Branchial cleft anomaly, Congenital neck mass, Endoscope assisted surgery
Branchial cleft cysts are frequent causes of congenital neck masses-second only to thyroglossal duct cysts. Often asymptomatic, these masses can be missed until adulthood. The branchial apparatus is comprised of 3 parts: Arch, cleft, and pouch; these parts develop into the soft tissue, cartilaginous, and bony structures the mandible and neck. Incomplete obliteration is thought to result in branchial anomalies.
First branchial cleft anomalies (FBCA) are quite rare, comprising less than 8% of all brachial cleft malformations [1] and can be divided into two types by their embryological origin. Type I are ectodermal only and are a malformation of the EAC ending in a blind pouch toward the mesotympanum. Type II are composed of both ectoderm and mesoderm. They duplicate both the EAC and auricular elements, and thereby contain cartilage [1]. A complete type II tract frequently pierces the parotid gland, often tracking medial to the facial nerve on its way to the bony-cartilaginous junction or middle ear [2].
Here we describe a type II FBCA presenting as a parotid cyst, and compare it with the current literature describing the presentation, diagnosis, and treatment of other FBCAs.
A 14-year-old girl with a history of migraine headaches, presents with progressively enlarging left parotid mass, present for at least 10 years. The patient reported associated swelling and erythema with concurrent viral infections. Denies facial numbness, weakness, pain, or hearing changes. While being evaluated for headaches, an MRI of the brain revealed a 3.7 × 3.1 × 3.0 cm T1 enhancing mass in left parotid gland (Figure 1 and Figure 2). On further work-up, a CT neck with contrast demonstrated a well circumscribed homogenous mass within the superficial lobe of the left parotid, which was read as likely a lipoma. Physical