Mesenteric cysts are rare abdominal masses that can present with varied clinical manifestations, including partial intestinal obstruction. We present a case of a 17-year-old boy with no significant medical history who exhibited chronic abdominal pain, fluctuant abdominal swelling, constipation, loss of appetite, and bilious projectile vomiting. Previous history of blunt trauma to the hypogastric region at age 10 was noted. Laboratory investigations showed elevated white blood cell count, neutrophilia, and elevated alkaline phosphatase. Imaging studies including abdominal ultrasound and CT scan revealed a large cystic mass in the midline and hypogastric regions, displacing surrounding organs. The patient underwent surgical intervention with a transverse colectomy to remove the mesenteric cyst, which was found adhered to the transverse colon. Postoperatively, the patient recovered well with early ambulation, return of bowel sounds, and toleration of oral intake. This case highlights the importance of considering mesenteric cysts in the differential diagnosis of abdominal masses presenting with symptoms of partial intestinal obstruction, and the successful management through surgical intervention.
Mesenteric cysts encompass a diverse range of cystic lesions found in the abdominal cavity or retroperitoneum, presenting as rare intra-abdominal entities with reported incidences of 1 in 100,000 in adults, 1 in 20,000 in children, and a female-to-male ratio of 2:1 [1]. A set of distinctive characteristics was identified by the French surgeon Paul Jules Tillaux, which includes a swelling near the belly button that can move freely in a direction perpendicular to the mesentery's attachment. When tapped, a resonant sound is produced over the bowel loop in front of the cyst, while a dull sound is heard behind it due to the presence of fluid within the cyst. The occurrence of this triad ranges from 1 in 100,000 to 250,000 cases [2]. The origin of these cysts is presumed to be congenital or due to trauma, resulting in ectopic lymphatic vessel proliferation within the mesentery without connection to the lymphatic system [3]. Typically, asymptomatic due to their size and location, mesenteric cysts are often incidentally discovered during routine imaging. Common symptoms, ranging from 55% to 81% of cases, include nonspecific abdominal discomfort, palpable masses (44%-61%), abdominal distension (17%-61%), nausea, vomiting (45%), constipation (27%), and diarrhea (6%) [4]. Alternatively, individuals could initially present with sudden gastrointestinal symptoms like severe abdominal pain, stemming from complete bowel blockage, peritonitis, or volvulus, necessitating immediate surgical intervention in the emergency setting [5]. Recurrence rates following complete surgical excision via laparoscopic or open methods are minimal, despite various theories on cyst growth mechanisms [6]. The primary treatment for mesenteric cysts involves complete surgical removal, with a low likelihood of recurrence post-surgery [7]. The mortality rate of surgical excision for mesenteric cysts is 9%. However, if resection of a bowel segment is required, the mortality rate triples [8]. This article aims to raise awareness of mesenteric cysts, particularly when there is suspicion of partial intestinal obstruction.
A 17-year-old boy, without any known underlying health conditions or current medication use, presented with chronic and diffuse abdominal pain. He exhibited fluctuant abdominal swelling near the umbilicus with clearly defined margins and a dull sound upon percussion. Other accompanying symptoms included constipation, loss of appetite, and bilious projectile vomiting. Notably, the patient did not report any urinary issues or other associated constitutional symptoms and denied any contact with cattle or farming.
The patient reports experiencing a gradual swelling following blunt trauma to the hypogastric area, which was initially addressed at a nearby national hospital three months before seeking admission to our facility. Subsequently, he was discharged with prescriptions for stool softeners and antiemetics to manage his condition. The abdominal ultrasound revealed a sizable, well-defined cystic mass that encompassed the epigastric region, extending into both the left and right hypogastric quadrants. Within the cystic mass, a mobile echogenic material was observed. Additionally, no internal vascularization was detected during doppler interrogation. The computer tomography (CT) scan of the abdomen and pelvis displayed a significant finding of a large cystic lesion measuring 19.5 × 10.9 × 14 cm in the hypochondrial and midline areas. The lesion exhibited a thin wall and mild marginal enhancement, resulting in the displacement of the stomach anteriorly and the pancreas posteriorly. Notably, the lesion smoothly indented the head of the pancreas and the left hepatic lobe. The diagnosis based on both studies confirmed the presence of a mesenteric cyst (Figure 1). The patient was kept on 10% dextrose before surgery. The patient underwent general anesthesia followed by an extended midline incision (Figure 2). The abdomen was meticulously opened in layers, revealing the anterior displacement of the stomach. A careful dissection of the gastrocolic area was performed, with the stomach deflected anteriorly. Subsequently, a large cystic mass located posterior to the stomach was identified. This mass was covered by the anterior leaf of the greater curvature, indenting the pylorus of the stomach, left lobe of the liver, head of the pancreas, and the transverse colon (Figure 3). The mucosa of the transverse colon was adhered to the cysts, necessitating a transverse colectomy procedure (Figure 4). This involved careful blunt dissection and unroofing of the cyst, which was causing indentations on the liver and pancreas. Subsequently, the contents of the cyst were aspirated (Figure 5), followed by the complete removal of the cyst, which was thin-walled and lacked a muscular coat (Figure 6 and Figure 7).
