The number of cases undergoing Total Knee Arthroplasty (TKA) has advanced manifolds in India and the role of Metal Artifacts Reduction Sequences (MARS) MRI is also gaining wide attention amongst Orthopaedicians/Radiologists for evaluation of painful knee after TKA or post TKA complications [1]. Here, we report a case of Patellar Clunk Syndrome (PCS) diagnosed on MRI with MARS sequence where the patient was also undertaken for Ultrasound for correlation. Here, the patient was also diagnosed with fracture of post of Polythylene liner of right and left knee.
Globally, Painful Patellar Crepitation or Patellar Clunk Syndrome (PCS) after TKA has been reported to be 0-20% [2]. Many studies have reported the occurrence as a result of Posterior stabilized knee prosthesis, although it may occur after cruciate-retraining TKA.PCS is a painful palpable “Clunk” that occur at the patellofemoral articulation of a posterior stabilized TKA. It is the overgrowth of a fibrous nodule at the attachment of extensor mechanism to superior aspect of Patella. This fibrous tissue engages the intercondylar box of femoral component and results in painful catching while knee is moving from a flexed to an extended position [3]. Generally, PCS develops after a year of TKA, while some studies have also reported PCS to be occurring after six years of TKA [4].
Diagnosis of painful knee after TKA can be challenging. Hence, imaging serves as the cornerstone for differential diagnosis of painful knee after TKA. Historically, MRI served limited role in soft tissue evaluation after TKA, given the artifacts from metallic hardware which produces significant in-plane and through-plan distortion of the encoded signal, which blocks visualization of soft tissue and osseous details [5]. Recently, over the past decade, development of novel pulse MRI sequence, MARS protocol has improved MR examination relevant to answer clinical questions of the osseous integration, aseptic loosening, polyethylene wear, component malrotation, extensor mechanisms, patellar clunk syndrome, and vascular complications etc [6]. Ultrasound may also be used for confirmation of patellar clunk syndrome by directly visualizing soft tissue proliferation deep to distal quadriceps tendon. Soft tissue proliferation can be dynamically demonstrated during both flexion and extension of knee on ultrasound [7].
Metal Artifact Reduction Sequence (MARS) is an advanced imaging technique in magnetic resonance imaging (MRI) designed to minimize the size and intensity of artifacts caused by metal implants [8]. MARS employs a combination of innovative acquisition strategies, including using multiple radiofrequency pulses and adjusting gradient strengths in order to mitigate the impact of metal-induced artifacts. MARS selectively acquires data around the metal thereby minimizing signal loss and distortion. This results in more accurate and clearer images of the tissues near the metal implant [9]. Hence, this technique improves the diagnostic value of MRI in patients with metal implants.
Finally, the most common causes of PCS are design of the implant, more than average flexion of the Knee, surgical trauma, components position, and alteration of the joint line, patellar height, and patellar button-patellar bone composite thickness. Once identification, treatment is relatively simple by arthroscopic debridement, removal of the fibrous nodule along the undersurface of Quadriceps tendon [2]. While, fracture of Post of Polyethylene liner is a rare occurrence along with presence of PCS and is rarely reported after TKA even radiologically.
We report a clinical case of a 65-year-old Male of Indian origin with Bilateral Patellar Clunk Syndrome along with fracture of post of Polythylene Liner of right as well as Left knee.
Here, the patient’s both knees were completely stable and the only complaint was locking of both knees (right more than left) with a click sound while standing from sitting position associated with mild pain. The patient was ambulatory and had complete Knee range of motion without any reported instability. Patient had a history of TKA (PFC Sigma, DePuy implant) ten years ago.
Patient reported to Orthopaedic OPD of our hospital with above mentioned complaint. Clinically patient was suspected with Patellar clunk syndrome and for confirmation Patient was referred to the Radiology department. X-rays (Figure 1, Figure 2 and Figure 3) and MRI MARS protocol was performed at 3-T (ACHIEVA, Philips Medical Solutions) including T1-weighted, axial T2-weighted, coronal T1-weighted, and sagittal T2-weighted turbo spin echoes and coronal Short Tau Inversion Recovery (STIR) sequences.
