Introduction: Renal cell carcinoma (RCC) is the most common tumour of the kidney. The common histological subtypes are clear cell, papillary and chromophobe renal cell carcinomas. This case has several unique features, which makes it a rare presentation. The most important unique fact is the presence of all the three common histological types of renal cell carcinoma in the same patient, which is a rarity.
Presentation: 63-years-old male from Tanzania with End Stage Renal Disease came to hospital for Live Donor renal transplantation. Incidental detection of left renal tumor of size 3 cm diameter in the lower pole of kidney was made. He underwent laparoscopic radical nephrectomy. The histopathology was clear cell renal cell carcinoma. He came back later after 3 years with persistent cough. On evaluation was found to have a 5 cm pulmonary metastasis and two tumors in the upper pole of right kidney. One of the tumours was 3 cm and was solid and the other was 2.5 cm complex cystic tumor. Laparoscopic right radical nephrectomy with partial pneumonectomy was done. Histopathology was papillary renal cell carcinoma in the cystic renal tumor and pulmonary metastasis. Chromophobe renal cell carcinoma reported in the solid renal tumor. The following immunohistochemical markers were used in the sub typing: Cytokeratin 7, vimentin and progesterone receptor.
Conclusion: Multitype and multifocal renal cell carcinoma though rare we may come across them. In these situations, it is prudent to suspect HRTS (Hereditary renal tumor syndrome). If these patients are on hemodialysis with ESRD a radical nephrectomy would be better option than partial nephrectomy. B/L radical nephrectomy in ESRD patients can be done in patients with good vascular access.
Renal cell carcinoma (RCC) is the most common tumour of the kidney. The common histological subtypes are clear cell, papillary and chromophobe renal cell carcinomas. This case has several unique features, which makes it a rare presentation. The most important unique fact is the presence of all the three common histological types of renal cell carcinoma in the same patient, which is a rarity.
63-years-old male from Tanzania with end stage renal disease came to hospital for Live Donor renal transplantation. Incidental detection of left renal tumor of size 3cm diameter in the lower pole on CT scan was made in the process of transplant work up (Figure 1). He was on dialysis twice a week with a permacath in place. He was not willing for arterio-venous fistula for hemodialysis. His urine output is around 100-200 ml per day. He was with the following Co-morbidities: Hypertension for 10 years, Diabetes mellitus for 10 years, Hypothyroidism for 10 years. Whole body FDG PET CT scan taken did not show any evidence of distant metastatic spread. Laparoscopic left radical nephrectomy and the histopathological evaluation of specimen came out as clear cell renal cell carcinomagrade 2 (WHO/ISUP grading system) without necrosis, lympho-vascular invasion and lymph nodes. Patient was explained about possibility of early transplantation, however he decided to wait and come back later. He went back home with a detailed follow up advice. He was on teleconsultation with support of local consultant at 3 months and 6 months. After which there was no follow up.Three years later he presented to the hospital with persistent cough lasting for 1 month. His urine output was Nil after the nephrectomy. He was on Three times a week hemodialysis via a right permacath. CT scan of chest showed a 5 cm × 3 cm × 2.5 cm mass in the anterior segment of upper lobe of right lung. CT scan abdomen showed a small SOL of size 3.2/2.8 cm and a complex cyst 2.5 cm diameter in the upper pole of right kidney. On FDG PET there was no evidence of metabolic activity elsewhere. Multidisciplinary Urology-nephrology-oncology combined discussion with the patient was done and the following treatment options were suggested: Biopsy and Targeted molecular therapy, Right radical nephrectomy with metastasectomy (R Segmental Pneumonectomy), right Partial nephrectomy with right Segmental pneumonectomy. Patient preferred surgical cure with Radical nephrectomy and segmental pneumonectomy. Partial nephrectomy was deferred as the tumor was suspected to be a HRTS (Hereditary Renal Tumor Syndrome) and recurrence in the residual renal parenchyma was anticipated. The nephrology team was confident that they can maintain him on dialysis after nephrectomy. Right laparoscopic radical nephrectomy was done first with operative time of 2.5 to 3 hours. Followed by right thoracotomy with bi-lobectomy of lung by the once-surgical team. Lateral position and 5 th intercostal space thoracotomy approach was done and right bi-lobectomy carried out as mass was adherent to the middle lobe. Time taken for pneumonectomy was 3 hours. Two units of Packed RBC were transfused intra-operatively. Both the specimens sent separately for histopathology evaluation.