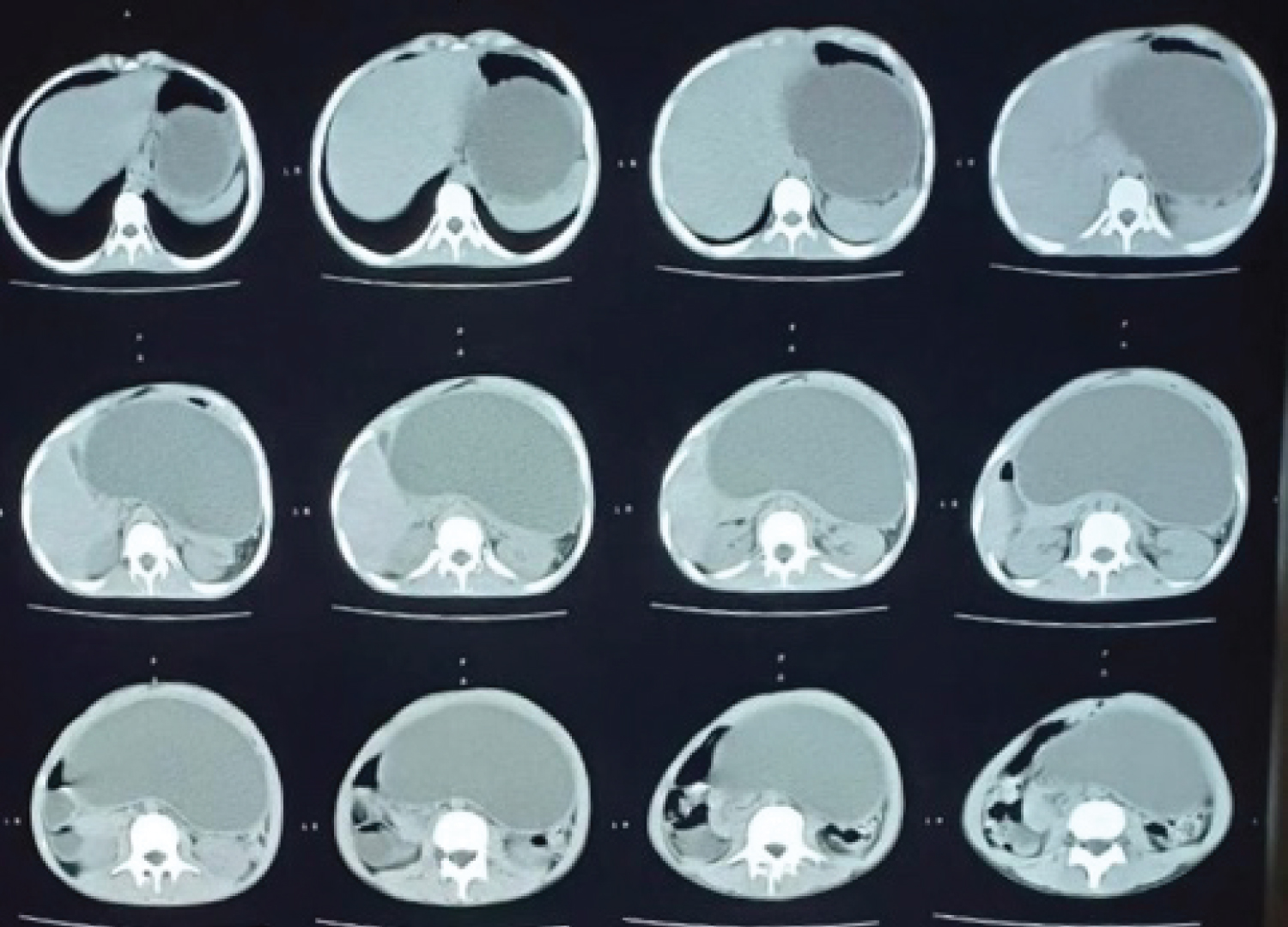 Figure 1: Large hypochondrial and midline cystic lesion.
