Malignant pleural mesothelioma is a rare neoplasm that mostly occurs in elderly men. Recurrent unilateral pleural effusion is the most typical presentation and it is very rare to find extra-thoracic lymphadenopathy before the primary tumor, even in advanced cases. Herein, we report a challenging case of a young man presenting with unresolved fever, sore throat, and dysphagia associated with massive pleural effusion, cardiac tamponade, and multiple cervical lymphadenopathy with mesothelial cells infiltration. Microscopic examination of lymph node structures revealed reactive follicular architecture and massive infiltration of epithelioid cells with pleomorphic vesicular nuclei in the sinuses and subcapsular spaces. Immunohistochemical staining of the epithelioid cells demonstrated a positive reaction to PAN-Cytokeratin (CK), CK7, calretinin, Wilms tumor (WT1), and CK5/6 while Ki-67 labeling index showed low proliferative activity. Biopsy of pericardium and fluid cytology revealed no evidence of malignancy. The patient underwent a second surgery due to unresolved effusion. Sample taken from the anterior mediastinal area showed infiltrating tubulo-glandular proliferation spreading to mediastinal fat component. Thereafter, the diagnosis of malignant mesothelioma originating from mediastinal reflections of the pleura was established. It is very important for the pathologist to accurately diagnose malignant mesothelioma over other differential diagnoses to prevent misdiagnosis in such rare and complicated cases.
Malignant mesothelioma, SVC syndrome, Intranodal mesothelial cell inclusion, Immunohistochemistry
Malignant mesothelioma is a rare fatal neoplasm of mesothelial surfaces of body cavities [1-3]. Malignant pleural mesothelioma mostly occurs in elderly men [1]. Usual clinical presentations include dyspnea, chest pain, and symptoms that are related to the site and amount of effusion [2,4]. The most typical presentation is recurrent unilateral pleural effusion and, pericardial involvement is uncommon. On top of that, it is rare to find peripheral extrathoracic lymphadenopathy or distant metastasis before the primary tumor [1,5,6].
We are going to present a case of a young male patient with malignant pleural mesothelioma and massive pleural and pericardial effusion. Recognition of this rare and complicated entity is important to prevent misdiagnosis in such cases.
A 33-year-old non-smoking male patient presented with fever, sore throat and dysphagia, received supportive medical treatment but, the symptoms did not resolve but deteriorated. The serologic evaluation revealed Epstein Barr virus infection based on 2+ positive monotest and high levels of EBV IgG and IgM. He experienced fullness in the face and neck region, palpated neck mass, and had shortness of breath. As his condition became chronic, he was examined more thoroughly by venography and was diagnosed with superior vena cava (SVC) thrombosis and SVC syndrome. Imaging studies namely chest X-ray and spiral chest CT scan were done and despite massive pericardial and bilateral pleural effusion, no mass lesion was found. The patient was not at risk due to his occupational and familial background; he only had a family history of factor V laden and the mutation was positive in his evaluation too. Due to massive pericardial effusion and signs of cardiac tamponade in echocardiography, surgical pericardiocentesis and pericardial biopsy were done. Multiple bilateral cervical lymphadenopathy was visualized and sampled during surgery. Patient follow-up after four months revealed unresolved pleural effusion and led to re-operation and thorough sampling of anterior mediastinal area.
The received specimen from the initial investigation designated as pericardial mass consisted of two brownish jugulodigastric lymph nodes measuring 2.2 and 1.5 cm in their greatest dimensions. Microscopic examination revealed lymph node structures with reactive follicular architecture and massive infiltration of epithelioid cells in the sinuses and subcapsular spaces (Figure 1 and Figure 2). The epithelioid cells were arranged individually and in clusters, containing relatively pleomorphic vesicular nuclei with conspicuous nucleoli. The cells had abundant amphophilic cytoplasm with distinct cell borders, some showing binucleation and nuclear irregularity. Immunohistochemical staining of the epithelioid cells demonstrated positive reaction with pan-CK, CK7, calretinin, WT1, and CK5/6. And evaluation for cluster of differentiation (CD) 20, CD3, CD68, CD1a, CD163, S100, leukocyte common antigen (LCA), CK20, thyroid transcription factor 1 (TTF1), CDX2, placental alkaline phosphatase (PLAP), CD30, Sal-like protein 4 (SAL4), activin receptor-like kinase 1 (Alk1) and alpha-fetoprotein were all negative. The Ki-67 labeling index showed low proliferative activity.