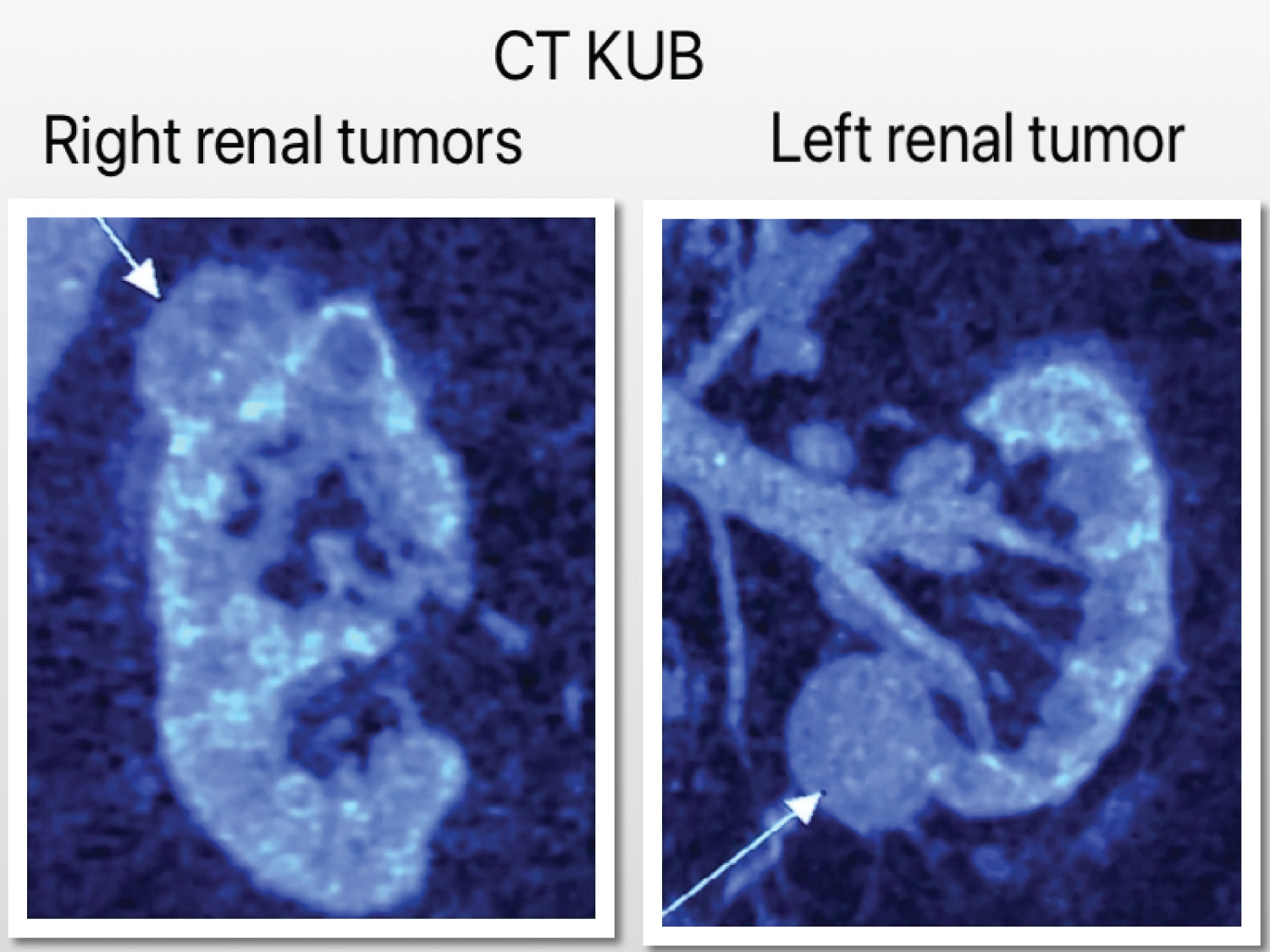 Figure 1: CT KUB of right renal tumor and left renal tumor.
View Figure 1
Figure 1: CT KUB of right renal tumor and left renal tumor.
View Figure 1
Histopathology of the specimen revealed that the lung metastasis was papillary RCC type 1. The solid SOL in kidney was a chromophobe renal cell carcinoma and the complex cyst was a papillary renal cell carcinoma type 1. The pathologist in addition to the routine staining and processing of specimen the following immune-histochemical markers were used: Cytokeratin-7, Vimentin and Progesterone Receptor. Sheets of large polygonal Cells with eosinophilic granular cytoplasm, with distinctive cell borders, with large vesicular nuclei, with peri nuclear halo arranged in alveoli and solid nests separated by fibrous septa with Cytokeratin-7 positive and other two markers were negative in chromophobe renal cell carcinoma was noted.