View Figure 1
Figure 1: Large hypochondrial and midline cystic lesion.
View Figure 1
 Figure 2: Extended midline incision.
View Figure 2
Figure 2: Extended midline incision.
View Figure 2
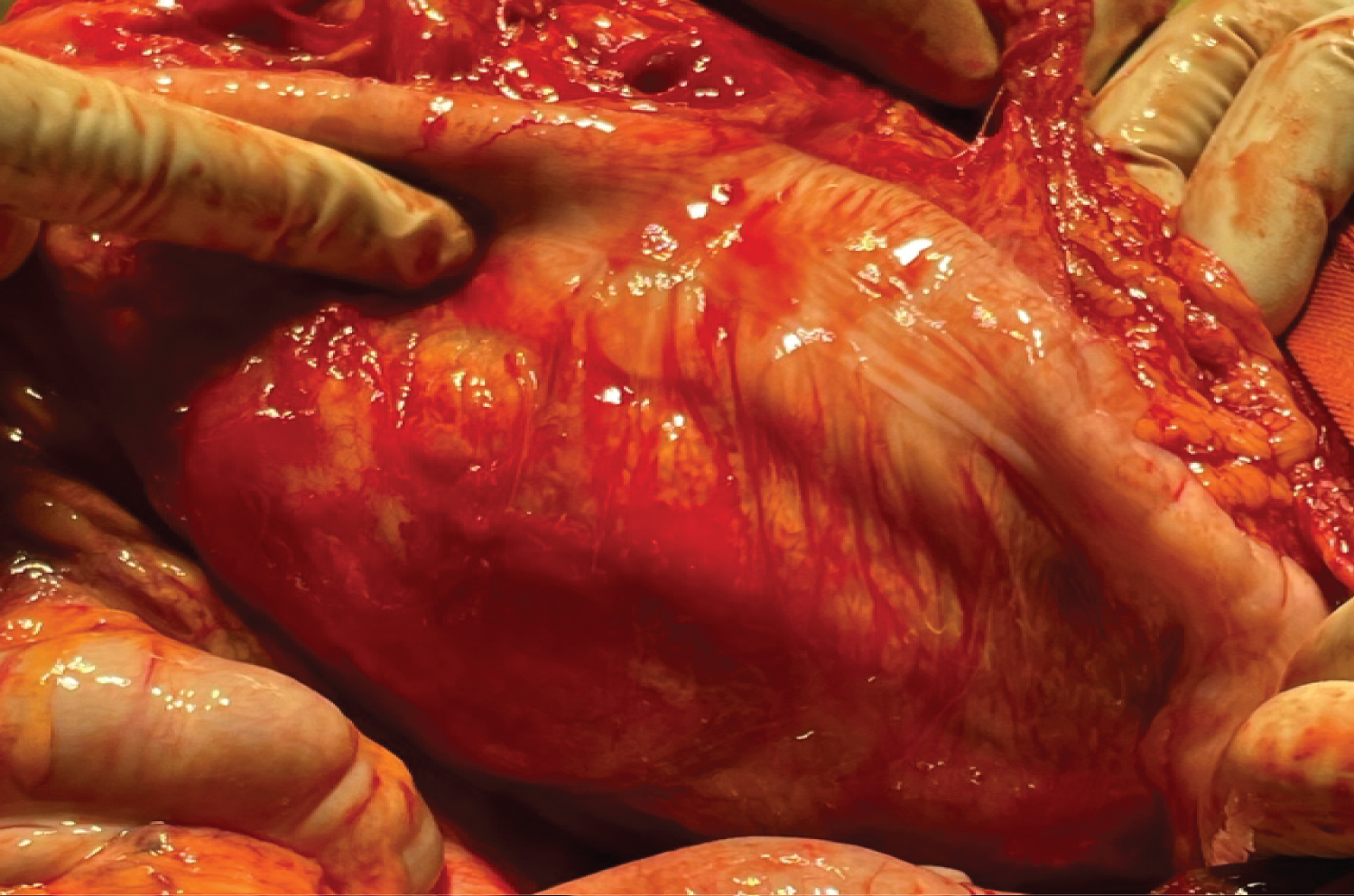 Figure 3: Cystic mass between the mesentery indenting the transverse colon.