exam did not reveal any skin pits or depressions, no abnormalities of the EAC or of the tympanic membrane was seen on otoscopy. As the mass was slowly increasing in size, cosmetically concerning to the patient, and causing discomfort, the decision was made to proceed with surgery.
 Figure 1: T1 Fat suppressed sagittal MRI showing close association of the mass with the EAC (arrow). View Figure 1
Figure 1: T1 Fat suppressed sagittal MRI showing close association of the mass with the EAC (arrow). View Figure 1
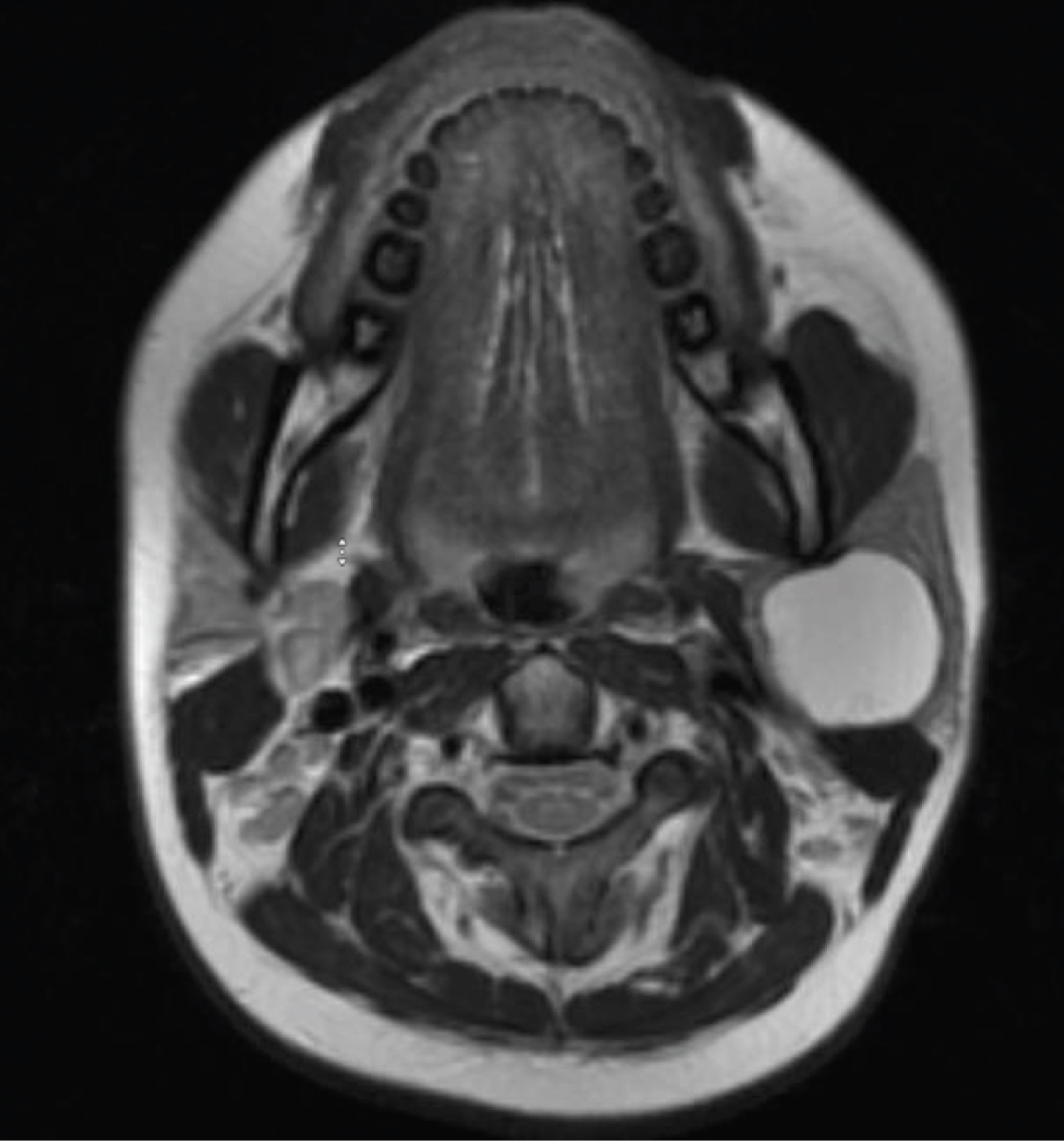 Figure 2: T1 axial MRI of parotid mass. View Figure 2
Figure 2: T1 axial MRI of parotid mass. View Figure 2
Under general anesthesia, a Blair incision was made to access the parotid mass, the root of the facial nerve was located. A well circumscribed cystic mass was identified at the tail of the parotid and extended medially and deep to the inferior division of the facial nerve (Figure 3). At the superior most extent of the mass, just deep to the main trunk of the facial nerve, the mass was connected to a cartilaginous stalk that appeared to be a duplicate EAC. The cyst itself was freed from the surrounding soft tissue, and as dissection was carried superiorly along the cartilaginous stalk it was found to be intertwined with the facial nerve. Once the proximal cartilaginous tract was dissected away from the nerve and excised, a STORZ rigid endoscope was used to examine the tract and a second, cartilaginous lumen was discovered which ended in a blind pouch proximally, with the facial nerve coming across it (Figure 4). Once the cyst and cartilaginous stalk were removed, the endoscope was re-introduced to confirm there was no communication or involvement of the EAC, and it was determined that the second lumen was too close to the facial nerve to safely resect. Prior to closure of the wound, the facial nerve was stimulated and was functional. Surgical pathology and cytology confirmed a type II first branchial cleft cyst. Post-operatively the incision was healing well, the facial nerve was intact, and the patient was pleased with the cosmetic appearance.