Basophilic cells with scarce clear cytoplasm, with hyper- chromatic nuclei surrounding the basal membrane arranged in a papillary pattern over a fibrovascular core with Vimentin positive and other two markers negative was noted in papillary renal cell carcinoma (Figure 2).
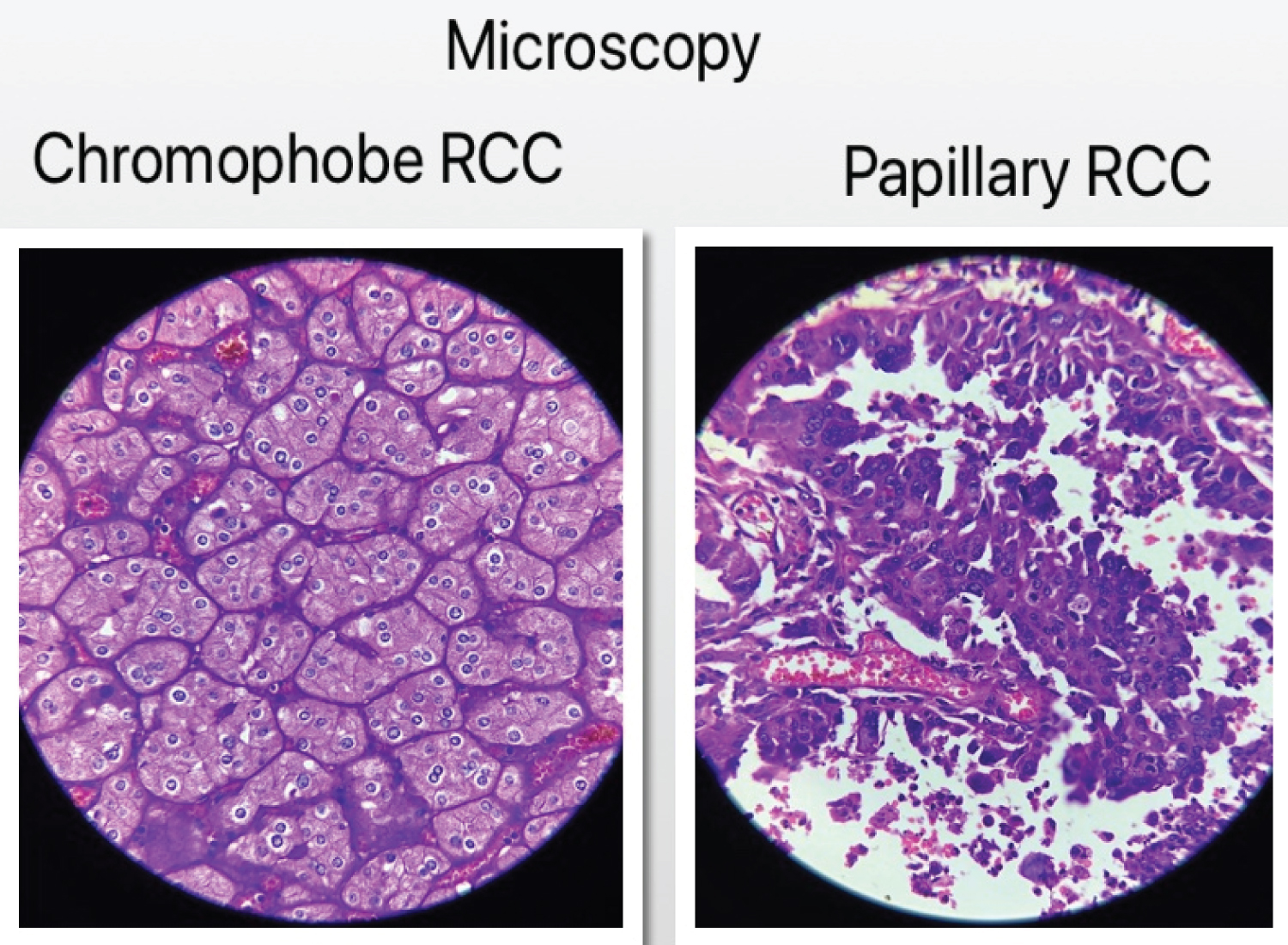 Figure 2: Microscopy of renal cell carcinoma.
View Figure 2
Figure 2: Microscopy of renal cell carcinoma.
