Yellow nail syndrome is a rare condition of unknown etiology, which is defined by the triad of yellow, slowly growing thickened nails, lymphedema, and respiratory manifestations. In order to strengthen the literature on this topic, we report the case of a 64-year-old man with yellow nail syndrome and recurrent pleural effusion. The patient was referred to the Emergency Department because of dry cough and gradually worsening dyspnea over the previous two months. A diagnosis of yellow nail syndrome was based on the presence of nail abnormalities, lymphedema and pleural effusion. He was administered symptomatically with thoracentesis of the left pleural space, initiation of intravenous diuretics and antibiotics and topical nail treatment. However, two years later the patient was readmitted to the hospital due to recurrent pleural effusion, confirming that managing the complications of the syndrome could be more challenging than setting the diagnosis.
Yellow nail syndrome, Pleural effusion, Nail abnormalities
Yellow nail syndrome is a rare condition of unknown etiology, which was first described in 1964 by Samman and White [1]. It is typically encountered among middle-aged people, with both sexes being equally affected. Current evidence suggests that it is characterized by the triad of yellow -slowly growing thickened- nails, lymphedema and respiratory manifestations, such as pleural effusion, bronchiectasis, bronchial hyperactivity, rhinosinusitis, chronic cough and recurrent lower respiratory tract infections [2]. The presence of two of the three aforementioned criteria is sufficient to set the diagnosis.
The pathophysiology of the syndrome remains obscure, with hypoplasia of the lymphatic system or an immunological deficiency being the most common underlying causes. An association with systemic malignancies and drugs (D-penicillamine, gold and bucillamin) has also been described [3,4]. There have been only a few published cases, where a positive family history was reported [5,6]. Treatment is symptomatic and mainly includes pharmaceutical and interventional methods unless an underlying disease is diagnosed. The prognosis of yellow nail syndrome is generally good and even spontaneous remission can occur [7].
The purpose of this article is to present a rare case of yellow nail syndrome in a 64-year-old male with recurrent pleural effusions and provide a comprehensive review of the literature regarding this unique entity.
A 64-year-old obese man presented to the Emergency Department with dry cough and gradually worsening dyspnea over the previous two-month period. He also reported anorexia, malaise, and myalgia. His medical history was unremarkable, except for arterial hypertension. He was a current smoker with a smoking history of 60 packyears. A year ago, he was admitted to hospital due to pleural effusion which was effectively treated with furosemide.
Physical examination was notable for hypoxemic respiratory failure along with sinus tachycardia and bilateral pitting lower leg oedema (Figure 1). Lung auscultation revealed decreased breath sounds at the left lung base and a subsequent chest X-ray confirmed the diagnosis of unilateral pleural effusion. The patient was also found to have a yellowish discoloration of his nails with onycholysis and increased transverse curvature (Figure 2). He was consequently admitted to the Pulmonary Department for further investigation.
 Figure 1: Lymphedema and nail abnormalities. View Figure 1
Figure 1: Lymphedema and nail abnormalities. View Figure 1
 Figure 2: Yellowish discoloration of nails with onycholysis and increased transverse curvature. View Figure 2
Figure 2: Yellowish discoloration of nails with onycholysis and increased transverse curvature. View Figure 2
Thoracentesis of the left pleural space was performed, revealing 2.500 ml of exudative pleural fluid with a lymphocytic predominance (cell count = 3.600 cells/μl, lactate dehydrogenase = 263 U/I, glucose = 123 mg/dl, protein = 5.87 g/dL and pH 7.41), value of ADA within normal limits and negative cytology and microbiology. Blood tests showed a leukocyte count within normal range, a slightly high serum albumin level while there was no sign of inflammatory or autoimmune disease. Flow cytometry ruled out chronic lymphoproliferative disorders. A chest CT was therefore performed, describing mild bilateral pleural effusions, bronchiectasis and bronchopneumonia with wall thickening of the central bronchi (Figure 3). In addition, a sinus CT showed soft tissue densities around maxillary and ethmoid sinuses on both sides (Figure 4).
