Brugada, Sinus node dysfunction, Syncope
Brugada Syndrome is a rare arrhythmogenic entity that poses a risk of sudden cardiac death due to ventricular arrhythmias. Sinus node dysfunction is a less recognized and acknowledged conduction abnormality associated with Brugada syndrome, but nevertheless an important potential manifestation that can alter management. We present a case of a young patient who presented with syncope initially presumed to be secondary to a ventricular arrhythmia in the setting of newly diagnosed Brugada syndrome but was later found to have evidence of sinus node dysfunction. We review the relevant literature and discuss the management.
A 31-year-old male with no significant past medical history presents after a witnessed syncopal episode. He denied any pre or post syncopal symptoms of chest pain, palpitations, fevers, nausea, loss of bowel or bladder control or tongue biting. He does not take any medications and denied any family history of sudden cardiac death. His physical exam and laboratory workup were unremarkable. His ECG showed sinus rhythm with coved ST segment elevation and T wave inversions in leads V1 and V2 consistent with type 1 Brugada pattern (Figure 1). His echocardiogram was unremarkable with normal chamber size, no hypertrophy or valvular disease and a left ventricular ejection fraction of 60%. He was evaluated by general cardiology and electrophysiology and due to the concern for Brugada associated ventricular tachyarrhythmias as the culprit for his syncopal event, the placement of a defibrillator was recommended. After lengthy discussions with the patient about the different types