion by pathogenic organisms is observed due to changes in the barriers formed by the skin, lungs and gastrointestinal system. The risk of intracellular pathogen detection increases due to the loss of the proliferative capacity of immune cells and the reduced production of specific cytokines such as interleukin 2. After infection, cells in the elderly have impaired defense system against fungal and viral pathogens due to impaired signal transduction after cytokine binding. They give reduced antibody response to vaccines associated with decreases in CD8 and CD4 cell populations and changes in B cell biology. Accordingly, the infection causes antibody responses associated with impaired immunoglobulin production and reduction in B cells [11-13]. Older adults with chronic diseases such as diabetes, chronic obstructive pulmonary disease, or heart failure are more immune compromised, resulting in greater susceptibility to common infections and poorer vaccine responses. The risk of infection in elderly patients generally increases in other social areas such as social settings, crowded places, day care centers and elderly nursing homes [14,15]. Comorbidities associated with severe disease can be listed as cardiovascular disease, diabetes, hypertension, chronic lung disease, cancer (especially hematological malignancies, lung cancer and metastases), chronic kidney disease, obesity, and smoking.
Among patients with advanced age and these medical comorbidities, COVID-19 infection is severe. For example, in the SARS-CoV-2 outbreak that occurred in several long-term care facilities in Washington State, the hospitalization rate of 101 affected facility residents was reported as 55% and mortality rates as 34%. An underlying chronic secondary disease was found in 94% of the patients who died [16]. In the analysis of approximately 300,000 confirmed cases of COVID-19 reported in the United States, the mortality rate was 12 times higher among patients with reported comorbidities [17]. Various complications such as acute respiratory distress syndrome, the most important complication in patients with severe disease caused by COVID-19, arrhythmias, pulmonary embolism, thromboembolic complications including acute stroke, encephalopathy and persistent fever have been identified in the literature. In addition, secondary infections and long-term permanent damage are among the expected complications of COVID-19. Infection is the primary cause of death in one third of individuals aged 65 and over. Infection also has a pronounced effect on morbidity in older adults; exacerbates the underlying diseases and causes functional regression. Multiple biological and social factors reveal that the elderly is more susceptible to infection. The COVID-19 pandemic had a serious impact on the elderly as an infection, and nearly 80% of all deaths were seen in the elderly aged 65 and over. In our study, we focused on the secondary health problems caused by the pandemic on the elderly for one year, such as physical activity, depression, loneliness, and social problems. And we made an analysis by examining the research studies on these topics in the literature.