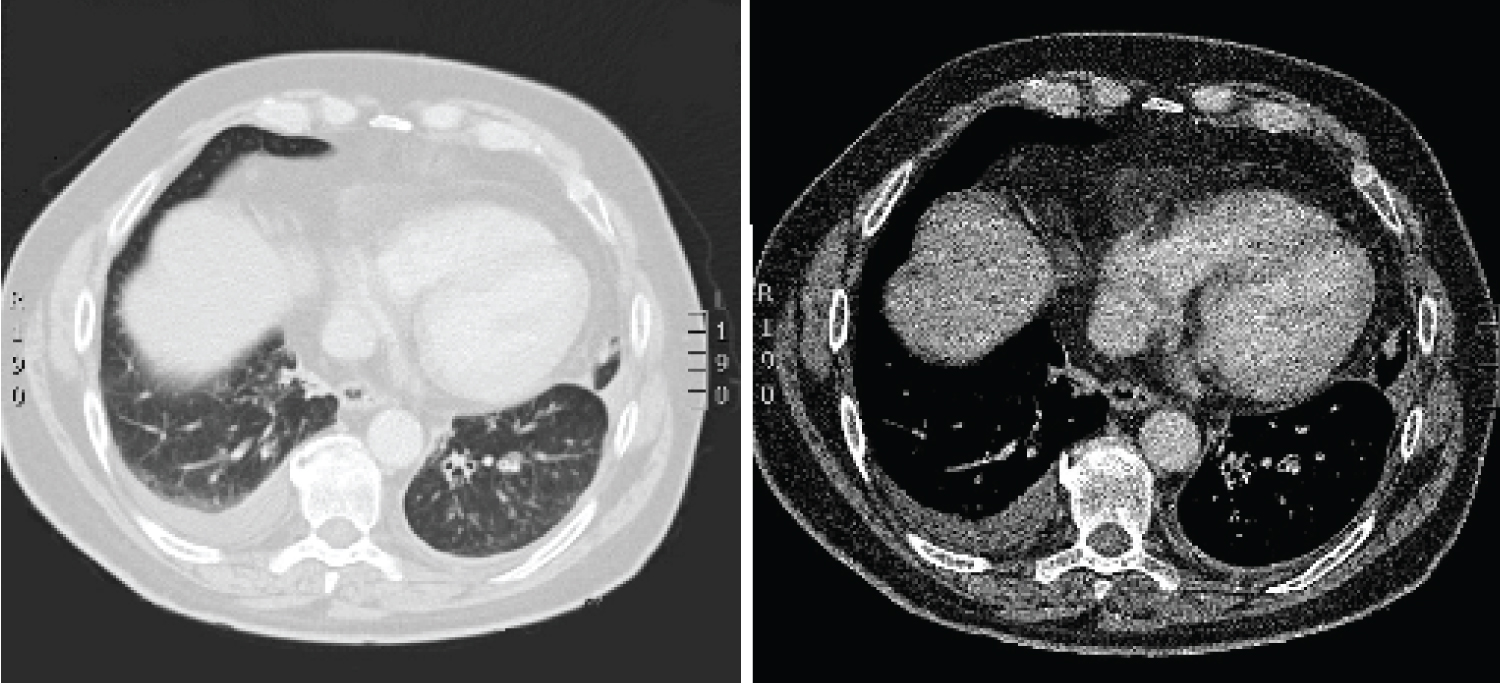 Figure 3: Chest CT with mild bilateral pleural effusions and bronchiectasis. View Figure 3
Figure 3: Chest CT with mild bilateral pleural effusions and bronchiectasis. View Figure 3
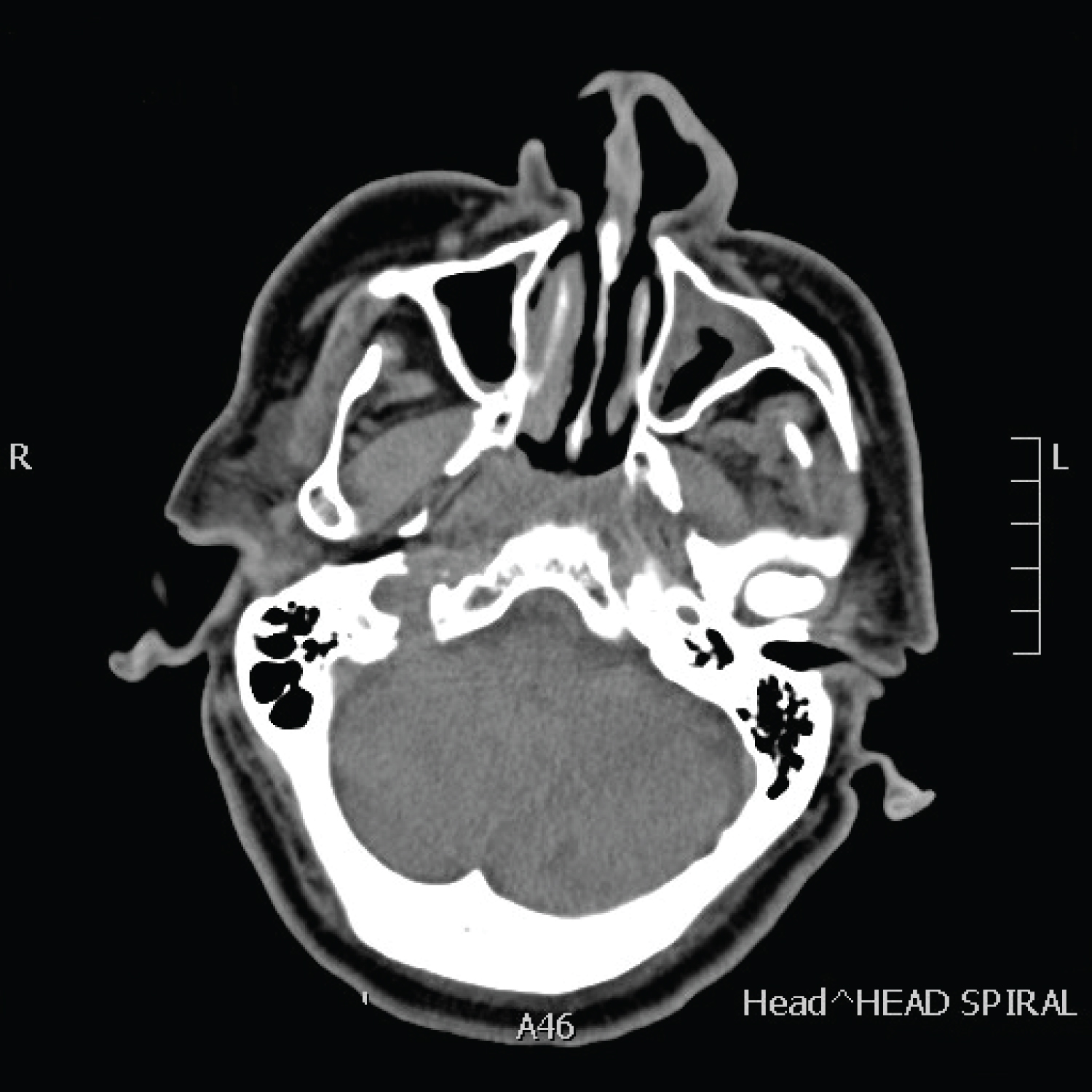 Figure 4: Sinus CT: Soft tissue densities around maxillary and ethmoid sinuses on both sides. View Figure 4
Figure 4: Sinus CT: Soft tissue densities around maxillary and ethmoid sinuses on both sides. View Figure 4
As a result, a diagnosis of yellow nail syndrome with chronic sinusitis was given. Nail cultures for bacteria and fungi were negative and lymphangiographic data confirmed impaired lymphatic drainage of the lower limbs.
Conservative management was attempted with continued catheter drainage and initiation of antibiotic treatment with ampicillin/sulbactam (3 gm every six hours intravenously) for ten days. Intravenous furosemide was also added, resulting in a significant improvement of the leg swelling. The yellow nails were treated with topical betamethasone valerate and gentamicin sulfate ointment according to the instructions of the experts of the Dermatology Department. However, no clear response was observed. Drainage gradually decreased over the next days and the patient was discharged from the hospital with instructions for continuation of oral diuretics at home.
At 4-week follow-up, chest X-ray detected no recurrence of pleural effusion. There was notable enhancement regarding dyspnea, cough, and hypoxemia. The lymphedema of the extremities was clinically stable.
Two years later, the patient was readmitted to hospital due to exertional dyspnea. On examination, sinus tachycardia, hypercapnic respiratory failure and excessive swelling of both lower limbs was noted. Chest X-ray findings proved the reproduction of the left-sided pleural effusion and intravenous diuretics were administered. A chest tube was also inserted, and pleural fluid was completely drained.