View Figure 3
Figure 3: Cystic mass between the mesentery indenting the transverse colon.
View Figure 3
 Figure 4: Transverse hemicolectomy, anterior view showing the adhered side of the cyst to the mucosa of the transverse colon.
View Figure 4
Figure 4: Transverse hemicolectomy, anterior view showing the adhered side of the cyst to the mucosa of the transverse colon.
View Figure 4
 Figure 5: Draining the cyst.
View Figure 5
Figure 5: Draining the cyst.
View Figure 5
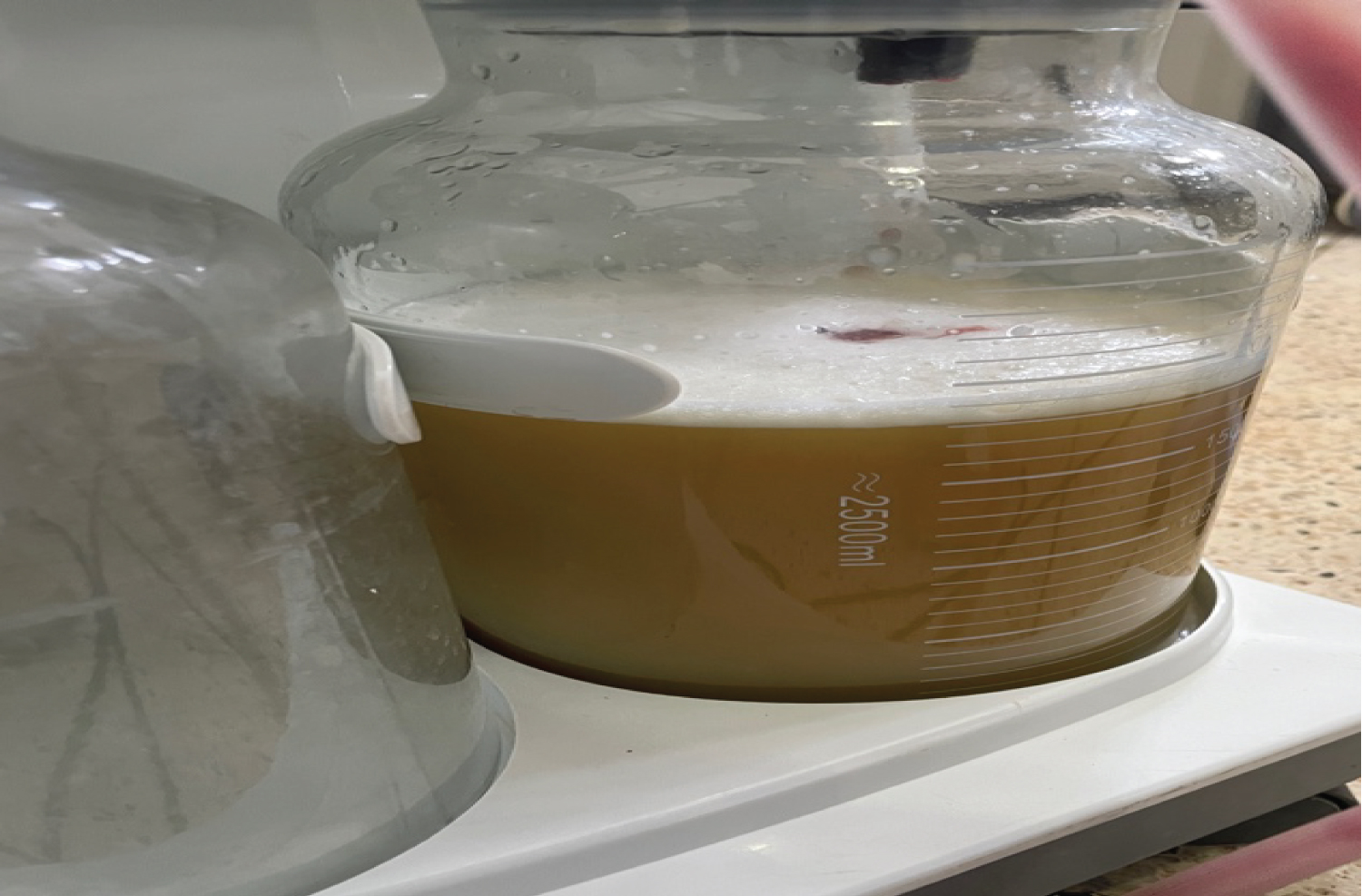 Figure 6: Chylus content suctioned from the cyst.
