Many patients seek dental offices for a beautiful, harmonious smile to boost their self-esteem. At present, there is a great search for oral aesthetics, where the harmony of the smile is determined not only by the shape, position, and color of teeth but also by the gingival tissue. The present study aimed to establish the etiology and diagnosis of the gingival smile, with the alternative of correcting it with very safe surgical techniques such as gingivectomy. The procedure consists in the elimination of gingival deformities resulting in a better gingival contour. Usually, surgical removal of 1 to 2 millimeters of gingival tissue solves most cases of the gingival smile. The surgical technique has the possibility to perform the incision with a conventional scalpel, electrosurgery (electric scalpel) and there are also the high-frequency lasers, being a choice obtained during the treatment plan and in patient-professional harmony, for each case. The literature review was carried out through the selection of articles related to etiology and diagnosis of gingival smile and periodontal surgery, focused on gingivectomy. With this, it is concluded that, based on technical and scientific knowledge, gingivectomy promotes essential visibility and access to a complete removal of superficial irritant deposits and perfect root straightening.
Gingivectomy, Gingival hyperplasia, Periodontics, Periodontal health
Many patients seek dental offices for a beautiful, harmonic smile to boost their self-esteem [1,2]. At present, there is a great search for the buccal aesthetics, where the harmony of the smile is determined not only by the shape, position, and color of the teeth, but also by the gingival tissue, and can be corrected with surgical techniques such as gingivectomy.
Gingivectomy is a technique that is easy to carry out and is usually well accepted by patients, who, according to the correct indications, can obtain satisfactory results in dentogingival aesthetics and harmony [3].
The procedure consists in the removal of gingival deformities resulting in a better gingival contour, it can be performed in the removal of the inserted, papillary and marginal gingiva when there is an absence of periodontal disease [4].
However, it may be indicated for clinical crown augmentation or remodeling of thick margins, removal of hyperplasias caused by a variety of factors, or even removal of supra-bony periodontal pockets [5-7].
The present study aimed to establish the etiology and diagnosis of the gingival smile, with the alternative of correcting it with very safe surgical techniques such as gingivectomy.
Following the criteria of literary search with the use of the Mesh Terms that were cited in the item below on "Search strategies", a total of 34 papers that were submitted to the eligibility analysis were collated and, after that, 24 studies were selected (Figure 1).
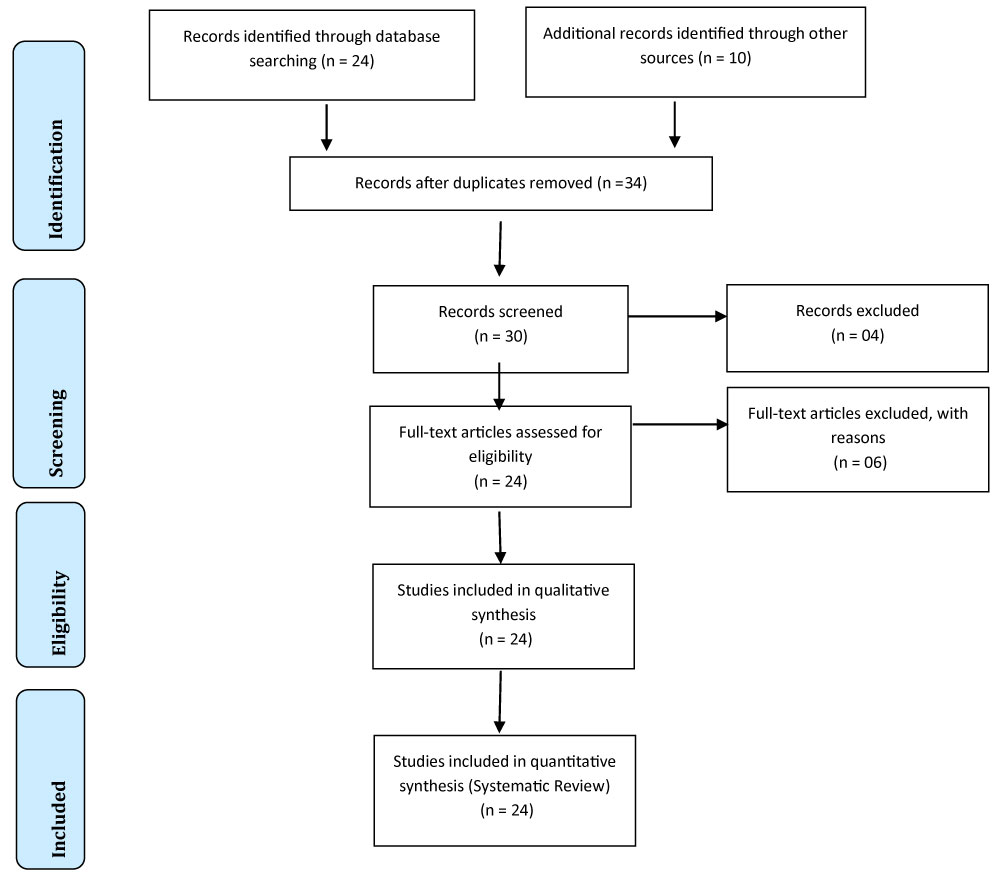 Figure 1: Flow chart.