A pulmonary embolism was suspected based on persistent hypoxemia despite complete resolution of pleural effusion. Heart failure was also ruled out. Therefore, the patient underwent CTPA (Computed Tomographic Pulmonary Angiography) and the diagnosis of pulmonary embolism was confirmed. A subsequent triplex ultrasound of the left lower limb revealed the presence of thrombus in the left common femoral vein and low molecular weight heparin was prescribed. Five days later, significant clinical improvement was observed, as hypoxia and leg swelling decreased, and the patient was discharged from the hospital. At 2- and 4-week follow ups, chest X-ray showed trace pleural effusion with no recurrence of hypoxia, but patients' yellow nails and lymphedema remained unchanged. A follow-up F-18 FDG PET/CT was scheduled one month later, revealing no sign of malignancy. The patient remains on active follow up.
Yellow nail syndrome is a rare clinical entity that is often misdiagnosed. Since its' initial description, less than 400 cases have been described in the literature, including either single case reports or limited case series [2,8]. Although the yellow nail syndrome is defined by the characteristic triad of nail abnormalities, lymphedema and respiratory disorders, all three criteria are reported in less than one-third of the patients [9]. Unlike our patient who presented with all the above mentioned criteria at the time of diagnosis, not all of them are required at once [9,10].
The pathogenesis of yellow nail syndrome remains uncertain. Current literature suggests that the dysfunction of the lymphatics and microvasculopathy with protein leakage constitute the main causes, while nail discoloration is possibly attributed to lipofuscin pigments [2,9,11]. Even though yellow nail syndrome can rarely be congenital or occur in pediatric age, a fully detailed family history is required prior to examination [1,12]. The etiology of the syndrome is still undefined. However, an association with malignancies, endocrine and autoimmune disorders has been suggested [12].
The diagnosis of the syndrome is mainly based on the three clinical criteria and is established by supplementary laboratory and imaging tests. Chest and sinus computed tomography are eligible for the detection of lower respiratory track abnormalities and chronic sinusitis, while lymphoscintigraphy constitutes a useful tool in the diagnosis of lymphatic system dysfunctions [13]. Pleural effusion is frequently bilateral and typically exudative with a predominance of lymphocytes. The diagnosis of lymphoproliferative disorders could be eliminated using flow cytometry analysis. Nail cultures for bacteria and fungi are advised as a routine investigation before the prescription of antifungals, since they are usually negative [14].
Once the diagnosis of yellow nail syndrome is set, there are various symptomatic approaches but no consensus therapy has been established [2]. Pleural effusion is mainly treated by diuretics, while respiratory tract infections usually require the prescription of antibiotics and bronchodilators. Chest tube placement might be indicated in cases of large pleural effusions, chylothorax or empyema. Sputum cultures could provide further targeted therapy, especially in patients with a medical history of recurrent exacerbations of bronchiectasis [15]. As for the latter, pneumococcal and annual flu vaccinations are also recommended [15]. Studies show that endoscopic sinus surgery could enhance patients' respiratory symptoms [16].
High doses of vitamin E have been widely prescribed, resulting in remarkable improvement of the yellowish nails. There are still a significant number of patients who have reported a spontaneous reversal of nail manifestations without treatment [6]. Oral antifungals could favor outgrowth and clearance of the nail discoloration, when indicated [14]. Management of lymphedema includes bandage wraps, exercise, diuretics, manual drainage and external pneumatic compression [2,13]. In case of comorbidities, patients may benefit from the treatment of the underlying diseases [15].
Prognosis of patients with yellow nail syndrome is favorable [2,11]. A review of the literature concludes that no deaths have been directly associated with yellow nail syndrome, whereas overall survival remains shorter than the general population [14].
In this case, the hypothesis of yellow nail syndrome was based on clinical manifestations, since the patient fulfilled all three criteria on examination. Further investigation confirmed the presence of the syndrome, and the patient was symptomatically treated. Notably, management of the case was challenging, since the detection of pulmonary embolism on follow up aroused the suspicion of other underlying causes, such as malignancy.
Yellow nail syndrome remains a rare and intriguing disorder that should be considered in individuals with pleural effusion of unknown etiology, who arrive at the pulmonary department. This case alerts physicians to a thorough clinical examination of every patient since it could unravel an alternative pathway in early diagnosis of the syndrome.
No funding resources have been provided for this manuscript. The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
All authors contributed equally to this manuscript.
Konstantinos Porpodis, Filippou Ioanna, Tsiouprou Ioanna and Kontakiotis Theodore: Conceptualisation, investigation, resources, writing - original draft, review, editing.
This manuscript has not been submitted to, nor is under review at, another journal or other publishing venue.
A written consent was obtained by the patient.