View Figure 2
Renal cell carcinoma (RCC) is the most common tumour of the kidney, accounts for 90% of all renal tumours [1]. The presence of histologically three different subtypes of renal tumours in the same patient is rare, with most case reports describing up to two subtypes [2-5]. Martha C, et al. described 3 subtypes clear cell, type 1 and type 2 papillary renal cell carcinoma, but not chromophobe renal cell carcinoma [6]. Bilateral radical nephrectomy in renal failure patients who are on dialysis is not commonly done [7-9]. The anephric status patients pose certain unique challenges than nephric patients on dialysis. The nephric patients and anephric patients on dialysis behave similar in the degree of uremic intoxication. But the hormonal deficiency effects are more common in anephric patients. It seems that though the tubulo-glomerular function is defective in end stage renal disease patients, the hormonal functions are significantly retained [10,11]. The anephric patients are more prone for anemia due to impaired erythropoiesis. Some patients with anephric status are prone to sodium chloride and volume dependent blood pressure fluctuation requiring tight monitoring of salt and water intake. Severe hypotension or hypertension is possible and must be watched for. These are due to absence of Renin-Angiotensin mechanism. Blood pressure monitoring during and after dialysis is essential. Home monitoring of blood pressure and a watch for giddiness and other symptoms of hypotension/hypertension is required [10,11]. Some anephric patients experience hypocalcemia [10,11]. However the incidence of renal osteodystrophy is similar in nephric and anephric patients.
Bilateral radical nephrectomy with Metastasectomy (Pneumonectomy) is an even uncommonly done procedure in renal failure patients on dialysis. HRTS (Hereditary renal tumor syndrome) must be suspected in patients with multiple renal tumours, bilateral renal tumours, Tumours in less than 46-years-old and 1 st or 2 nd degree relatives having RCC [12]. Although it must be known that most of the bilateral renal tumors are sporadic and not hereditary [13]. Patients with HRTS are at an increased risk for the development of additional renal tumours, even when the original tumour has been resected [14]. So in end stage renal disease leaving a non-function renal stump after partial nephrectomy is arguable (Figure 3). When considering surgical options of metastatic renal cell carcinoma, it is required to think whether to do a metastasectomyornot. Its important to note that the mean overall survival is better with metastasectomy than without: 40 months vs. 14 months [15]. However, these survival data may not be applicable in the scenario with different subtypes of renal cell carcinoma in same patient and in patients with bilateral renal tumours. As the occurrence of such tumours are rare there are no available data to suggest which treatment option gives superior results. The biological behaviour of different subtypes of renal cell carcinoma are different with different survival outcomes [16].