View Figure 1
Figure 1: Flow chart.
View Figure 1
In general, as an example, the search strategy in MEDLINE/Pubmed, Web Of Science, Science Direct Journals (Elsevier), Scopus (Elsevier), OneFile (Gale) followed the following steps:-Search for mesh terms: Gingivectomy, Gingival Hyperplasia, Periodontics, Periodontal Health, and use of the bouleanos "and" between mesh terms and "or" among historical findings.
The healthy gingiva is represented by specific clinical features such as pink-pale color, matte and dotted surface, firm and resilient consistency, volume-dependent shape and gingival contour being the thin margin and ending against the tooth like a knife blade. When subjected to the periodontal probe, its depth may vary from 1-3 mm and should not present bleeding to this examination [8].
Hyperplasia resulting from the failure of oral hygiene is one of the most common complications in relation to gingival increases since the accumulation of biofilm from food remains causes the proliferation of inflammatory cells and pathogenic bacteria, causing the gingiva to present edematous, color reddish, loose and with chances of spontaneous bleeding [3].
There are risk factors that may predispose to gingival hyperplasias, such as the use of orthodontic appliances or medications, but their development is directly linked to deficient hygiene, causing space for dental biofilm installation, which is the etiological agent of the great majority of periodontal problems [4].
The implantation of dental appliances facilitates gingival inflammation and has great influence on the oral microbiota, but these conditions are subjects of reversion in people who have an adequate oral hygiene [5].
The presence of periodontal pockets is detected through the depth of probing. To do this, the clinical insertion level of each patient is measured to analyze the periodontal biological space, which includes gingival sulcus (0.69 mm), junctional epithelium (0.97 mm), that is, taking into account that in the natural state it presents from 2 to 3 millimeters of healthy structure that extends from the alveolar bone crest to the gingival margin [6].
After gingival hyperplasia is observed, surgery is usually indicated for treatment, the ideal is always to be associated with basic periodontal therapy, and after performing scaling and root planning, the adequacy of the buccal environment, with elimination of all the outbreaks of infection seeking to awaken the patient through the instructions of oral hygiene, care and concern with oral health, being this phase more important of the treatment to obtain a healthy gingival condition [9].
In general, surgical removal of 1 to 2 millimeters of gingival tissue resolves most cases of a gingival smile, but when gingiva at a height is very significant, more complex surgery should be performed [7].
While performing the surgical technique, one has the possibility to perform the incision with the conventional scalpel or elect electrosurgery (electrosurgical scalpel), although the former is the most used and most preferably among the professionals, both reach the same satisfactory aesthetic results, being a choice obtained during the treatment plan and in patient-professional harmony, for each specific case [9].
After the preparation of the surgical field and oral antisepsis, local infiltrative anesthesia is performed and bleeding points are marked, both buccally and lingually. To determine the bleeding points and thus the gingival portion to be removed, the depth of probing is marked with a probe millimeter with the aid of an explorer [9].
Thus, the union of these points is performed with Kirkland gingival, the literature also describes the use of a blade 15c connected to a scalpel handle and also with the use of electric scalpel to perform this step, and for the interproximal areas is the Orban gingival, and sometimes a McCall 13/14 curette may be used to remove gingival tissues, dental calculi or dental biofilm [8,10,11]. After removal of the gingival collar, gingivoplasty is performed using a Kirkland gingivectomy and cuticle pliers at the surgery site in order to improve aesthetics by favoring tissue repair and restoring a functional gingival shape, being that is covered with surgical cement for protection and favoring tissue repair [12-15].
There are also high-frequency lasers such as carbon dioxide laser, which can be used in the transoperative to remove the gingival collar because it has long wavelengths, is better absorbed by tissues with large tracts of water, evaporating more easily and providing removal of the gingiva without causing deep burns, replacing the use of conventional scalpels [16-19].
Carbon dioxide laser stimulates blood clotting in small blood vessels, allowing it to work in a controlled area, being indicated for very vascular areas and in patients in whom infection control is critical, since the laser has the capacity to transform an area contaminated or infected in a sterile wound [19,20], also inhibiting the formation of abnormal cells, by the lining of lymphatic vessels, in addition to little contraction, scar formation, usually does not require surgical cementation, nor suture and the pain remains for only a few seconds after surgery, generating little discomfort in the postoperative period allowing the patient to return to normal activities [21,22].
The first step in establishing a correct diagnosis is to properly classify the gingival level, taking into account variables such as gender, age and periodontal health [3,12,13]. The causes defined for gingival growth can be characterized by numerous factors (orthodontic reasons, maxillary growth, drug-induced, pathologies) and aggravated according to factors such as age, gender, hygiene and systemic condition of the affected patient [14].
After the literature review in this study, it can be concluded that gingivectomy promotes essential visibility and access to a complete removal of irritating superficial deposits and perfect root straightening. One of the great advantages that gingivectomy provides is the transformation of a periodontal pocket of difficult hygiene into an easily hygienizable gingival sulcus. Contraindications for gingivectomy are based on existing local conditions and the patient's physical health. Laser therapy has been used successfully for gingivectomy treatments. The main disadvantages are the high cost of the apparatus for use in dental clinics.
There is no conflict of interest between authors.