Antibiotherapy has shown a clinically significant decrease in PSA levels in some patients. However, the clinical benefit of this decrease, which would increase the diagnostic efficacy of PSA, has not yet been established. To our knowledge, PSA half-life and PSA-ENT2.5 (expected normalization time according to 2.5 ng/mL cut-off value) were unexamined parameters. The aim of this study is to investigate the efficacy of PSA-ENT2.5 and PSA half-life after antibiotherapy for predicting prostate cancer diagnosis.
64 patients with a PSA value in gray scale (2.5-10 ng/mL) were included in this prospective study. Two weeks of oral levofloxacin treatment was given to all of the patients. Twelve core prostate biopsies were performed after antibiotherapy in all cases. Patients were divided into two groups as biopsy-proven cancer patients and non-cancer biopsy groups, and were compared according to PSA-ENT2.5 and PSA half-life.
The mean PSA half-life (624.6 ± 1062 days) was higher in the group with prostate cancer than in the group without prostate cancer (390.2 ± 476) (p = 0.49). PSA-ENT2.5 was higher in prostate cancer detected group (p = 0.16). There was no statistically significant difference between the two groups for other dynamic parameters (PSA reduction rate and value change). However, the most statistical powerfull parameter was PSA-ENT2.5 in all dynamic PSA parameters.
Antibiotherapy provides a clinically significant reduction in patients with PSA level gray scale (2.5-10 ng/mL). PSA half life and PSA-ENT2.5 are promising new parameters that can be used for this purpose. A larger scale prospective study is needed in this area.
PSA, Antibiotherapy, Prostate cancer
It is a method that clinicians frequently refer to evaluate the effect of antibiotherapy on PSA before giving a biopsy decision in high PSA values. Some studies have shown that PSA may be reduced by antibiotherapy and that the biopsy requirement may be absent. The pilot study was published in 2002 [1]. Bulbul and his colleagues gave ciprofloxacin treatment for 2 weeks to 48 patients due to high PSA (5-28.5 ng/mL). All of the patients had normal rectal examination findings. 52% PSA reduction was reported after antibiotherapy.
Although antibiotics are not recommended except for symptomatic patients with high PSA levels, they are currently used. This may be explained by the fact that a single PSA value is still insufficient in biopsy decision making by clinicians. It is clear that antibiotherapy provides PSA reduction in some patients. On the other hand, the clinical benefit of this decline has not yet become clear. A randomized clinical trial conducted in 2016 showed a limited PSA reduction advantage in the antibiotherapy group but no difference in positive prostate biopsy results [2]. There are even studies showing that cancer is detected at a higher rate in patients has PSA decline with antibiotherapy [3,4].
To our knowledge, PSA half-life and PSA-ENT2.5 (expected normalization time according to 2.5 ng/mL cut-off value) were unexamined parameters. The aim of this study is to investigate the efficacy of PSA-ENT2.5 and PSA half-life after antibiotherapy for predicting prostate cancer diagnosis.
The data of 64 patients were obtained from a surveillance study on the use of antibiotherapy in high PSA values in Cerrahpaşa Medical Faculty [5]. 7200 men aged over 40 were admitted to the urology outpatient clinic in 2017. Of these, 3096 (43%) men who were not diagnosed with prostate cancer subjected to PSA screening (Figure 1). 136 patients with PSA values in the gray zone (2.5-10 ng/dL) were treated with antibiotics and 96 patients were followed-up. All patients digital rectal examinations were normal. PSA reduction was observed in 89 patients with antibiotherapy.
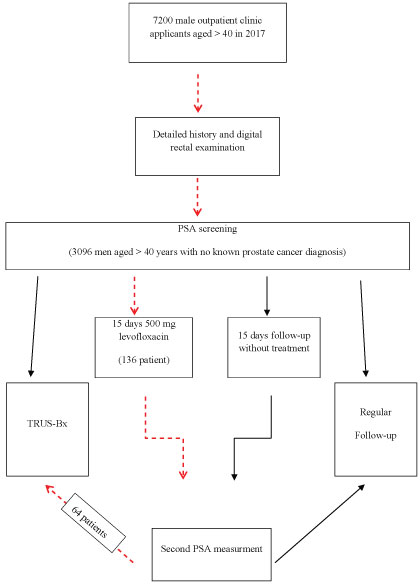 Figure 1: The flow diagram of the surveillance study.
View Figure 1
Figure 1: The flow diagram of the surveillance study.