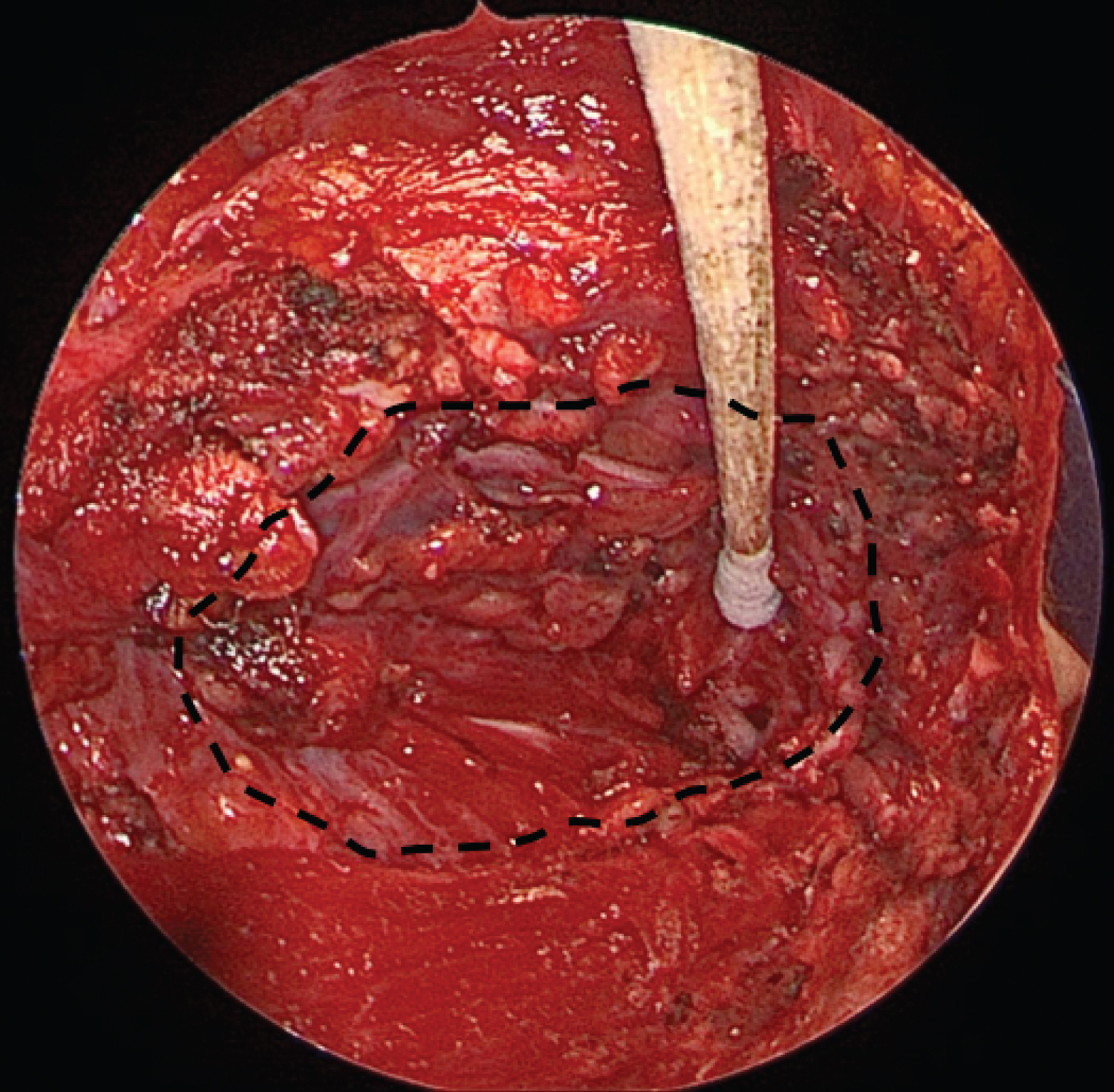 Figure 3: Extent of excised mass from the tail of the parotid. View Figure 3
Figure 3: Extent of excised mass from the tail of the parotid. View Figure 3
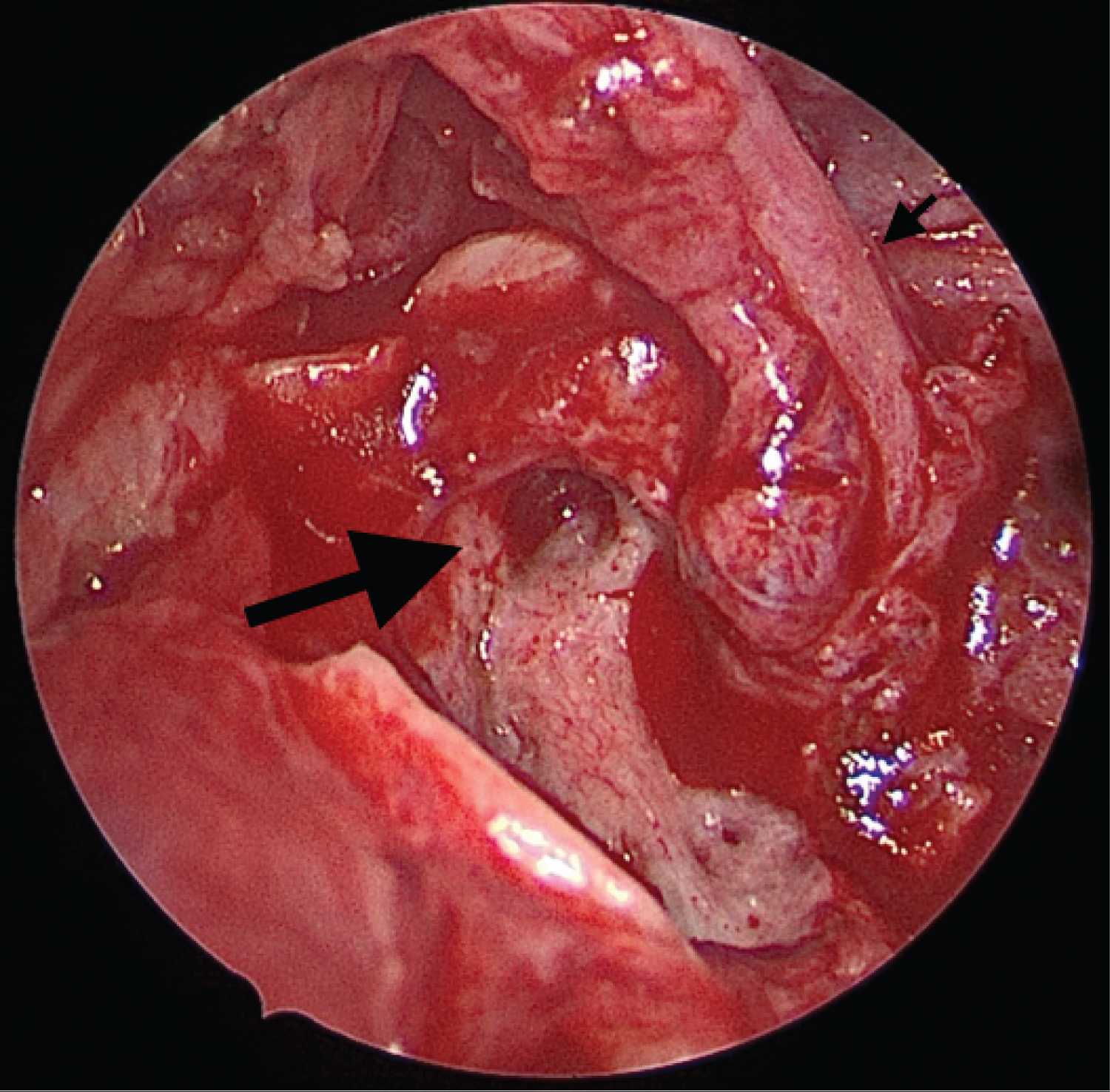 Figure 4: Cartilaginous portion of the branchial cleft cyst with close association of facial nerve. Small arrow: Root of the facial nerve; Large arrow: Cartilaginous portion of the branchial cleft cyst running deep to the facial nerve. View Figure 4
Figure 4: Cartilaginous portion of the branchial cleft cyst with close association of facial nerve. Small arrow: Root of the facial nerve; Large arrow: Cartilaginous portion of the branchial cleft cyst running deep to the facial nerve. View Figure 4
Abnormal fusion of branchial arches can result in various cysts, sinuses or fistula tracts. 66% of FBCAs present as cysts, typically within the parotid, and often with pits or depressions near the external auditory meatus. Many are asymptomatic, but patients can have a history of recurrent infections (up to 71% in one study), and some have presented with cholesteatoma secondary to an opening within the auditory canal [3]. Diagnosis can be challenging, requiring a thorough physical examination and CT and/or MRI imagining. Misdiagnosis often leads to incomplete measures such as incision and drainage of the mass. Radiographic dyes can also be introduced into the EAC or fistula tract and imaged to help delineate its path prior to surgery.
