Background: Coronary artery fistulas are abnormal communications between the coronary arteries and other cardiac or pulmonary structures. Many patients are asymptomatic; however, symptoms and complications may develop with increasing age. We discuss a rare case of a 56-year-old woman presenting with chest pain WHO was found to have bilateral coronary fistulae. We also review relevant literature regarding diagnosis and management options.
Coronary artery fistula, CTCA, Congenital heart disease
Coronary artery fistulas (CAFs) are abnormal vascular connections between coronary arteries and cardiac chambers or surrounding blood vessels [1]. They are a rare congenital or acquired anomaly of the coronary circulatory system reported to be present in 0.9% of the population [1,2]. Approaches to treatment are guided by symptoms, fistula anatomy, level of hemodynamic compromise, local expertise and the presence of concurrent cardiac abnormalities. Treatment options include surgical ligation, transcutaneous closure, or observation [2].
1) To gain an understanding of coronary artery to pulmonary artery fistulae and possible signs and symptoms.
2) To learn the indications for intervention and the different ways this can be approached.
A 56-year-old woman presented to the emergency department with 3 days of intermittent chest pain lasting 30 minutes at a time at rest. The pain was not responsive to sublingual GTN spray and overall felt to be atypical for cardiac ischaemia. Her vital signs on presentation were stable: Blood pressure 107/67 mmHg, heart rate 72 beats/minute, saturations were 96% on room air, respiratory rate of 17 and she was afebrile. Her examination was unremarkable. She had no other medical conditions. However, she did have a strong family history of premature coronary artery disease. Initial bloodwork revealed serial negative troponin I over 12 hours, ECG showed sinus rhythm with non