View Figure 6
Figure 6: Chylus content suctioned from the cyst.
View Figure 6
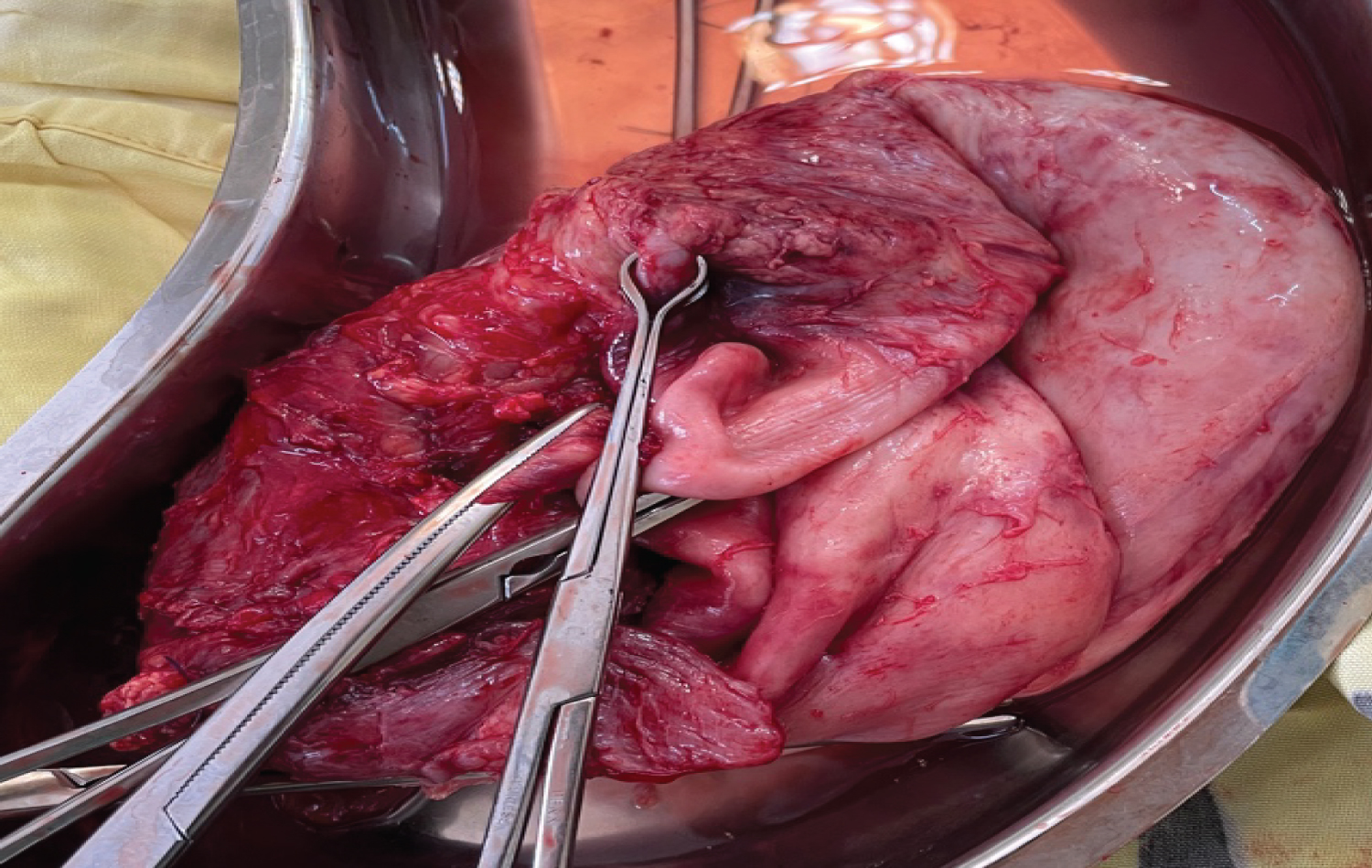 Figure 7: Thinned wall with no musculature coat mesenteric cyst.