Definitive treatment of FBCAs is complete surgical resection including any involved skin or portion of the EAC and cartilage, typically involving a superficial parotidectomy for type II lesions. Recurrences are common, especially with incomplete resections. FBCAs are difficult to surgically resect due to their close association with the facial nerve. Complications can include facial nerve palsy/injury, parotid seroma, EAC stenosis [4]. Due to the close association of the facial nerve with type II lesions, it is recommended to have an operative microscope or telescope to avoid injury to the nerve, as well as contrast-enhanced preoperative imaging and intraoperative facial nerve monitoring. In fact, some surgeons in still a water-soluble dye such as methylene blue intraoperatively to help define the anomalous tract [4].
The presented case was unique in being diagnosed as a defined, encapsulated cyst within the parotid due to clinical findings and appearance on imaging, yet it was intraoperatively found to have a separate, uncommunicating sinus tract towards the EAC and middle ear. As there was no communication with the cyst, it was not enhanced with contrast on pre-operative imaging. This deeper portion may not have been discovered without the use of an endoscope and has not been previously described.
On average, it takes 2.4 procedures per patient to achieve complete resection, with each subsequent surgery increasing the risk of facial nerve injury due to scarring [5]. Although complete resection could not be safely achieved, she is asymptomatic and has had no episodes of recurrent infection or swelling with a 16 month follow-up.
First branchial cleft cysts are challenging entities to diagnose and treat. This patient presented with a unique variant of a type II anomaly with duplicate EAC attached to the facial nerve leading to a second, uncommunicating cartilaginous lumen. The use of a rigid endoscope was instrumental in this discovery as well as in preventing facial nerve injury.
No financial disclosures.
No conflicts of interest.