Oro-antral fistulas (OAF) produce infections in the maxillary sinus due to contamination with bacteria from the oral cavity, saliva and or food debris.
They are most frequently caused by extraction of upper molars or premolars or due to failure in the osseointegration of dental implants.
The treatment consists of the repair of the oral sinus communication and drainage of the sinus infection.
To determine the success rate of the repair of oral-sinus communications greater than 5 mm with the Bichat ball (BB) and vestibular mucoperiosteal flaps.
Data from patients who were treated for oroantral fistulas with Bichat ball (BB) and vestibular mucoperiosteal flaps between March 2019 and August 2022 were prospectively collected and analyzed.
Fifteen patients were treated, eleven women and four men.
The success rate of closure of the OAF with the Bichat ball and vestibular flaps was 93.33% (14/15).
The incidence of flap necrosis was 13.33% (2/15).
The success rate of closure of OAF that we had with the Bichat ball and vestibular flaps was 93.33% (14/15).
The use of the BB and vestibular mucoperiosteum flaps allowed to close the OAF in two planes. Due to its low morbidity, simple dissection, and high effectiveness, we believe that it is the surgical technique of choice to repair OAF.
Oroantral fistulas, Bichat ball flap, Buccal mucosa, Reconstruction
Oroantral fistulas are pathological communications between the oral cavity and the maxillary sinus.
The extraction of a tooth is frequently the cause of oroantral communication, due to the proximity of the dental roots to the floor of the maxillary sinus, which may also be thinned due to a dental infection.
A fibrous tract lined with epithelium is produced that can be blocked by granulation tissue, but which allows the passage of fluid, food, or bacteria from the oral cavity to the maxillary sinus, perpetuating the infection.
Treatment requires drainage of the sinus infection and repair of the oral-sinus communication with a local flap.
To determine the success rate of the repair of oral-sinus communications greater than 5 mm with the Bichat ball (BB) and vestibular mucoperiosteal flaps.
Prospective and descriptive.
The following data were prospectively collected and recorded as of March 2019 in patients who would be treated for OAF with BB and vestibular mucoperiosteal flaps: Sex, age, etiology of the fistula, location and laterality of the oral-sinus communication, history of previous closures, success, and complications of the repair of the fistulas.
The study was carried out in the Rhinosinusology section of the Otorhinolaryngology Department of the Italian Hospital of Buenos Aires, and end in August 2022.
All patients were evaluated by ENT examination, nasal endoscopy, and computed tomography (CT) of paranasal sinuses without contrast. All the fistulas were larger than 5 mm (the diameter was measured after performing the curettage of the granulation tissue that occluded the fistulous tract).
Patients were treated 45 days after tooth extraction or implant failure.
OAF repairs were made under general anesthesia on an outpatient basis or with 24 hours of hospitalization according to the anesthetic surgical risk that the patient had.
By an endonasal approach with a 0-degree endoscope an uncinectomy and median maxillary antrostomy and in some cases an anterior ethmoidectomy were performed.
Later in the same surgical time the mucofibrous edges of the fistula were resected and the tract was curetted. A trapezoidal mucoperiosteal flap was then dissected from the upper gingiva (vestibular) with buccal extension and upper base, and the buccinator muscle and its fascia were dissected with a Halsted-type forceps to locate the Bichat ball fat.
The Bichat ball was dissected by pulling on it without injuring its capsule or the vascular plexus, preserving a wide implantation base, until it covered the buccal orifice of the fistula, after it was sutured with two points of absorbable material (3/0 vycril) to the mucosal edge of the fistula.
The vestibular mucoperiosteum flap was then advanced and sutured to the edges of the communication with three sutures of resorbable material (Figure 1).