View Figure 1
64 patients has a PSA decrease after antibiotherapy and biopsied were included in the this study. All patients treated with levofloxacin 500 mg orally for 14 days. The duration of antibiotherapy was based on a prospective controlled trial in which the PSA decline curve reached plateau on the 7th day [6].
Patients with a PSA less than 2.5 ng/dL and greater than 10 ng/dL, positive digital rectal examination sign, known prostate cancer and levofloxacin allergy were excluded from study. PSA was measured twice with a three-day interval and the lower value was taken into account.
PSA half life calculated according to the following formula [7,8]:
In the formula, dt refers to the time elapsed between two PSA measurements. PSA0 indicates initial (pre-antibiotherapy) PSA value and PSAt indicates the value after antibiotherapy.
In addition, the predicted time for PSA to be reduced to 2.5 ng/mL was calculated by substituting 2.5 cut-off values for the PSAt. This is defined as the Expected Normalization Time (ENT2.5). The formula is as follows;
Systemic 12-core prostate biopsy was performed with transrectal US in all patients. Patients were divided into two groups as biopsy-proven cancer patients and non-cancer survivors. PSA half-life and PSA-ENT2.5 and other static and dynamic PSA parameters (PSA, PSA-D, PSA value change and rate) were compared.
Statistically significant difference was investigated using Student's T-test between the two groups. The data was analyzed with the Statistical Package for the Social Sciences v. 16 (SPSS Inc, Illinois, USA). A p-value under 0.05 was considered statistically significant.
PSA parameters after antibiotherapy according to pathologic results are shown in Table 1. Patients has PSA reduction with antibiotherapy and biopsied were divided into two groups as prostate cancer and benign pathologic findings (BPH, prostatitis). Although the first PSA value (5.81 ± 1.37) was lower in the cancer detected group than the other group (6.43 ± 1.82), the difference was not statistically significant (p = 0.68). There was no statistically significant difference between the two groups in terms of pretreatment PSA-D, posttreatment PSA and PSA-D parameters (p = 0.87, p = 0.86 and p = 0.77, respectively).
Table 1: PSA parameters after antibiotherapy according to pathologic results. View Table 1
There was no statistically significant difference between the two groups in terms of PSA means of value change, PSA and PSA-D value change (p = 0.30, p = 0.39 and p = 0.50, respectively).
The mean PSA half-life (624.6 ± 1062 days) was higher in the group with prostate cancer than in the group without prostate cancer (390.2 ± 476). However, inadequate patient numbers of the groups resulted in statistical unsignificance (p = 0.49). A similar statistical insufficiency existed for the PSA-ENT2.5 parameter. PSA-ENT2.5 was higher in prostate cancer detected group (p = 0.16). However, the statistically strongest parameter in all dynamic PSA parameters was PSA-ENT2.5.
It is clear that the strong clinical effect of antibiotherapy on PSA can not turn the clinical benefit that will increase the diagnostic power of the test. Although many studies have shown statistically significant reductions in PSA with antibiotherapy in cohorts with high serum PSA, the clinical benefit of statistical significance has not been fully elucidated. To this end, a dynamic parameter is needed to increase the effectiveness of PSA in prostate cancer screening. First of all, the conditions for evaluating the statistical significance of PSA reduction as clinically significant PSA reduction should be established.
Differences between histopathological diagnostic groups were investigated by considering the value change or percentage of PSA decrease in some studies. In a study investigating the efficacy of antibiotherapy in patients with a range of 4-10 ng/mL PSA, a 23.3% reduction was reported [9]. Another study in our country aimed to show the effects of antibiotherapy and antiinflammatory treatment separately on the data of 216 patients with similar PSA range (2.5-10 ng/mL) in our study group [10]. A statistically significant decrease in PSA was reported with antibiotherapy (mean: 5.2 ng/mL to 4 ng/mL) in the group with prospective randomized design with only inflammatory findings of the prostate secretory. The highest percentage of PSA decline was observed in the antibiotherapy group, followed by patients receiving anti-inflammatory treatment and the control group (18.5%, 10.2%, and 2.1%, respectively). When the study was considered in terms of pathological results, it was seen that the results were not statistically significant. In our study, a similar PSA reduction rate was obtained with antibiotherapy (21%).