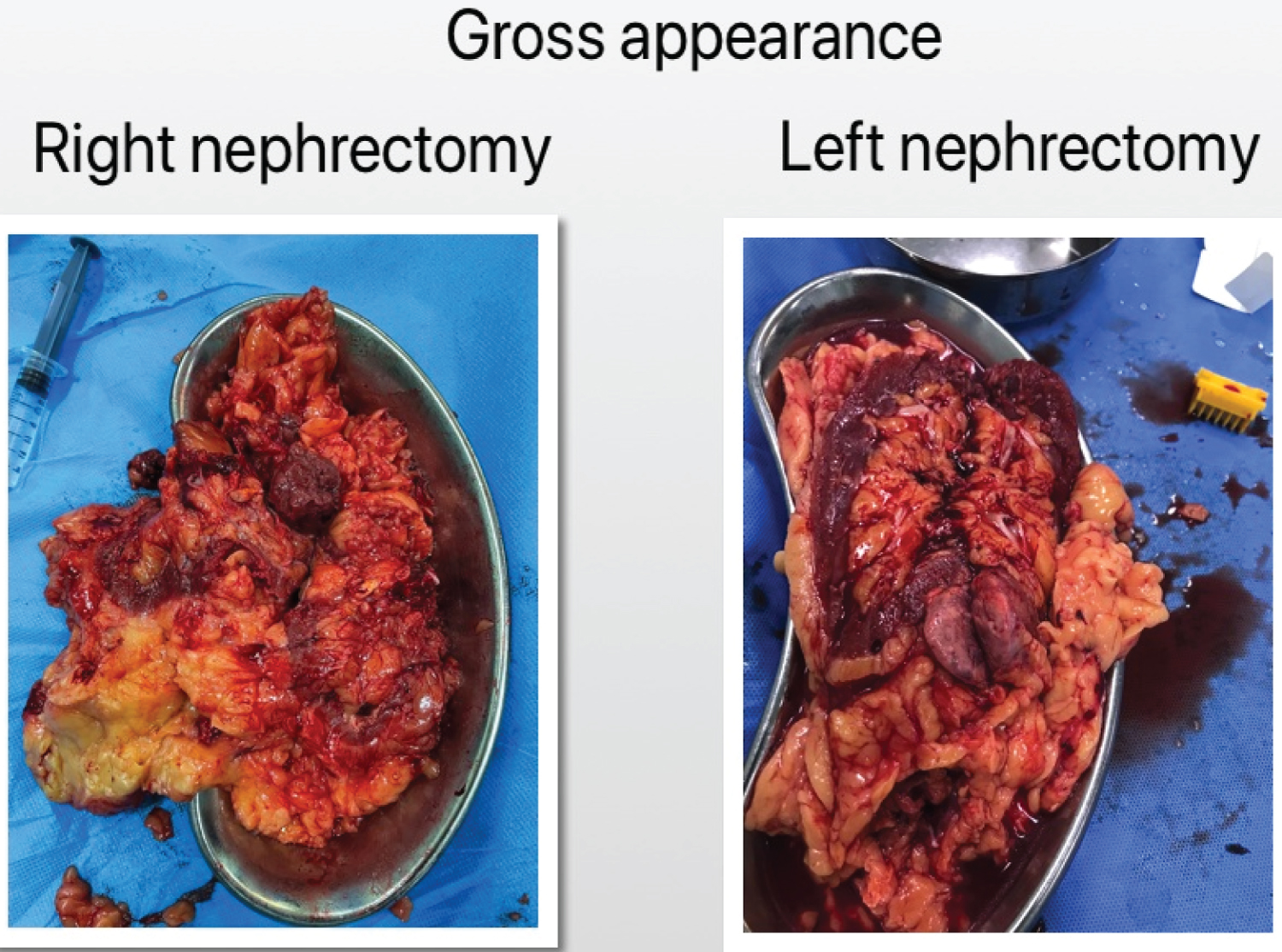 Figure 3: Gross appearance of right nephrectomy and left nephrectomy.
View Figure 3
Figure 3: Gross appearance of right nephrectomy and left nephrectomy.
View Figure 3
Regarding dialysis maintain ability after bilateral nephrectomy. Bilateral radical nephrectomy in renal failure patients and on maintenance dialysis are reported [7-9]. Bilateral radical nephrectomy and renal transplantation after 6-years of maintenance dialysis [17] and after 2 years [18] are also reported. Whether renal transplantation after metastasectomy can be done? there are no studies found, supporting it. The life expectancy of the patient with end stage renal disease must be at least 5-years after considering the co-morbidities to include in the wait list for renal transplantation [19]. Even after radical nephrectomy and metastasectomy, 5-year survival may be difficult to achieve. There is always a concern of tumor spread after transplantation and immunosuppression. According to a recent systematic review the risk of tumour recurrence was similar between transplantation (n = 786) and dialysis (n = 1,733) populations for renal cell carcinoma (RCC) [20]. It was needed to consider the waiting period after nephrectomy before renal transplantation. For low stage and low grade renal cell carcinomas the European association of urologist guideline suggests that no additional delay is required after appropriate treatment of the disease has been carried out [21]. However the evidence supporting early transplantation was weak. In general, for solid renal tumours an average waiting period of 2-years is advisable [22]. Renal cell carcinomas are classified into various subtypes based on 2016 WHO/ISUP guidelines. Routine microscopy may not be sufficient to differentiate the various sub types, we need to rely on immunehistochemical markers. Various set of recommended markers are used according to the availability. We have used Cytokeratin 7, Vimentin and Progesterone receptors. The chromophobe renal cell carcinoma must be differentiated between eosinophilic variant of clear cell renal cell carcinoma and oncocytoma. The cytokeratin 7 positive, vimentin negative and progesterone receptor may or may not be positive is the pattern in chromophobe renal cell carcinoma. Cytokeratin 7 negative, Vimentin strong positivity and progesterone receptor negative is the pattern in clear cell renal cell carcinoma and papillary renal cell carcinoma. Cytokeratin 7 and Vimentin negative, but positive for progesterone receptors is the pattern for onchocytoma [23-26]. These patterns of immunohistochemical markers formed the basis of our specimen processing and reporting.
Multitype and multifocal renal cell carcinoma though rare we may come across them. In these situations, it is prudent to suspect HRTS (Hereditary renal tumor syndrome). If these patients are on hemodialysis with ESRD a radical nephrectomy would be better option than partial nephrectomy. B/L radical nephrectomy in ESRD patients can be done in patients with good vascular access.
No funding received from any source and there are no conflicts of interest.