specific ST-T changes in V2, 3. Transthoracic echo revealed normal right and left ventricular function with no regional wall motion abnormalities. Given her strong family history of ischaemic heart disease and her New Zealand Māori heritage we proceeded to an inpatient CT Coronary Angiogram (CTCA). CTCA revealed no significant atherosclerotic coronary disease however; it did reveal bilateral coronary-to-pulmonary artery fistulae (Figure 1, Figure 2 and Figure 3). One fistula from the proximal LAD and one from the conus branch of the RCA. As a result, she proceeded to coronary angiogram to better define these fistulae (see Video 1 and Video 2). We discussed the case at our local heart team meeting between cardiology and cardiothoracic surgery. The consensus was that to justify any intervention, we should demonstrate reversible ischemia in the anomalous vascular territories. A subsequent myocardial perfusion scan performed with exercise showed no evidence of reversible ischemia and the LVEF was 70%. On further discussion with cardiologists from another institution experienced in adult congenital heart disease and the consensus was that these bilateral fistulae were likely an incidental finding although we should observe for development of heart failure or concerning cardiac symptoms. The patient was discharged and attends regular follow up appointments with no recurrence of chest pain to date.
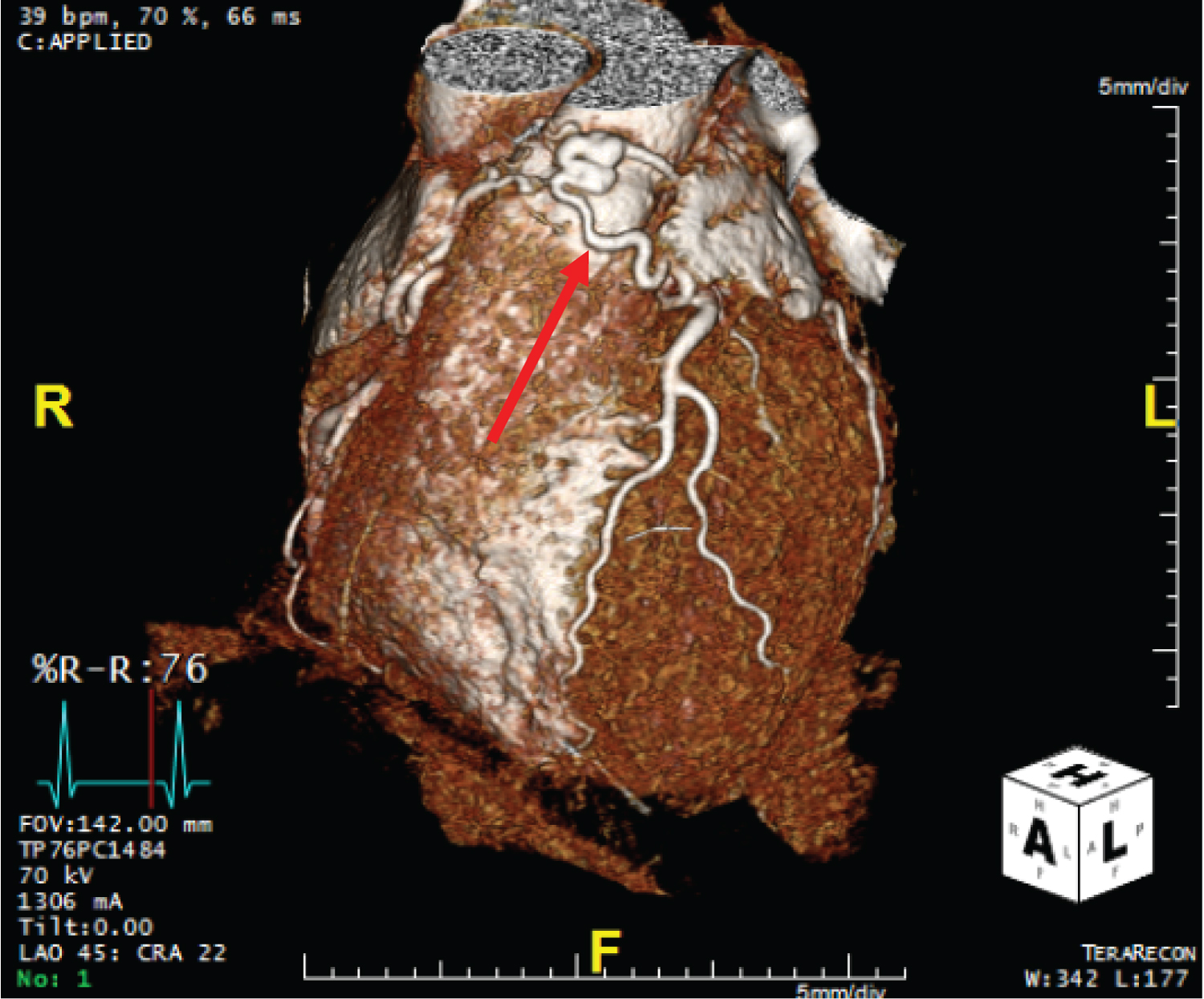 Figure 1: CTCA showing a fistula from the left anterior descending artery to the main pulmonary artery. Highlighted by red arrow.
View Figure 1
Figure 1: CTCA showing a fistula from the left anterior descending artery to the main pulmonary artery. Highlighted by red arrow.
View Figure 1
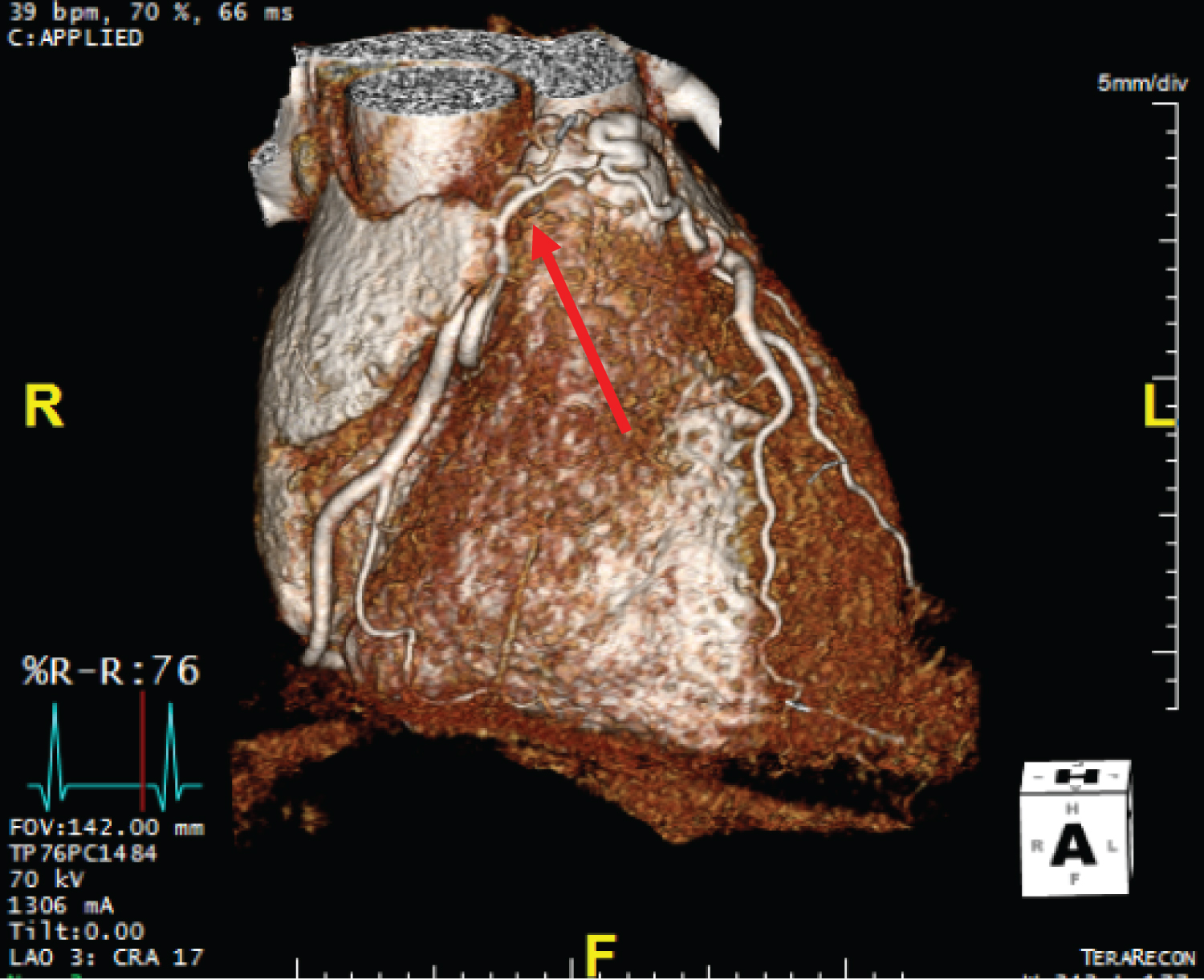 Figure 2: CTCA showing a fistula from the conus branch of the right coronary artery to the main pulmonary artery. Highlighted by red arrow.