In a study investigating the efficacy of PSA-level reduction in distinguishing pathologic diagnostic groups, PSA reductions in prostate cancer cases have been shown to be statistically insignificant [11]. PSA in patients with cancer decreased by 8.5% on average, while rates of inflammation and BPH were 12.3% and 16.4%, respectively. Although the study has a controlled design, combined therapy has made it difficult to determine which agent the responsible of the PSA is due to. On the other hand, as is done in the study, it is not a randomization method to choosing one of the three patients. As a result of this situation, there are significant differences between treatment and control groups in terms of many factors. Patients in the treatment group had younger and more normal rectal feelings in a statistically significant manner. As a result, the baseline PSA level in the control group was significantly higher (25.2 and 13 ng/mL). In our study, a decrease in PSA of 7% was found in the group receiving prostate cancer, compared with 11% in cancer-negative patients. Although the rate of decrease was low in cancer cases, the difference was not statistically significant (p = 0.3).
In a systematic review of studies involving patients with Type 4 chronic prostatitis, antibiotherapy was associated with a total PSA reduction of 33.2% [12]. The meta-analysis of two randomized clinical trials showed that this rate of decline was statistically insignificant compared to the control group. Although the amount of decrease in PSA as a candidate parameter for investigating the efficacy of antibiotherapy has been extensively investigated, prostate cancer cases seem to be inadequate to separate from other benign cases. In fact, with this method it is possible to obtain a PSA reduction rate predictor value that predicts prostate cancer diagnosis with certain sensitivity and specificity rates. However, the number of cases to achieve cut-off value in any study has not been reached.
In the study of Karazanashvili, et al., PSA-VCh (PSA value change) after antibiotherapy was considered as a diagnostic method and its efficacy in prostate cancer screening was investigated [13]. PSA-VCh has been reported to exhibit 85% sensitivity, 96% specificity, 85% positive predictive value, and 96% negative predictive value for prostate cancer. For an ideal diagnostic test, all of the above values should be more than 80% of all values. According to the findings of the study, PSA-VCh is an ideal diagnostic test that increases the value of PSA in prostate cancer screening.
On the other hand, some authors categorized PSA reductions by taking the existing PSA cut-off values (2.5 or 4.5 ng/mL) used for prostate cancer diagnosis as a reference. Ugurlu and colleagues found that the PSA levels fell under the 2.5 ng/mL cut-off value in 22.2% of patients [10]. In our study, 19 of the 89 patients were below the PSA 2.5 ng/mL cut-off value, which is similar to the above-mentioned study (21%). In another study, 37.5% of patients had PSA below the 4 ng/mL cut-off value [9]. Even with very low serum PSA levels prostate cancer is known to be present. Although some predictive values are used, PSA is a continuous parameter that increases the predictability of prostate cancer diagnosis as it rises. As expected, PSA, which falls below the cut-off value in any study, is far from predictive of prostate cancer diagnosis.
As shown, clinical course in antibiotherapy-treated patients have been given a lots of PSA parametres. The categorization of post-treatment value was frequently investigated according to pre-treatment PSA, post-treatment PSA and time between two values, the difference or percent change between two PSA values and the commonly accepted cut-off values (2.5 and 4 ng/mL) in some trials. However, these parameters alone are insufficient to compare with pathological results. Possibly all of the parameters are valuable and more meaningful results can be obtained when taken together.
PSA half life is a common function of many of the above parameters. The time between the first PSA and the post-treatment PSA values and the two PSA values is included the formula. However, the rate of change between the two values comes into play as the initial PSA and post-treatment PSA values do not directly affect the outcome. That is, the PSA half-life of the patient who regressed from 10 ng/mL to 5 ng/mL in 10 days and the patient who decreased from 4 ng/mL to 2 ng/mL is the same (PSA: 10 days). However, the PSA value of the first patient was still gray, while the PSA of the second patient was normalized to 2.5 cut-off values. There is also a significant difference between the initial PSA value of the first patient and the latter in terms of the risk of clinically significant prostate cancer detection.
Another candidate parameter that represents all these differences is the expected normalization time of the PSA according to the cutoff value of 2.5. The formula contains almost all of the available parameters used to investigate the efficacy of antibiotherapy. According to the formula, there is a 3-fold difference between the expected normalization durations of patients in the sample (20 and 6, 78, respectively).
In our study, we tried to obtain a function and parameter which includes all factors that may affect the biopsy decision over the new PSA value obtained after antibiotherapy. We believe that this study will contribute to science because it includes a new approach. However, the insufficient number of patients made it difficult to obtain statistically significant results. Therefore, the sensitivity and specificity value of the new parameters (PSA half-life and PSA-ENT2.5) for a certain cut-off value could not be studied.
Dynamic parameters (PSA reduction rate, value change, PSA half-life and PSA-ENT2.5) obtained after antibiotherapy did not make a statistically significant difference between the cancerous and cancer-free cases. Specificity and sensitivity studies for diagnostic cut-off value could not be done due to insufficient number of patients.