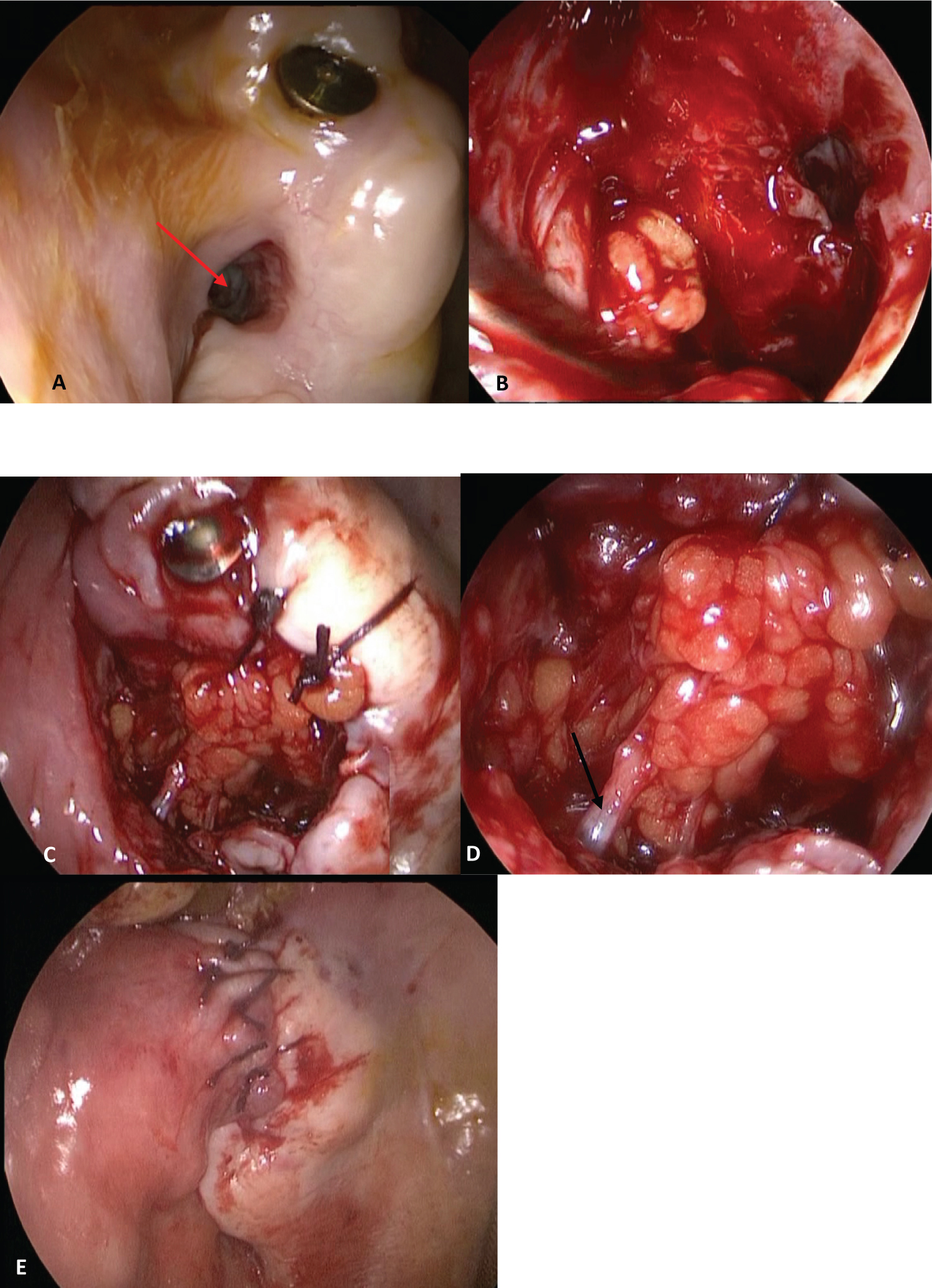 Figure 1: Oro-antral fistula repair with bichat ball and vestibular mucoperiosteum flaps: A) oral sinus communication; B) Bichat ball flap dissection; C) BB flap suture closing the fistula; D) Artery supplying the BB flap (arrow); E) Closure in two planes with vestibular mucoperiosteum flap.