The PRISMA flow chart illustrating the selection process for all included and excluded studies were given in Figure 1. Total of 561 studies were examined detected by database scan. 60 out of 463 studies were examined according to the research criteria and common results from these studies were given. The review was performed in accordance with Preferred Recording Items for Systematic Review and Meta-analysis (PRISMA) Statements [18]. Studies that did not directly or indirectly address the elderly population were excluded. Publications with the language of publication in English were examined and publications in other languages were not included in the study.
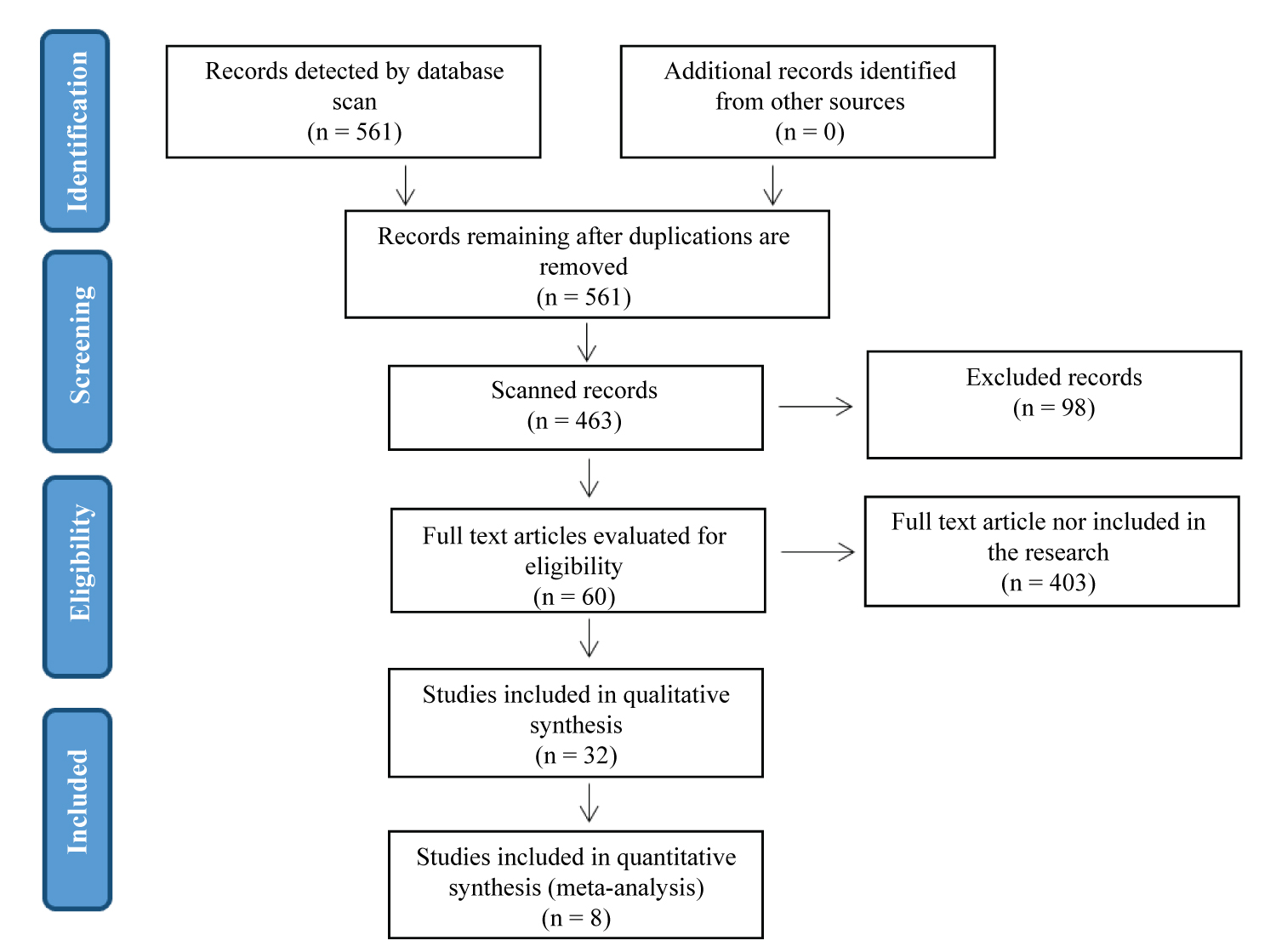 Figure 1: Flow chart illustrating the selection process for all included and excluded studies.
View Figure 1
Figure 1: Flow chart illustrating the selection process for all included and excluded studies.
View Figure 1
A literature review of studies examining older adults and COVID-19 issues was conducted. PubMed and Web of Science were selected from databases indexing world health sciences research studies. The search period was planned to cover the years 15 March 2020 and 15 February 2021. As a search strategy in databases; [«COVID» [Mesh] OR COVID19 OR « COVID-19 »] AND [older OR elderly OR aging OR «Aged» [Mesh AND «physiotherapy»]] and [covid AND aged AND physiotherapy] were used. Participants in the trials were elderly patients (age ≥ 65 years) with COVID-19.
According to PRISMA guideline; 60 studies were examined and 8 of them was given as an example in Table 1. Most of the studies have been conducted in the form of an online questionnaire due to COVID-19 measures. There are also studies conducted through telephone surveys and social media. The participant profiles of the studies consist of older people or all adults. Participant numbers vary between 93 and 6186. Scales and questionnaires used in studies are;
Table 1: Sample studies related to COVID-19 and the elderly. View Table 1
Depression Rating Scale (DRS), Delirium Clinical Assessment Protocol (CAP), Aggressive Behavior Scale (ABS), Activities of Daily Living Hierarchy (ADL Hierarchy), Cognitive Performance Scale (CPS), Revised Index of Social Engagement (RISE), International Physical Activity Questionnaire (IPAQ-SF) Short form, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI, World Health Organization Quality of Life Scale (WHOQOL-BREF), UCLA Loneliness Scale (UCLA), Patient Health Questionnaire (PHQ-9), Mini mental test (MMT) , Functional Independence Measure (FAST), Rating of Perceived Capacity scale (RPC) , Life Satisfaction Questionnaire-11 (LISAT-11), Lawton Instrumental Activities of Daily Living Scale (IADL), Geriatric Depression Scale (M-GDS), Dietary History Questionnaire (DHQ United States Department of Agriculture (USDA) Household Food Security Survey, General Health Questionnaire-12 (GHQ-12) [19-41] as shown in Table 1.
According to the literature, the results of the studies evaluating the negative effects of COVID-19 on the elderly in many aspects are shown in Figure 2. In the study with lowest participant (n: 93) the mean age is 73 and the outcome of the study is interpretation of increased loneliness, sleep problems and psychological problems in the elderly [42]. At the same time, in the study with highest participant (n: 6186) the participants mean age is 36 including the elderly population and the outcome of the study is increased loneliness [43,44]. The highest mean age (82) of the participants is seen in study of face-to-face survey in Norway [45].