View Figure 2
Figure 2: CTCA showing a fistula from the conus branch of the right coronary artery to the main pulmonary artery. Highlighted by red arrow.
View Figure 2
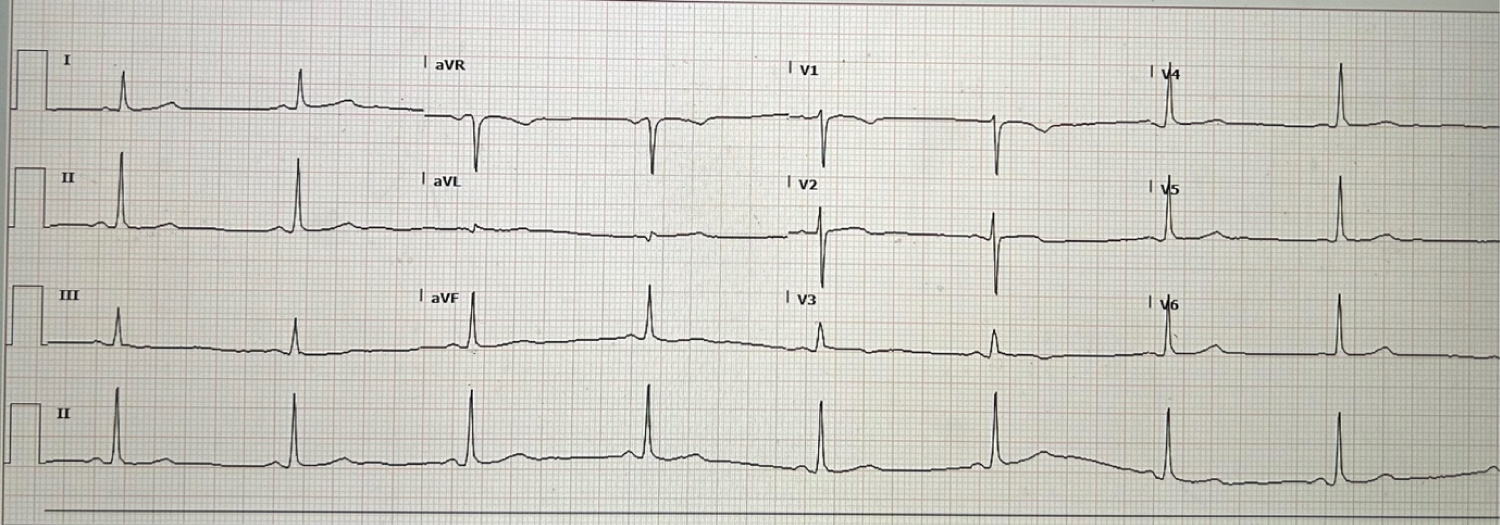 Figure 3: 12 lead ECG - Sinus Rhythm with non Specific T wave inversion lead V3.
View Figure 3
Figure 3: 12 lead ECG - Sinus Rhythm with non Specific T wave inversion lead V3.
View Figure 3
Video 1: RAO Caudal projection of the left anterior descending artery to pulmonary artery fistula.
Video 2: RAO Projection of the right coronary artery to pulmonary artery fistula.