of defibrillators, he elected to have a subcutaneous defibrillator (S-ICD) due to its cosmetic advantage, lack of vascular injury risk and low systemic infection risk (Figure 2). Unfortunately, after placement of his S-ICD, the patient had another syncopal episode associated with dizziness while he was in the hospital. The episode was documented on the telemetry monitor and revealed a 12 second sinus arrest (Figure 3A). The patient received brief CPR before regaining consciousness. Continuous telemetry monitoring revealed multiple episodes of sinus pauses of different durations at different times (Figure 3B). Multiple differential diagnoses were entertained including sinus node dysfunction in the setting of Brugada vs. vasovagal syncope. Due to concerns of recurrent episodes, the patient was presented with different management options including the placement of a pacemaker or a dual chamber ICD and the future removal of the subcutaneous ICD. He deferred further procedures and elected to pursue outpatient cardiac event monitoring. He was scheduled to follow up in clinic with recommendation to obtain an outpatient cardiac MRI to rule out infiltrative diseases. He had a few more episodes of sinus pause documented and Mobitz 1 AV block on his event monitor which he reported were not associated with any syncopal events (Figure 4).
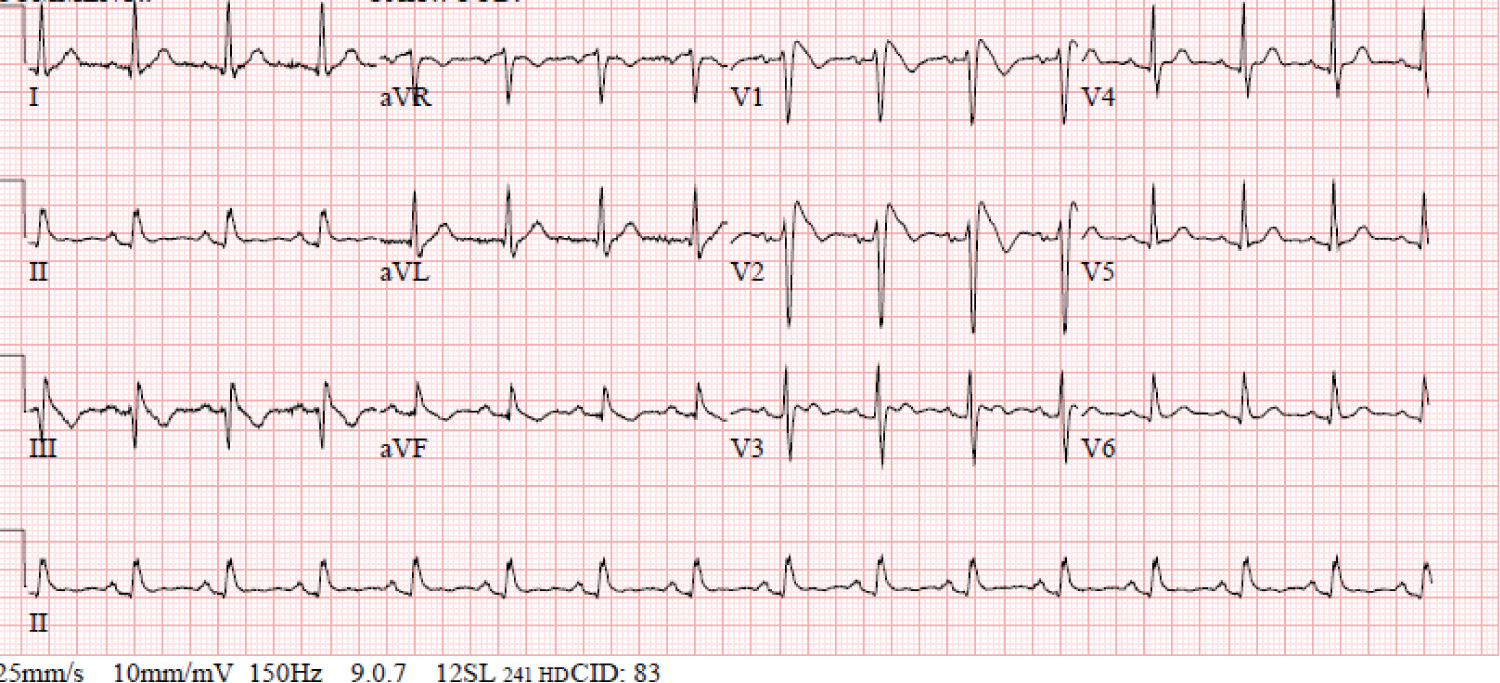 Figure 1: ECG with normal sinus rhythm and type-1 Brugada pattern.
View Figure 1
Figure 1: ECG with normal sinus rhythm and type-1 Brugada pattern.
View Figure 1
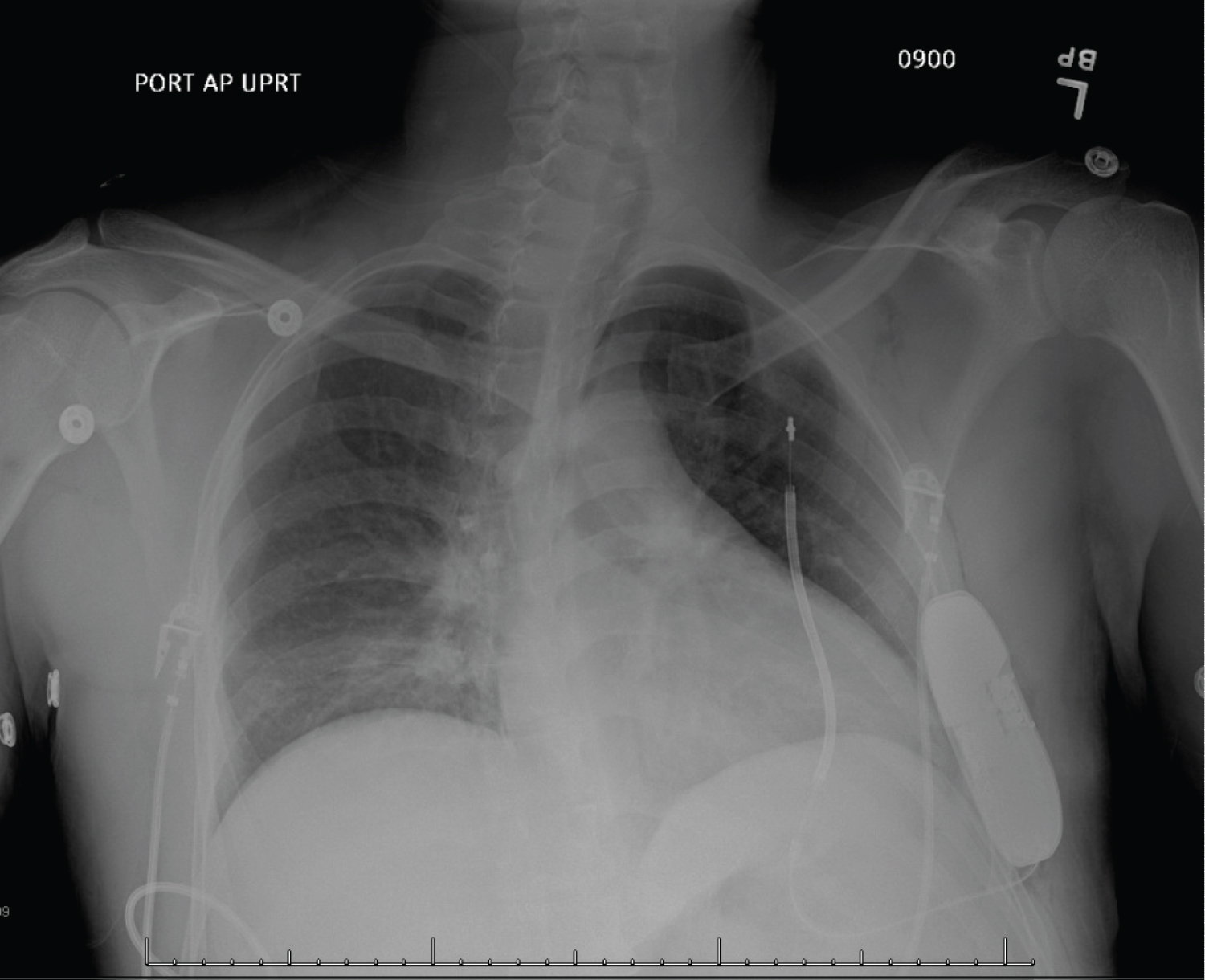 Figure 2: Chest X-ray status post subcutaneous ICD placement.