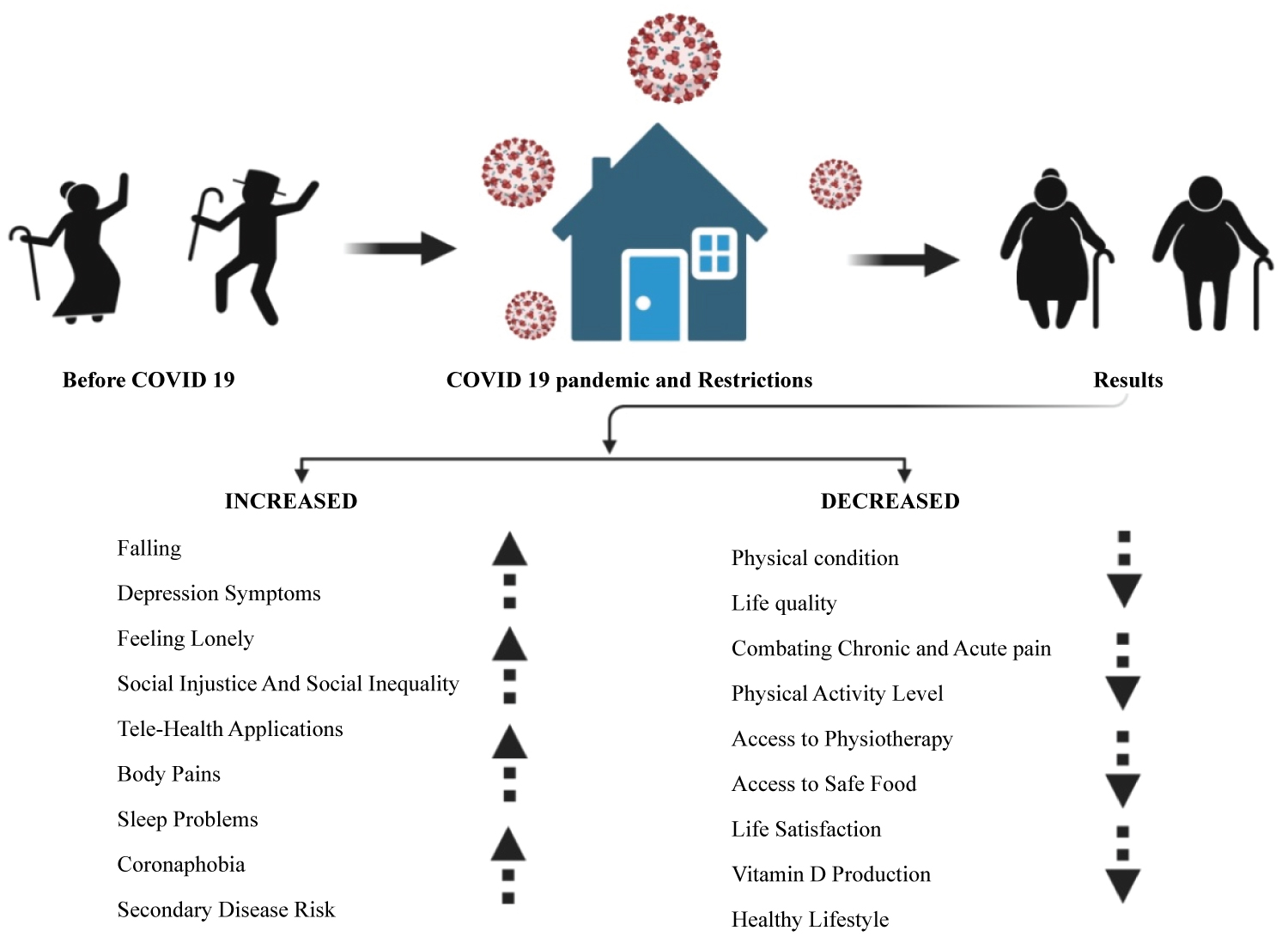 Figure 2: Effects of COVID 19 on the elderly.
View Figure 2
Figure 2: Effects of COVID 19 on the elderly.
View Figure 2
COVID-19 infection has affected all of humanity as well as the elderly. Due to the fragile nature of the elderly and secondary reasons, this impact was felt more severely. The reasons for these are; their health conditions such as having chronic diseases, fragile structure of the body and weak immune system. In addition to physical effects, it also has social and psychological effects. In this study, we presented a one-year up-to-date summary of studies conducted in various countries in the literature that examined the elderly directly or indirectly.
In most countries, due to restrictions, elderly people have been forced to either forced or voluntary isolation at home. This not only caused social and psychological problems, but also caused a change in their physical capacities. According to the literature; the results of the studies evaluating the negative effects of COVID-19 on the elderly in many aspects are shown in Figure 2. These negative effects of COVID-19 on the elderly are decreased physical condition, life quality, physical activity level, access to physiotherapy and safe food, life satisfaction and vitamin D production. Also, there is increased risk of falling, depression syndromes, body pain, sleep problems, corona-phobia and secondary disease risk for the elderly as negative results of pandemic (Figure 2).