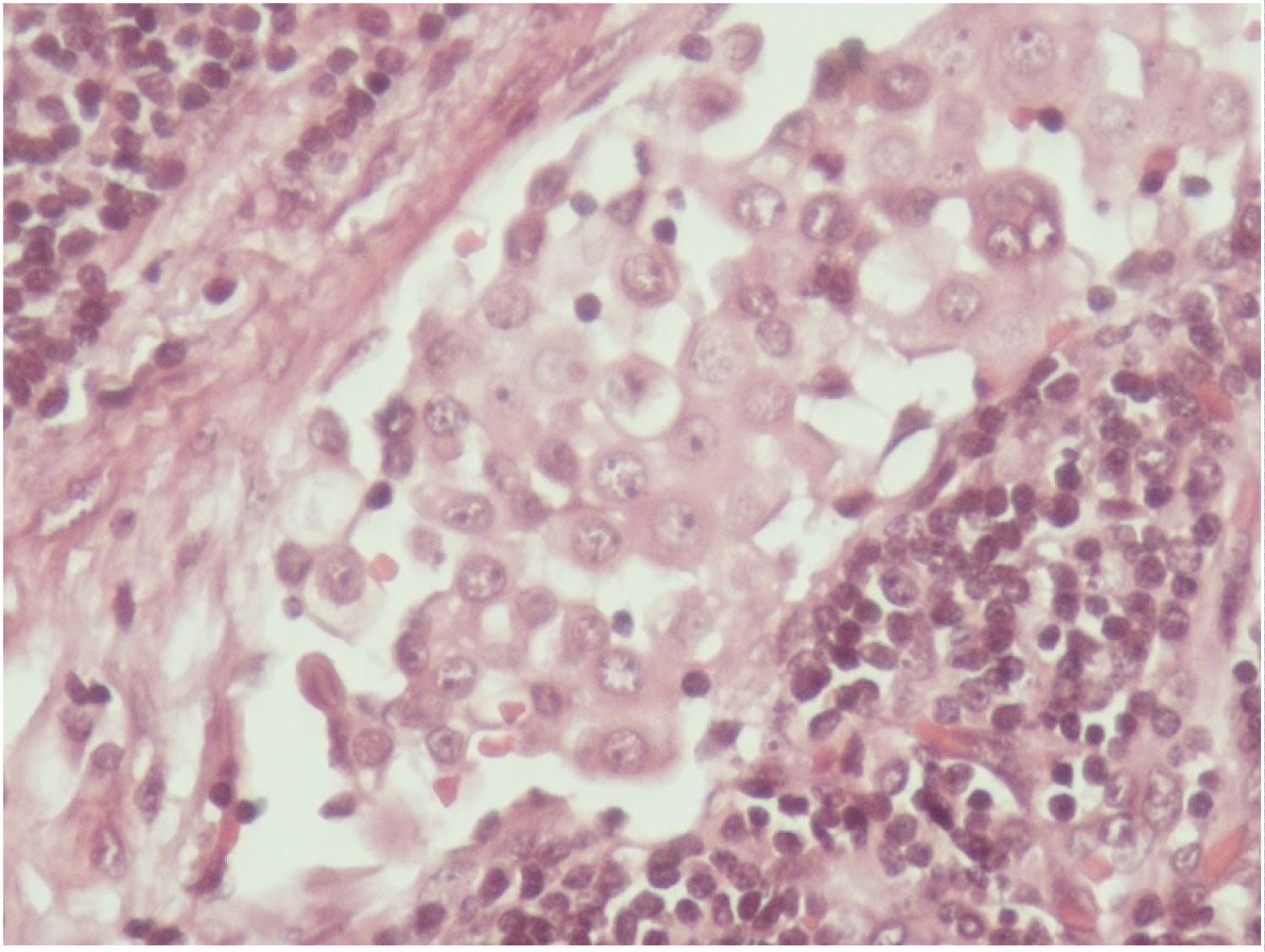 Figure 1: High power view of intrasinusoidal cells (hematoxylin and eosin staining, 400X). View Figure 1
Figure 1: High power view of intrasinusoidal cells (hematoxylin and eosin staining, 400X). View Figure 1
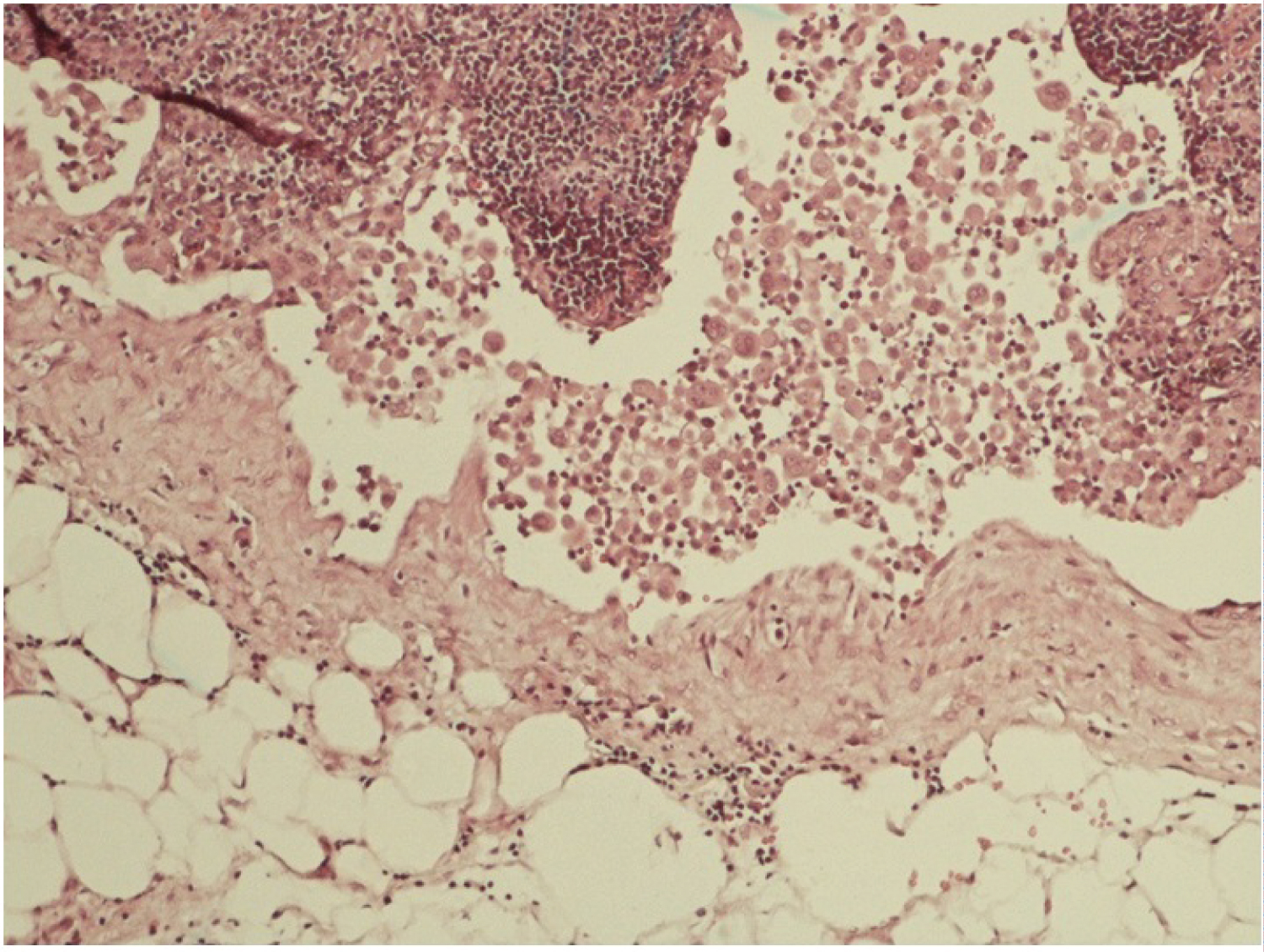 Figure 2: Mesothelial cells in subcapsular sinus of mediastinal lymph node (hematoxylin and eosin staining, 100X). View Figure 2
Figure 2: Mesothelial cells in subcapsular sinus of mediastinal lymph node (hematoxylin and eosin staining, 100X). View Figure 2
Histopathologic evaluation of the pericardial biopsy and pericardial fluid cytology revealed no evidence of malignancy. The pleural fluid was sampled and