View Figure 2
Figure 2: Chest X-ray status post subcutaneous ICD placement.
View Figure 2
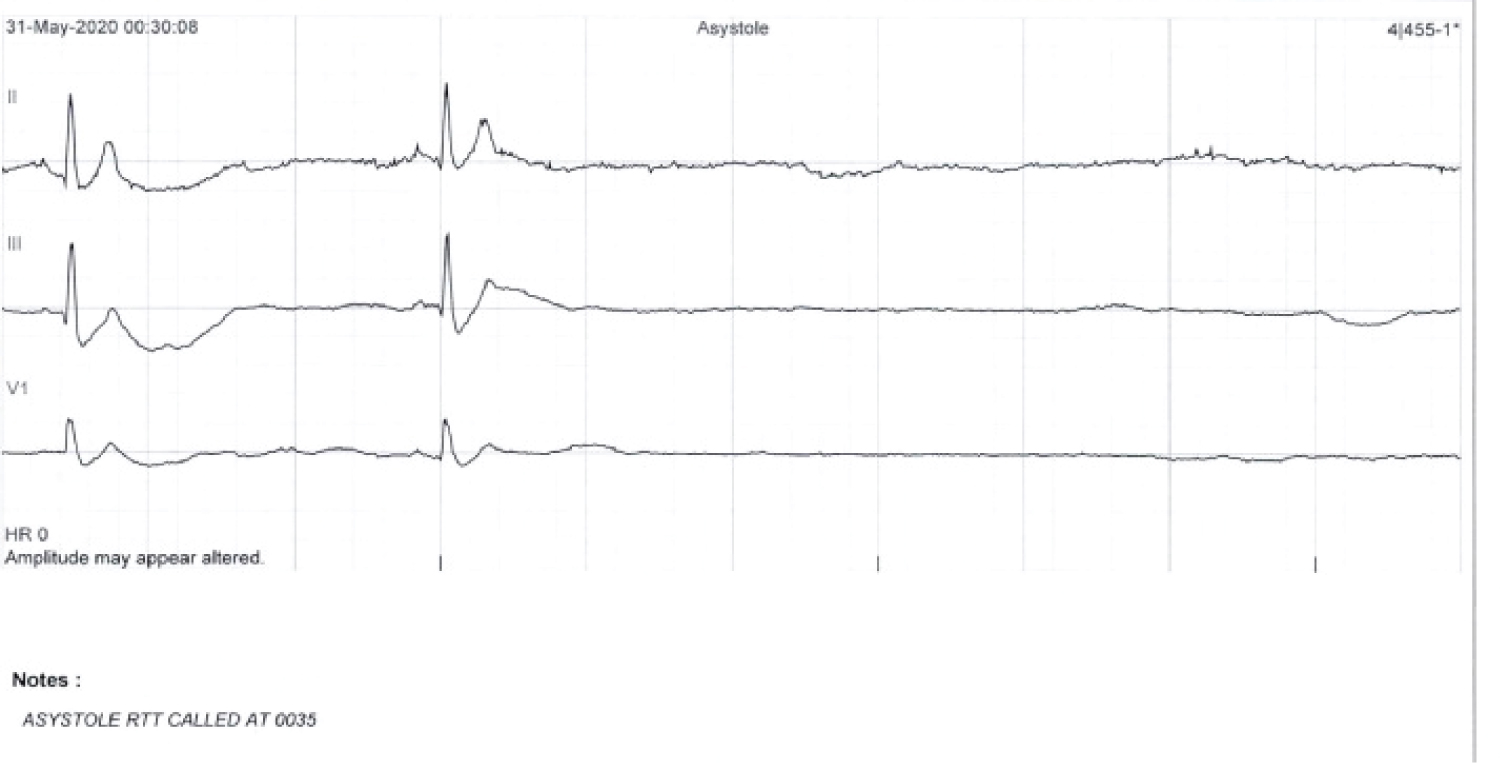 Figure 3A: In-hospital telemonitor demonstrates asystole during patient's syncopal episode.