Coronary artery fistulas (CAFs) are a rare congenital or acquired anomaly of the coronary circulatory system reported to be present in 0.9% of the population [1,2]. The bilateral incidence of coronary artery fistulas found in this case, however, are an exceedingly rare variation, accounting for only 5% of all CAFs [2]. The exact mechanism causing coronary-to-pulmonary artery fistulas (CPAFs) remains unclear [1,3]. Fistulas tend to grow with age and approximately half of these patients subsequently develop cardiovascular symptoms [3]. Larger fistulas draining into relatively low resistance pulmonary circulation, like in CPAFs, can divert significant amounts of diastolic run-off away from coronary arteries to the pulmonary artery [4,5]. The resulting compromise of coronary blood supply and myocardial oxygenation is known as the ‘coronary steal phenomenon’ as was originally thought to be the case in our patient [5].
In asymptomatic patients the only potential sign of an underlying CPAF is a continuous cardiac murmur present in 47% of patients and is best auscultated over the second intercostal space of the left sternal edge [1]. Patients with significant left-to-right shunts may present with chest pain, dyspnoea, palpitation and fatigue [3,4]. In severe circumstances, large left-to-right shunts can have deleterious consequences, causing myocardial infarction or chronic ischemia of the territory distal to the fistula and heart failure from pulmonary circuit overload [1]. In our patient, the absence of inducible myocardial ischemia and preserved left ventricular function indicated a benign course, suggesting that the bilateral coronary-pulmonary fistulas were an incidental finding and unlikely the cause of her symptoms.
Coronary angiography and cardiac CT both serve as the gold-standard for diagnosis of CPAFs, with the latter recommended by the 2020 European Society of Cardiology Guidelines to characterise high risk anatomy [6]. Recent evidence suggests cardiac CT detects CAFs at a higher rate, whilst also carrying the advantage of being able to reconstruct three-dimensional models of the coronary anatomy in high resolution [1,7]. Coronary angiography, despite being invasive, has the advantage of precisely mapping the fistula’s origin and termination as well as visualizing the amount of blood flow it receives [1]. Myocardial perfusion scans can subsequently demonstrate the functional hemodynamic consequences, if any, on the patient’s myocardium [8].
Approaches to treatment are guided by symptoms, fistula anatomy, level of hemodynamic compromise, local expertise and the presence of concurrent cardiac abnormalities. Treatment options include surgical ligation, transcutaneous closure, or observation [2]. Indications for intervention are: fistula-associated myocardial ischemia or heart failure symptoms, and significant left-to-right shunt, even in the absence of symptoms, to prevent long term complications [1,2]. Surgical closure has historically been the mainstay of treatment and has demonstrated excellent long-term efficacy, with most patients remaining asymptomatic [2,3,8]. However, surgical intervention carries high postoperative risk of myocardial infarction and is now reserved for patients with multiple fistulas, concurrent cardiac abnormalities or large fistulas with high flow [1]. Since the advent of transcatheter closure as a non-invasive alternative, percutaneous intervention is now first-line in those with favourable anatomy due to lower overall complication and recurrence rates [2,8]. Techniques for transcatheter closure involve either coils or covered stent placement and reported rates of complete occlusion are between 82.9% and 89% in small single-centre, retrospective reviews [9]. These occlusion devices still carry risks and can be complicated by device-associated thromboembolic myocardial ischemia, aneurysmal dilation, haemolysis and device migration [9,10].
The 2020 European Society of Cardiology Adult Congenital Heart Disease guidelines have a paucity of recommendations on coronary artery fistulas [6]. Broadly, functional imaging is endorsed to evaluate for stress-induced ischemia and remains the cornerstone of decision making [6]. Intervention is recommended the presence of symptoms, complications, or significant shunt [6]. In asymptomatic patients with small fistulae, without associated complications, conservative treatment is a safe approach and carries a good prognosis [6,10]. This was the strategy we opted for in our case. Similar cases of bilateral coronary-to-pulmonary fistulas with no clear hemodynamic correlation to symptoms have been described. Kutchetscki, et al. published ten-year follow-up echocardiographic data on a single patient, observing slight bilateral coronary fistula dilation but ultimately preserved ventricular function with good aerobic fitness and no symptoms or signs of myocardial ischemia [10].
Coronary artery fistulae are rare congenital cardiac abnormalities. If closure is indicated, percutaneous options are safe and effective. The decision to close a coronary fistula should be carefully considered and it is reasonable to watch and wait if there are no symptoms or high-risk features.
James Millhouse is the primary author and sourced the case as well as all the images. Harish Kamalanathan primarily did background research. Professor Kuljit Singh performed the angiogram and Professor Niranjan is the managing cardiologist of the patient for long term follow up, both were involved in manuscript review and editing. All authors have approved the final version.
I hereby declare the patient who is the subject of this case report provided informed consent for this report. All patient information has been deidentified.
The authors declare that there is no conflict of interest.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.