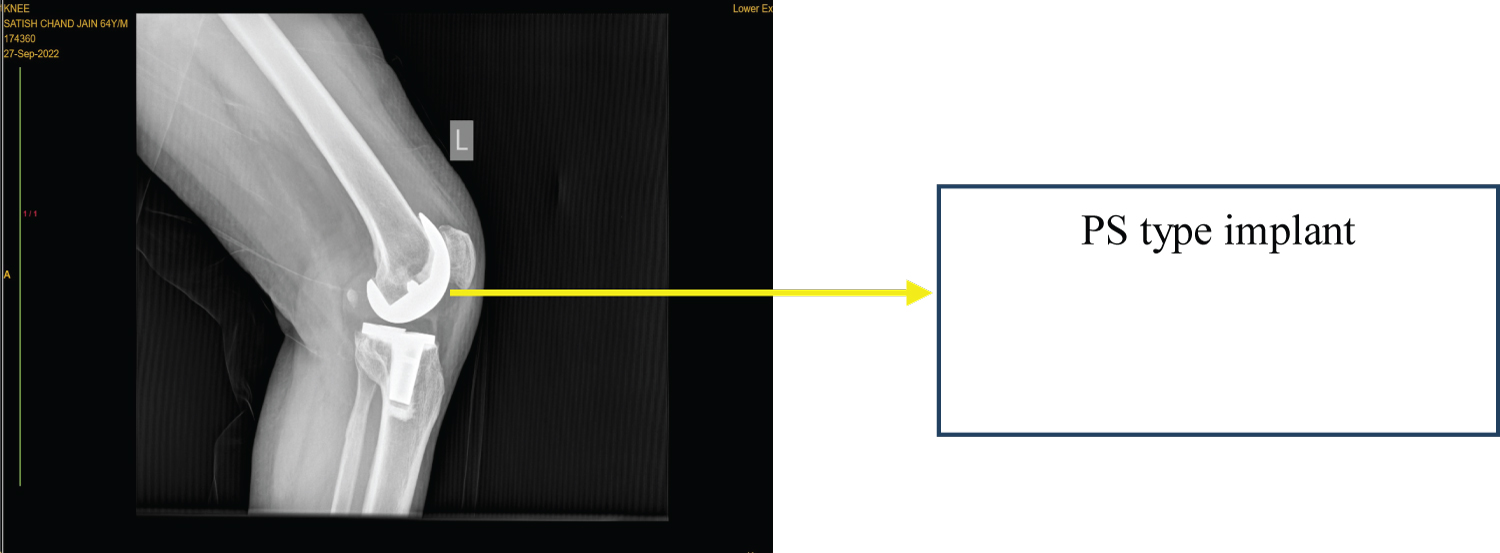 Figure 1: Lateral view (Left knee).
View Figure 1
Figure 1: Lateral view (Left knee).
View Figure 1
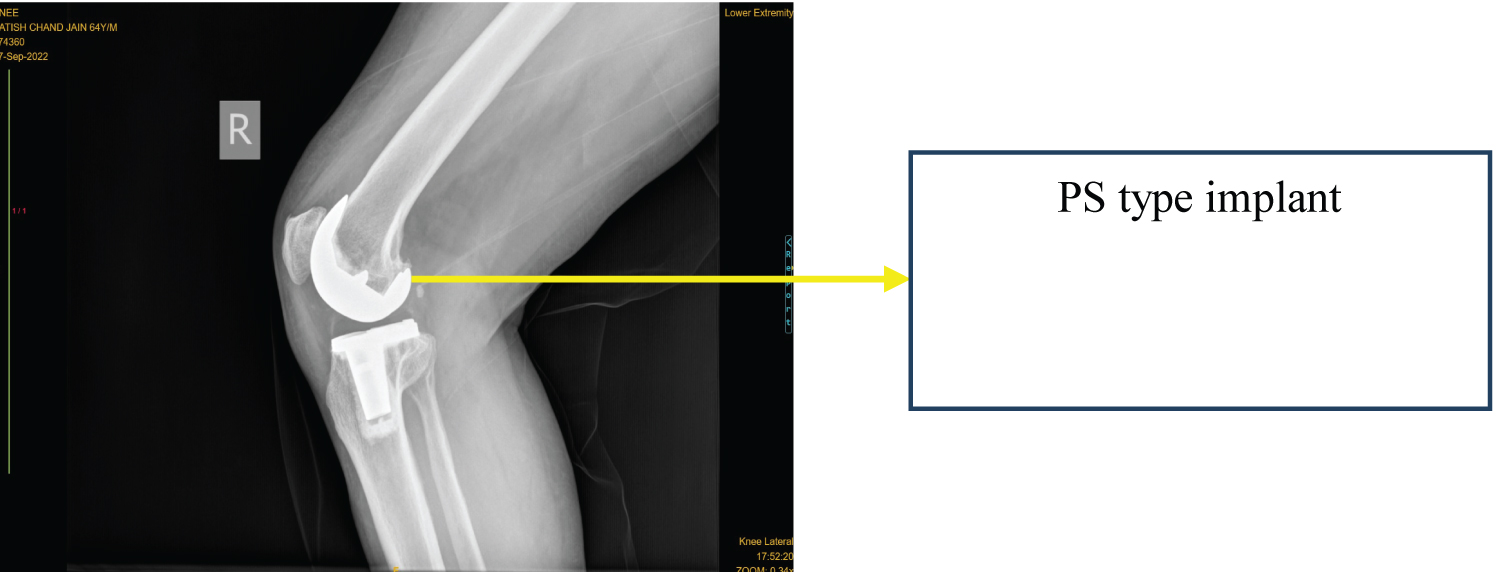 Figure 2: Lateral view (Right knee).