View Figure 3A
Figure 3A: In-hospital telemonitor demonstrates asystole during patient's syncopal episode.
View Figure 3A
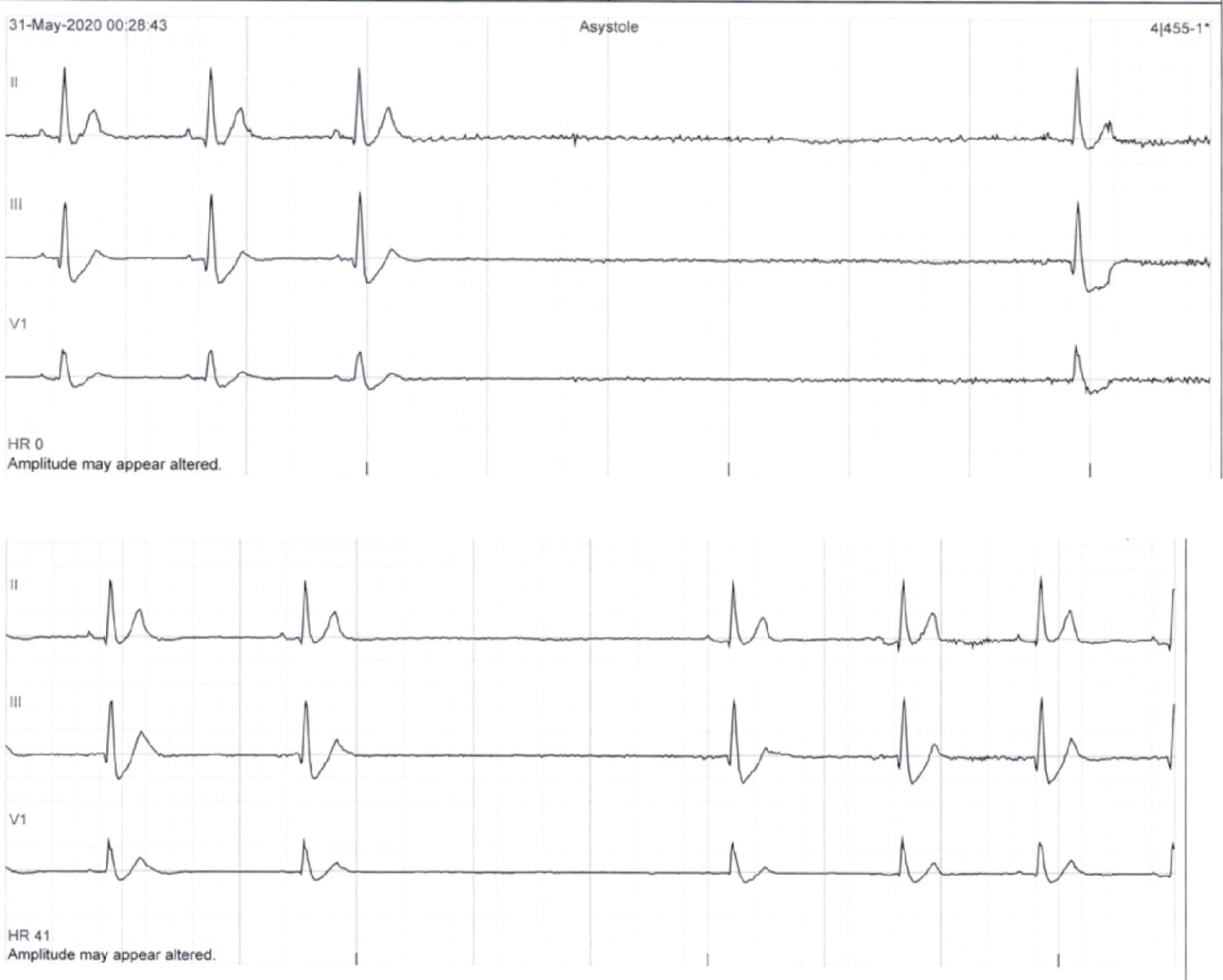 Figure 3B: In-hospital telemonitor demonstrates sinus pauses.