View Figure 7
Figure 7: Thinned wall with no musculature coat mesenteric cyst.
View Figure 7
Postoperatively, the patient's recovery progressed smoothly without any notable complications. Ambulation began 8 hours after the operation, audible bowel sounds were present 12 hours post-op, and the patient tolerated semisolids within the same timeframe. Subsequently, the passage of flatus and stool occurred 24 hours post-op, indicating a successful recovery process (Table 1).
Table 1: Laboratory indices. View Table 1
Mesenteric cysts are a rare type of abdominal cysts [9], that can develop anywhere from the duodenum to the rectum, with the small bowel mesentery, particularly the ileum, being the most common location (66%). The large intestine, specifically the transverse and ascending colon, accounts for about 33% of mesenteric cysts [10,11]. Understanding the cyst's relationships with surrounding structures is crucial for accurate localization. While imaging tests and symptoms can assist in diagnosing mesenteric cysts, they may not always provide definitive results, especially since pseudocysts, another common type of abdominal cysts, can exhibit similar features.
The clinical manifestations of mesenteric cysts are often nonspecific and can vary widely among individuals. Symptoms reported include intestinal blockage, gastroesophageal reflux, esophagitis, urinary incontinence, pancreatitis, and obesity [3,12-14]. The size of the cyst is linked to the duration and extent of lymphatic blockage or the accumulation of lymphatic fluid within the cyst [15]. Symptoms experienced are dependent on the cyst's pressure on neighboring organs; a large cyst can compress nearby organs, leading to organ-specific symptoms and complicating diagnosis [16]. Evaluating the size of the symptomatic cyst is challenging, as its presentation is influenced by its location and the impact on adjacent organ function [17,18].
The surgical treatment for mesenteric tumors involves complete excision either through laparoscopy or laparotomy [2,19-29]. The choice of surgical approach depends on factors such as cyst size, location in the peritoneal cavity, and surgeon expertise [29]. In some cases, intestinal resection may be necessary for complete excision [2,21-23,27,29]. Even in malignant cases, enucleation is often effective with a high cure rate [2]. Marsupialization is considered if other surgical options are not feasible [2,23]. Partial excision is linked to recurrence and complications, while simple drainage is avoided due to high mortality and recurrence rates [2,20,23,25,28]. Recurrence of cysts is more likely with retroperitoneal locations due to the technical challenges in excision [23].
In this case, the patient had symptoms resembling intestinal obstruction and pressure sensations for over 7 years. Initially, the symptoms were associated with blunt abdominal trauma, but no specific organ involvement was identified. Pain relief was the primary management strategy. Surgical removal of mesenteric cysts is typically recommended. However, in this particular instance, the cyst's location, pressing on the liver, pylorus, and pancreas, required a transverse hemicolectomy for drainage and complete excision. The surgery was complicated due to the extensive spread of the cyst, which led to anatomical distortion and adhesions, making it challenging to differentiate between the cyst and the colon's surface. As a result, the team opted to drain the cyst cautiously before proceeding with complete removal. The presence of fibrosing lesions further supported the link between the cyst and the past trauma. This case highlights the complexities involved in managing mesenteric cysts, particularly when the cyst's extension causes anatomical distortion and complicates surgical excision.
Mesenteric cysts often present with nonspecific symptoms; however, preoperative diagnosis is feasible by determining the cyst's location relative to surrounding structures. The initial diagnosis relies on a thorough assessment of the patient's symptoms and imaging studies, with MRI being the most accurate investigation. Surgical excision is the optimal approach for treating mesenteric cysts, with minimally invasive surgery being the preferred choice.
Salim Mzee, Mohammed M.M Ali, Cosmos Mutisya, and Zakari Shaibu, made substantial contributions to the reporting of the work. All authors were actively involved in reviewing relevant literature, drafting the manuscript, and revising the final draft. Material preparation, data collection, and data analysis were carried out by Swalah suleiman salim Al-Busaidy, and Isah Adamu Danbala and Arnold Kiptoo mutai. Said Abdulrahman Salim Mzee authored the initial draft of the manuscript, while Zakari Shaibu revised and proofread it. All authors provided feedback on earlier versions, and the final manuscript has been reviewed and approved by all.
None.
The authors state that they do not have any competing interests.
Consent was obtained from participant involved in the study, or it was waived in accordance with ethical standards.