View Figure 2
Figure 2: Lateral view (Right knee).
View Figure 2
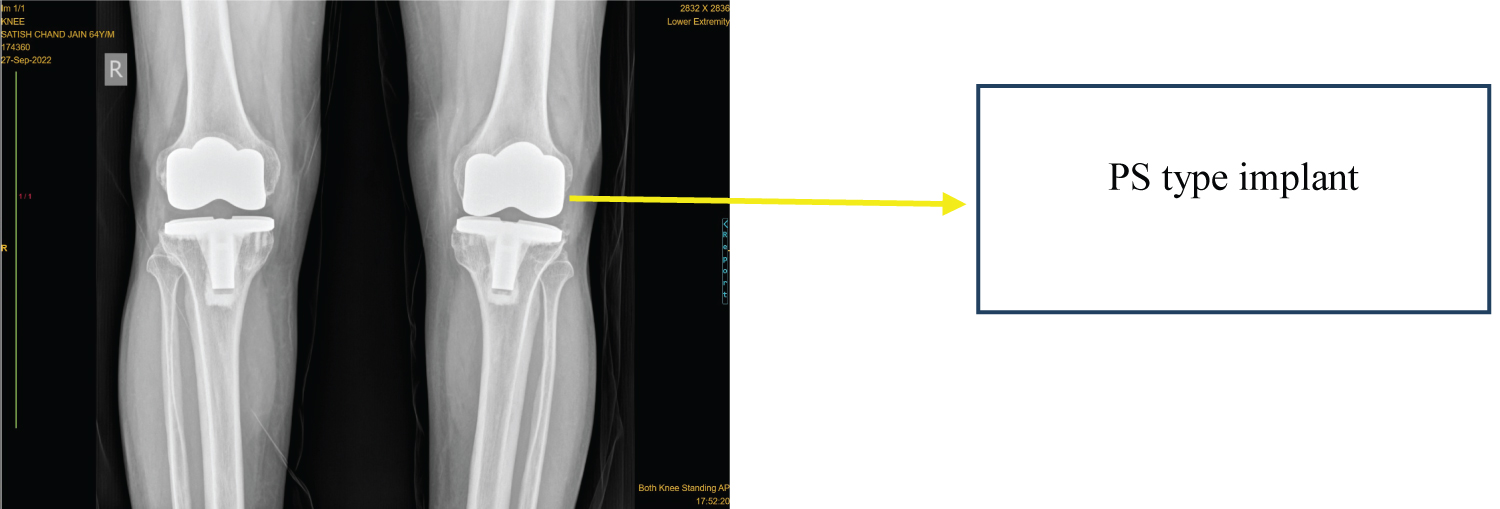 Figure 3: Anterolateral view (Both knees).
View Figure 3
Figure 3: Anterolateral view (Both knees).
View Figure 3
In our case MRI was done and size of soft tissue masses proximal to the patella were determined in sagittal and axial MRI views (Figure 4, Figure 5, Figure 6 and Figure 7). The nodule tissue was characteristically of intermediate signal intensity on the moderate echo time pulse sequence, characteristic of synovial scarring. A correlation ultrasound (Figure 8) was also undertaken and the soft tissue nodule was observed in suprapatellar region. Both MRI and ultrasound findings in our case are similar as in literature in patellar clunk syndrome. Fracture of post of polythylene liner was not detected on MRI as well as on USG.