The elderly, who have to change their normal lifestyle in an abnormal way, are also exposed to the adverse effects of the pandemic. Emphasizing that falls may become a new epidemic, scientists emphasized that the physical condition of the elderly decreases with the duration of staying at home and this trigger falls. It was emphasized that the elderly should be directed to resistive exercise and physical activities at home in order to maintain physical condition [46-50]. Increasing depression symptoms has been the main subject of many studies in the literature. The increase in depressive thoughts, which we think is related with physical inactivity, affects the mental health of the elderly [40]. Quality of life is an issue that needs to be handled as a whole. The decrease in physical condition and mental health deterioration naturally caused a decrease in the quality of life in the elderly [41,42]. Loneliness or being alone is a feeling of being cut off from the world along with a feeling of emptiness. Loneliness is an emotion that goes further than a lack of friends or a desire to be with others. People who are lonely may feel disconnected from society and have difficulty in meaningful communication with other people. Another feeling created by the pandemic is the feeling of loneliness in the elderly. Social injustice and inequality arise as a big problem during the pandemic as everywhere. Difficulties in accessing hygiene products, difficulties in food supply and financial inequality have revealed the distance between the elderly and other adults [51]. The tendency towards telephone-health applications has increased more in this period and it has been an opportunity for people to explain their health problems without leaving home and to get solutions for this with this method. Tele or mobile health has an important place in patient follow-up for healthcare professionals [42,52,53].
The sun is the biggest source of vitamin D and an indispensable natural source for the elderly. The elderly, who had to stay at home due to restrictions, could not benefit from this natural resource sufficiently. In a study, attention was drawn to the vitamin D deficiency during the pandemic period [54]. The impairment of dealing with chronic or acute pain is also vital for the elderly. Not being able to go to the hospital, insufficient medical support, financial problems, mental fears and depressive thoughts have changed the approach of the elderly to pain and created a weakness in their struggle [51]. It was obligatory for patients who needed physiotherapy to direct their treatment to home-based applications, but their treatment was interrupted during the restriction period. In a study conducted in patients with Parkinson's, it was found that depressive thoughts of patients who could not receive physical therapy increased and their treatment was disrupted during the pandemic [55].
Corona-phobia and sleep problems are closely related. Another negative effect seen during the pandemic is sleep. According to an online survey with 700 people; it has been observed that people staying at home have increased sleep problems compared to working people. However; it should be considered that there is limitation for the online survey studies because their use is not easy for elderly and only ones having confidence with the digital can access to the survey which may affect the outcome of the studies. Also, it was found that Corona-phobia values were higher in those staying at home. There are other studies pointing out that the sleep problem increased during the pandemic period [42,56]. Physical activity is defined as any movement that is performed using skeletal muscles in daily life and requires energy expenditure. Exercise (Regular Physical Activity) is regular, planned and repetitive physical activities aimed at maintaining or improving physical fitness. Regular physical activity has positive effects on the function of many systems and organs. It has been shown that regular exercise increases the life expectancy and quality of life even in people who did not do regular physical activity until old age. Physical activity levels in the pandemic have decreased significantly due to staying at home and this will cause an increase in the risk of many secondary diseases [41,57,43]. Poor food intake and food insecurity caused mental health to be affected in the elderly and caused the development of depression [47]. These effects can be considered as lifestyle changes. This lifestyle change has been extremely devastating for the elderly, who we describe as the oldest link in the COVID-19 pandemic. For example, values such as increased insulin level and body mass index ratios and cholesterol were affected by this lifestyle change [58]. On the other hand, there is also factors that can exacerbate the negative consequences of pandemic such including their living conditions. In the studies; it could be interesting to know if there are differences between elderly people living alone or with their wife/husband in terms of COVID-19 effects, or between elderly leaving in city or in countryside which may affect the negative effect of COVID-19 on the elderly. However, there is only one study that takes into account the living conditions of the elderly including education, civil status, having children and residential community site. As a result of these effects, it is expected that the elderly feelings of satisfaction with life decrease [46].
In order to protect the elderly and reduce the transmission in the pandemic, restrictions and protection measures have been taken in many countries. The difficulties experienced by elderly individuals in trying to cope with the coronavirus and getting used to the new normal after a conventional order have been investigated in many different areas. The most important thing we can do for the elderly is to empathize and manage this process in cooperation by helping these weak links of the pandemic. Complying with hygiene rules and avoiding crowded environments is the biggest responsibility of individuals. At the same time, it is the biggest responsibility of young adults to be with the elderly with social and psychological support and to encourage them to physical activity.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The figure of this review was created with Biorender.com