View Figure 1
Figure 1: Oro-antral fistula repair with bichat ball and vestibular mucoperiosteum flaps: A) oral sinus communication; B) Bichat ball flap dissection; C) BB flap suture closing the fistula; D) Artery supplying the BB flap (arrow); E) Closure in two planes with vestibular mucoperiosteum flap.
View Figure 1
In the postoperative period, chlorhexidine digluconate mouthwash after meals, antibiotics for 10 days (875 mg amoxicillin + 125 mg clavulanic acid), and a soft diet were indicated. The patient was instructed to try to eat preferably on the side opposite of the reconstruction.
Indications were given to avoid maneuvers that increased intranasal pressure (sneezing or coughing) and to avoid negative pressure caused by sucking (drinking mate).
Controls were performed every 7 days, and the repair was considered successful when complete closure of the oral-sinus communication was observed (epithelization in 4-5 weeks) and the symptoms disappeared.
Fifteen patients were treated, eleven women and four men, for suffering from oral-sinus communications. The mean age was 62.33 years (43-81).
All had chronic maxillary or maxillary and ethmoid sinusitis diagnosed by CT.
The location of the OAF was at the level of the second premolar (1/15), first molar (3/15), second molar (6/15), and third molar (5/15). Eleven were lefts and four were rights.
In nine patients the fistulas were due to extraction of dental pieces and in six due to dental implant failures. One patient had a history of failed attempts to close the oroantral communication with vestibular and palatal mucoperiosteal flaps.
One patient had necrosis of the Bichat ball and the vestibular flap, possibly due to infection. The necrotic tissue was excised and after 3 months the fistula closed spontaneously.
Another patient with a history of concurrent chemoradiotherapy for maxillary sinus cancer had a satisfactory fistula closure (7-day follow-up), but she used a prosthesis early, which caused flap loss and persistence of the fistula.
One patient had a dehiscence of the vestibular flap, but closure of the communication was obtained only with the Bichat ball flap (Table 1).
Table 1: Patients treated for oro-antral fistulas with a bichat ball and vestibular mucoperiosteum flap. View Table 1
The success rate of closure of the OAF with the Bichat ball and vestibular flaps was 93.33% (14/15).
The incidence of flap necrosis was 13.33% (2/15).
Oro-antral communications can originate from the extraction of an upper molar or premolar, due to the anatomical relationship of the dental roots with the floor of the maxillary sinus (iatrogenic causes: 47.56%).
Other causes may be the extrusion of endodontic filling material (22.27%), foreign bodies (19.72%), residual amalgams after apicoectomies (5.33%), maxillary sinus floor elevation procedures (4.17%) and failure in the osseointegration of dental implants (4.17%) [1].
They can also be caused by the resection of cysts, benign or malignant tumors of the upper jaw, trauma, or infections [2].
In our study there was a predominance of oral-sinus communications produced by dental extractions (9/15) and six fistulas were produced by lack of osseointegration of dental implants.
Defects with diameters smaller than 5 mm and without epithelialization of the fistulous tract can close spontaneously, when they are longer, they require a surgical repair [1].
It is necessary to drain the sinus infection before the repair of the fistula, at the same surgical time through a median maxillary antrostomy or to extend the drainage to the ethmoid by endonasal approach with endoscopes, according to the previous CT.
In all the patients described in our study, endonasal drainage was performed with endoscopes at the same surgical time, prior to fistula repair to treat chronic sinusitis.
The use of external approaches such as anterior sinusotomy should not be indicated since they do not act permeabilizing the maxillary natural ostium and can cause more complications and morbidity in patients, except in exceptional cases such as to remove foreign bodies or resect cysts or maxillary tumors coexisting with the fistula.
It is necessary to remove the granulation tissue and the fistulous tract of the communication prior to reconstruction [3].
Different types of flaps with or without grafts can be used to repair communication. Local flaps such as the vestibular mucoperiosteal advancement flap, the palatal flap with a pedicle in the greater palatine artery, the buccinator myomucosal flap with a posterior pedicle, or distal flaps such as the tongue flap can be used in the repair with different advantages and disadvantages [4].