revealed signs of chronic inflammation and cytologic evaluation for malignancy was negative. The specimens were negative for abnormal shape or count of mesothelial cells. No fluid or mass was visualized in the peritoneal cavity in abdominal ultrasonography. In light of histologic findings and immunohistochemical profile, the diagnosis of reactive mesothelial cell inclusions in lymph nodes was made.
Four months after first observation, unresolved pericardial and pleural effusion and no mass lesion in imaging studies led to a second look surgery and meticulous search of the mediastinal area for the possible cause of unresolved pleural effusion. The samples obtained from the anterior mediastinal area showed infiltrating tubulo-glandular proliferations spreading to the mediastinal fat component (Figure 3 and Figure 4). The cells exhibited immunoreactivity panel as mesothelial cells and the diagnosis of malignant mesothelioma established.
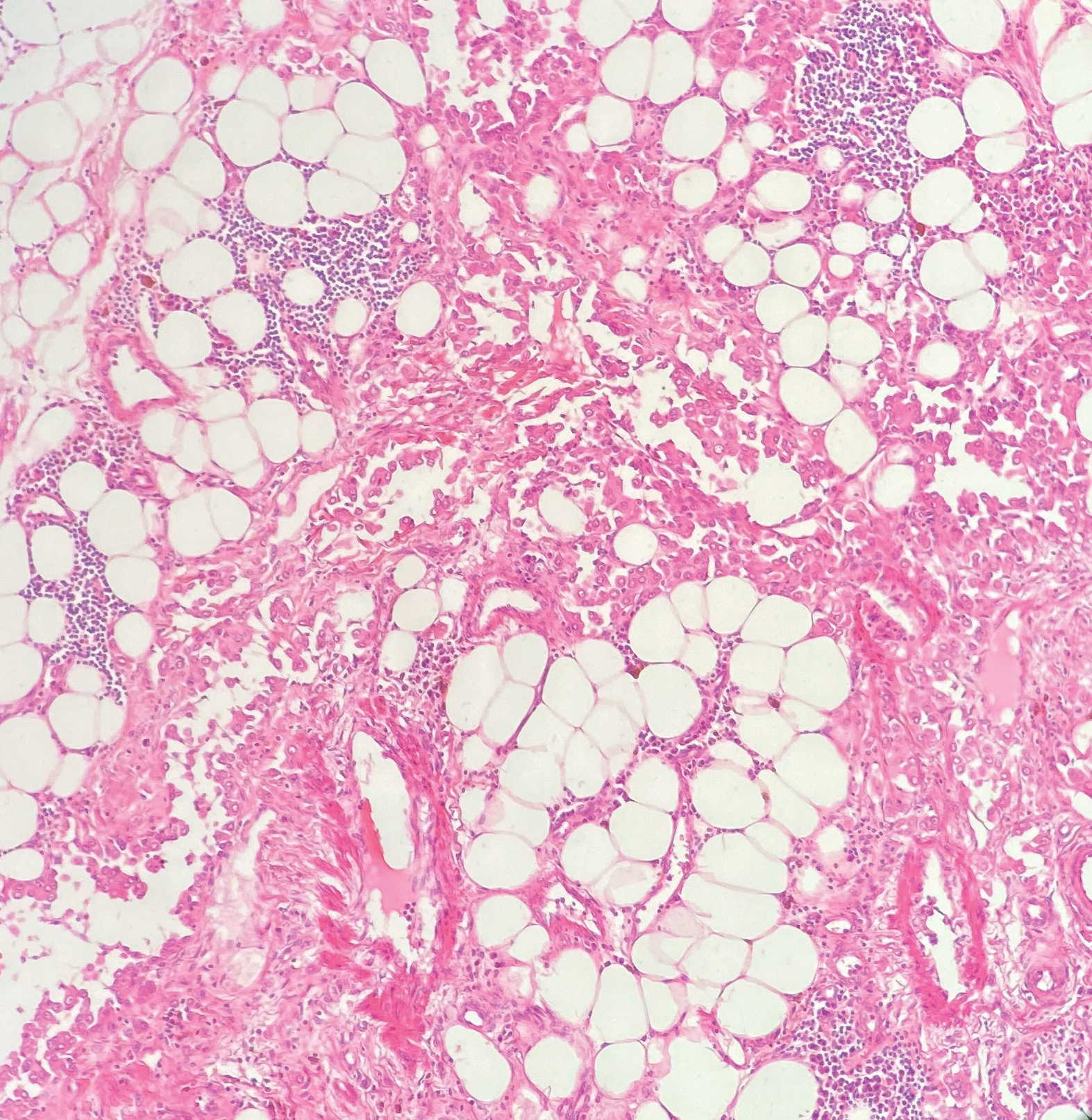 Figure 3: Low power view of tubular and glandular structures of mesothelial cells infiltrating mediastinal fat (hematoxylin and eosin staining, 100X). View Figure 3
Figure 3: Low power view of tubular and glandular structures of mesothelial cells infiltrating mediastinal fat (hematoxylin and eosin staining, 100X). View Figure 3
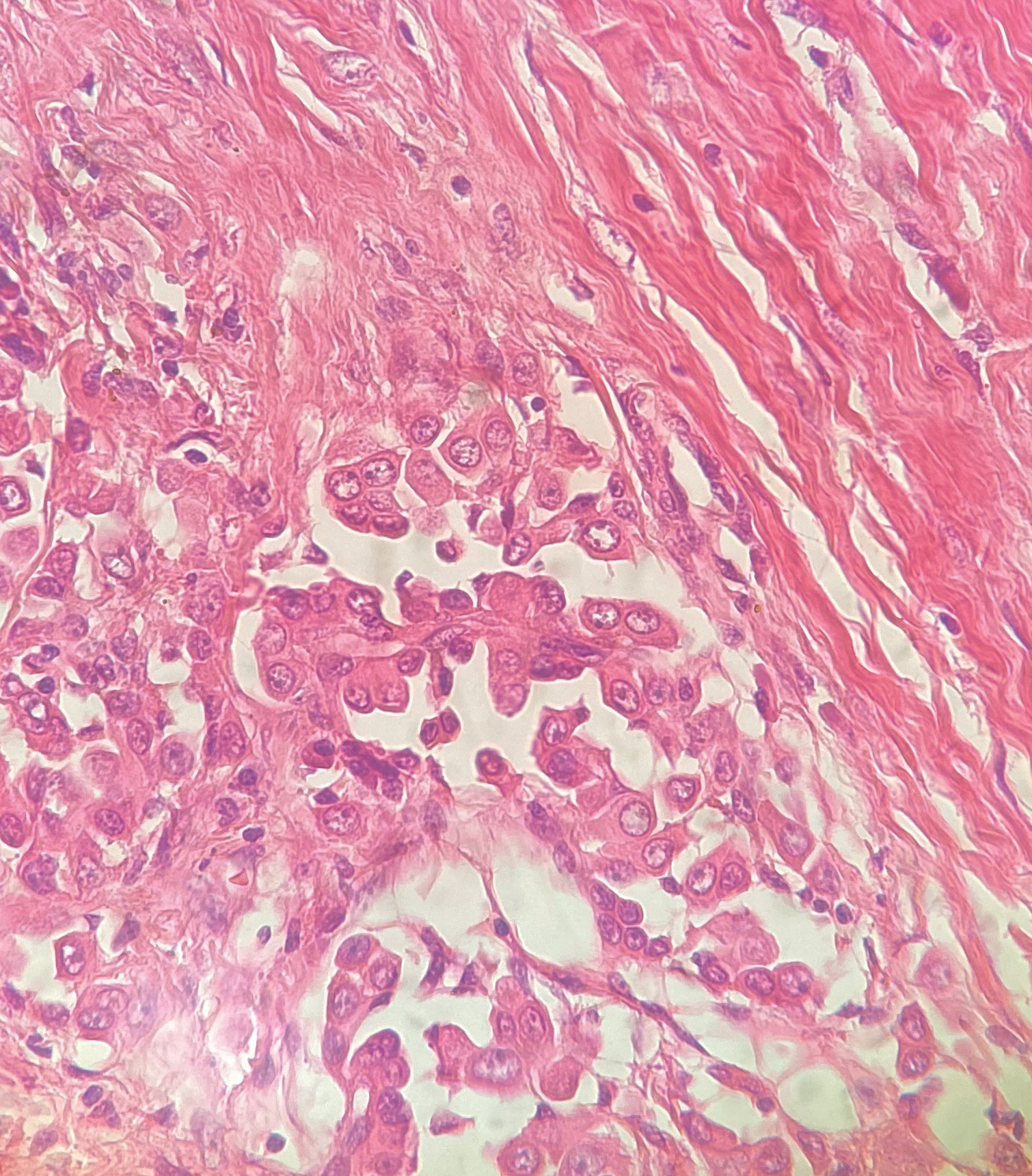 Figure 4: High power view of infiltrating mesothelial cells (hematoxylin and eosin staining, 400X). View Figure 4
Figure 4: High power view of infiltrating mesothelial cells (hematoxylin and eosin staining, 400X). View Figure 4
Malignant mesothelioma is a rare locally aggressive neoplasm of mesothelial surfaces of the pleural and peritoneal cavities, the pericardium, or the tunica vaginalis with a high mortality rate [1-3]. Based on recent studies, the incidence and prevalence of this tumor are rising these years, especially in Asia because of unregulated asbestos use [7,8]. Malignant pleural mesothelioma mostly appears in men with a median age of 74 years (in their 60s or 70s). However, based on recent reports, almost 15% of cases with malignant pleural mesothelioma were younger than the age 40 and it was equally found among men and women in the younger age group [2,4,9]. According to previous studies more than 80% of the patients are male and asbestos exposure history has been reported in more than 80% of patients [2,4,10]. In 1980 asbestos was widely abandoned as it was known as a strong risk factor for malignant mesothelioma [10]. Chronic exposure to silica and other chemicals, dust, SV40 virus and cigarette smoking are some of other contributing factors considered in previous studies [1,4,10]. The typical clinical presentations include dyspnea, chest pain, weight loss, and symptoms related to the site and amount of effusion [2,6,10].