View Figure 3B
Figure 3B: In-hospital telemonitor demonstrates sinus pauses.
View Figure 3B
 Figure 4: Holter monitor strip demonstrates sinus pause.
View Figure 4
Figure 4: Holter monitor strip demonstrates sinus pause.
View Figure 4
Brugada syndrome (BrS) is a well-known arrhythmogenic entity associated with a risk of sudden cardiac death (SCD) due to ventricular fibrillation. It is characterized by a pseudo-right bundle branch block pattern on ECG with ST elevations in V1 and V2 that are either "coved" as in type 1 or "saddle back" as in type 2 (Figure 1). The diagnosis of a syndrome is made based on the presence of the ECG pattern and the clinical presentation which may manifest as syncope or SCD; classically attributed to ventricular arrhythmias and specifically polymorphic ventricular tachycardiac originating from the right ventricular outflow tract [1]. Supraventricular tachycardia and atrial fibrillation have been linked to BrS with an estimated incidence of 10-13% [1-3]. Sinus node dysfunction (SND) in patients with Brugada has also been described and reported in the literature; but remains clinically a less recognized and identified presentation.
In 2005, evidence of SND in a young patient with BrS who died suddenly was illustrated on autopsy which revealed deposition of fatty tissue, atrophy and fibrosis of the sinus node [4]. A study by Bordachar, et al. of 59 asymptomatic patients demonstrated that 17% of them had SND induced during electrophysiology study [2]. Clinically documented SND in patients with BrS was estimated to be 1.1-1.7% in large population studies [5,6]. The prevalence of SND in children with BrS was higher than that in adults reaching 7.5%-9.0% [7,8].
Up to 20 different genetic mutations have been associated with BrS, including mutations in genes encoding sodium channel, calcium channels and potassium channels, and proteins affecting ion channels [9]. Interestingly, mutations in the cardiac predominant sodium channel α-subunit SCN5A which accounts for 20-30% of patients with Brugada, has been linked to SND [9-12]. The abnormal sodium channel is thought to prolong the action potential of sinus node cells, slow depolarization and as a result contribute to SND [13]. An overlap syndrome of cardiac sodium channelopathy including BrS, conduction disease and long QT syndrome has been proposed and linked to mutations in the gene encoding for SCN5A [14,15].
SND has been identified in patients with BrS as a risk factor for arrhythmic events [5,6]. In a study of 116 adult family members of whom 60 of them were carriers of a mutant SCN5A gene, a possible bradycardic mode of death was suggested with a carrier of the gene who suffered from sinus arrest > 9 seconds [13]. Although we are unable to determine the underlying rhythm that leads to our patient's first out-of-hospital syncopal event, his subsequent in-hospital syncopal event was due to a recorded 12 second sinus arrest. In fact, the patient proceeded to have multiple more episodes of sinus pause that were documented during his hospital stay and after discharge. Unfortunately, these episodes were identified after his subcutaneous ICD was already placed for a presumed ventricular arrhythmogenic cause of his presenting syncope. The patient declined pacemaker placement during the index hospitalization and elected to continue to monitor his rhythm and symptoms using an event monitor and to further discuss the placement of a pacemaker in the outpatient setting. The recognition of the possible overlap of BrS and SND is important in management and decision making. Given this association, we recommend avoiding the placement of SQ ICD which may necessitate future procedures such as the placement of a pacemaker or transvenous ICD and the removal of SQ ICD in the event that sinus node dysfunction is to develop.
Sinus node dysfunction is an underrecognized entity in patients with Brugada syndrome or pattern. It is imperative that providers and cardiologists are aware of this association which is likely related to common genetic mutations leading to an overlap syndrome. Consideration of SND in patient with BrS should be taken into account when making decisions in regard to management and device therapy.
None.
We have no relationship with industry to declare.
All authors contributed to the writing and review of the manuscript.