The Bichat ball fat flap was described in 1977 by Egyedi [5] and has the advantages of its proximity to the closure site, wide arc of rotation, and contraction resistance, making it possible to repair defects up to 5 × 4 cm [6].
The fat of the flap is located between the buccinator and the masseter muscles, surrounded by a thin fascia. It has a central body and four extensions (buccal, pterygoid, pterygomandibular and temporal), the central part and the buccal extension are used for reconstruction. The blood supply is from branches of the internal maxillary, superficial temporal, and facial arteries.
The failure rate of the communication repair with the Bichat ball flap is low [7,8] and is caused by flap necrosis. A mild depression in the cheek after the reconstruction has also been described as a sequel.
No patient in our series had an aesthetic change in the cheek due to the use of the BB flap.
Some authors have reported the use of the BB flap to fistulas repair without covering it with the vestibular advancement mucoperiosteal flap; according to them the epithelization occurs in two weeks [7-9].
Candamourty, et al. [10] compared the closure of OAF using the BB pedicled flap alone with the use of the combined BB and vestibular mucoperiosteum flap.
They concluded that there was no benefit in covering the BB flap with the buccal flap, and that this might be necessary if the fat traction was excessive, or the fat was perforated during dissection.
In a meta-analysis [11], they compared the complications that occurred with the use of different flaps used for the closure of oroantral communications.
The palatal rotary flap had 55.84% complications, the BB flap 16.88%, and the vestibular mucoperiosteal flap 15.58%.
The fistulas treated with primary closure had 10.39% of complications.
With all the techniques used, the most frequent complication was refistulization except with the palate flap, where partial necrosis of the flap predominated.
With the BB flap, they reported 1.30% failure, 3.9% herniation of fat, 9.09% formation of granulation tissue, and 2.59% partial necrosis (Table 2).
Table 2: Meta-analysis: Type and number of complications according to the reconstructive technique [11] (PUB-MED and Compludoc articles between 1983-2008: 15 articles = 1072 cases). View Table 2
In two studies they reported that they treated 25 and 19 patients respectively for oroantral fistulas with the BB flap and had 100% success in closing the communication [2,12].
In our series we had a total necrosis of the BB flap and of the vestibular mucoperiosteal flap due to infection, but endonasal drainage of the maxillary sinusitis possibly contributed to the resolution of the chronic infection and spontaneous closure of the communication at three months.
Another patient had a dehiscence of the vestibular flap without involvement of the BB flap, which adequately repaired and closed the fistula.
A patient who had a history of treatment with chemoradiotherapy for squamous cell carcinoma of the maxillary sinus had a post-extraction fistula at the level of the upper second molar.
In the control 7 days after the repair, was observed that the flap was vital and there were no dehiscences. Five days later she consulted and said that after using the prosthesis had a dehiscence and necrosis of the flap.
We attribute this case of failure to non-compliance with the preventive indications by the patient and not due to infection or a defect in the technique.
The combined repair with the two flaps allows closure in two planes and provides greater security in achieving the closure of the communication.
The disadvantage of using the vestibular flap is that it occludes the vestibular gingival sulcus [13,14] and this can make the use of a prosthesis challenging in the future.
Von Wowern, et al. demonstrated in a study that the reduction of the vestibular sulcus was permanent in 50% of the patients treated with a vestibular advancement flap [15].
The alternative in these cases is the placement of an implant to retain the prosthesis.
The success rate of closure of OAF that we had with the Bichat ball and vestibular flaps was 93.33% (14/15).
The use of the BB and vestibular mucoperiosteum flaps allowed to close OAF in two planes. Due to its low morbidity, simple dissection, and high effectiveness, we believe that it is the surgical technique of choice to repair OAF.
It is very important to perform an endonasal drain of the sinus infection at the same surgical time of the OAF repair.
We do not declare conflicts of interest.