It is very rare to find peripheral extra-thoracic lymphadenopathy before the primary tumor even in advanced cases [1,3,10]. Aggregation of mesothelial cells in lymph nodes or within the lumen of lymphatic vessels in histologic evaluations is considered indicative of malignant mesothelioma [11]. Infrequently, however, nonneoplastic intra-nodal mesothelial cells have been reported secondary to inflammatory and even neoplastic disorders other than malignant mesothelioma concerned to the serosal cavities [12]. Although malignant pleural effusion as a result of plasma extravasation and obstruction of pleural lymphatic outflow is the first clinical presentation of 90% of mesotheliomas, pericardial involvement is rare [13]. Usually, in pericardial involvement, direct tumor invasion is associated [10]. The most typical presentation is a recurrent unilateral pleural effusion which is sometimes exudative and hemorrhagic [5,6]. Parietal pleura involvement is more common than visceral pleura. Progression of malignant pleural mesothelioma is through local invasion into the mediastinum, parietal pleural fibrous tissue, extrapleural adipose tissue, and soft tissues of the chest wall and diaphragm [14]. Local invasion is a common occurrence and it can cause lymphadenopathy, SVC syndrome, vocal cord paralysis, Horner's syndrome, cardiac tamponade, and increased subcutaneous thickness [10,15]. Due to its hidden growth the tumor is found when it is relatively large or advanced in stage [15]. In 2015 Patra, et al. reported a case of mesothelioma accompanied by SVC obstruction as a rare presentation in an 18-year-old female. To our knowledge, very few examples of mesothelioma with SVC syndrome as presenting manifestations are reported [4].
It is not typical for malignant mesothelioma to present with paraneoplastic thrombosis in lymph nodes [1,10]. The basic problem with the presence of mesothelial cells in lymph nodes, is the diverse list of differential diagnoses; namely, sinus histiocytosis, benign intranodal mesothelial cell inclusion, metastatic carcinoma, and metastatic mesothelioma. The features that help to recognize benign mesothelial cells are their inherently benign appearance and absence of mitoses, parenchymal infiltration, and mesothelial windows showed by the CD34 staining pattern [16,17]. Their immune profile of positivity for CK AE1/AE3, CK7, calretinin, and negativity for CK20, TTF-1, and carcinoembryonic antigen (CEA) also establishes their mesothelial origin [17]. The cytokeratin-positive cells may represent either metastatic carcinoma, metastatic mesothelioma, or benign mesothelial cell inclusions [16]. Immunohistochemistry and morphological studies are used not only to prove mesothelial cell origin but also to distinguish benign from malignant mesothelial cell. A cytologic evaluation or biopsy of the questionable area of mesothelial surface may be helpful but the accurate diagnosis can be made under the light of clinical presentations and elimination of the effusion after appropriate treatment [3].
Our primary histopathologic diagnosis for this exceptional case of symptomatic young patient was benign intranodal mesothelial cell inclusions secondary to SVC occlusion and the pleural effusion was considered as the consequence of thrombosis. Remarkably, although pericardial effusion is expected to occur as a result of direct invasion of the pericardium; in our case, it was more likely a consequence of SVC thrombosis. As patient's signs and symptoms did not resolve, after meticulous examination and mediastinal tissue sampling in second-look surgery malignant mesothelioma was diagnosed incidentally in the mediastinal sample in its unusual location, since no identifiable mass was present neither at direct vision nor in imaging studies.
We report a special and challenging case of a young patient with SVC thrombosis, massive effusions, and multiple extra-thoracic lymphadenopathies. These features along with the patient's age and absence of chronic asbestos exposure offered a diagnostic dilemma to the pathologist and clinicians. It is vitally important for the practitioner to quickly and accurately establish the diagnosis of malignant mesothelioma through multidisciplinary approach over other differential diagnoses like adenocarcinoma. In the final diagnosis of such complicated cases, in addition to considering the progression of the patient's clinical manifestations and the extent of elimination of the effusion after appropriate treatment; Immunohistochemistry, a cytologic evaluation and sampling of the suspected mesothelial surface can be very effective in excluding other differential diagnoses and should be considered. Seeking guide from a mesothelioma review panel, in such difficult cases is of great help yet not available in our region.
No funding was provided for this report.
All authors declare no conflicts of interest.
All of the authors contributed to planning, conduct and reporting of the work and approved the final manuscript. All contributors are responsible for the overall content as guarantors.