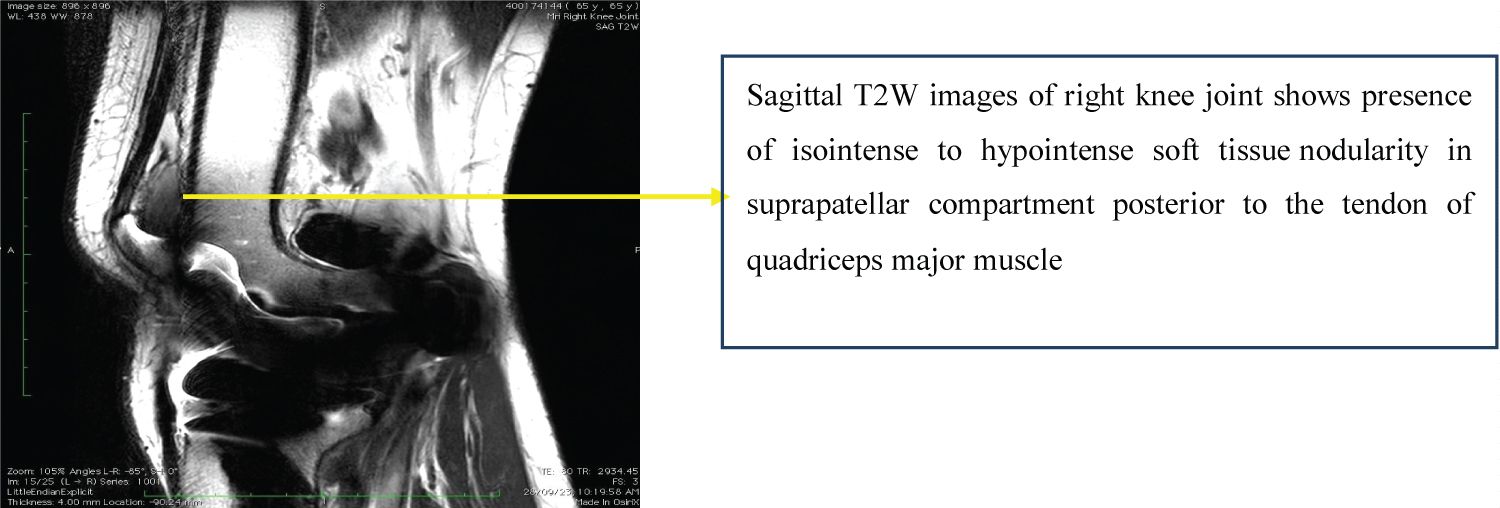 Figure 4: MRI (Right knee, Sagittal view).
View Figure 4
Figure 4: MRI (Right knee, Sagittal view).
View Figure 4
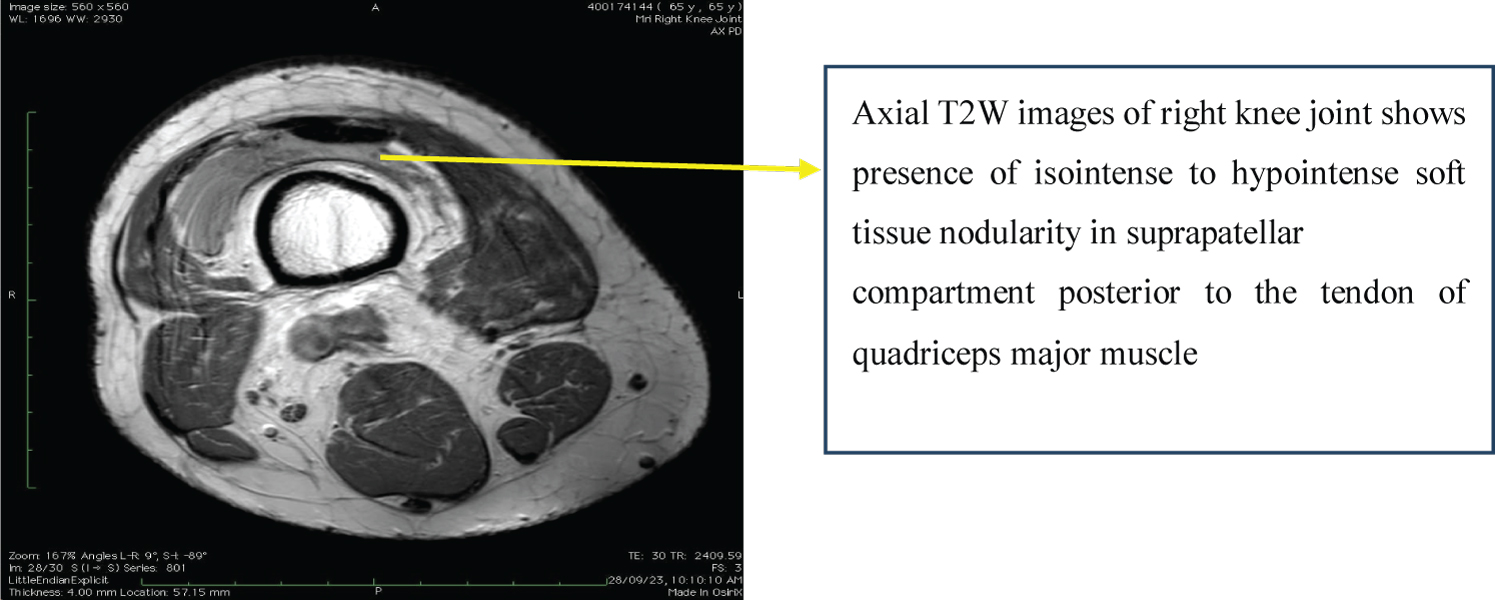 Figure 5: MRI (Right knee, Axial view).
View Figure 5
Figure 5: MRI (Right knee, Axial view).
View Figure 5
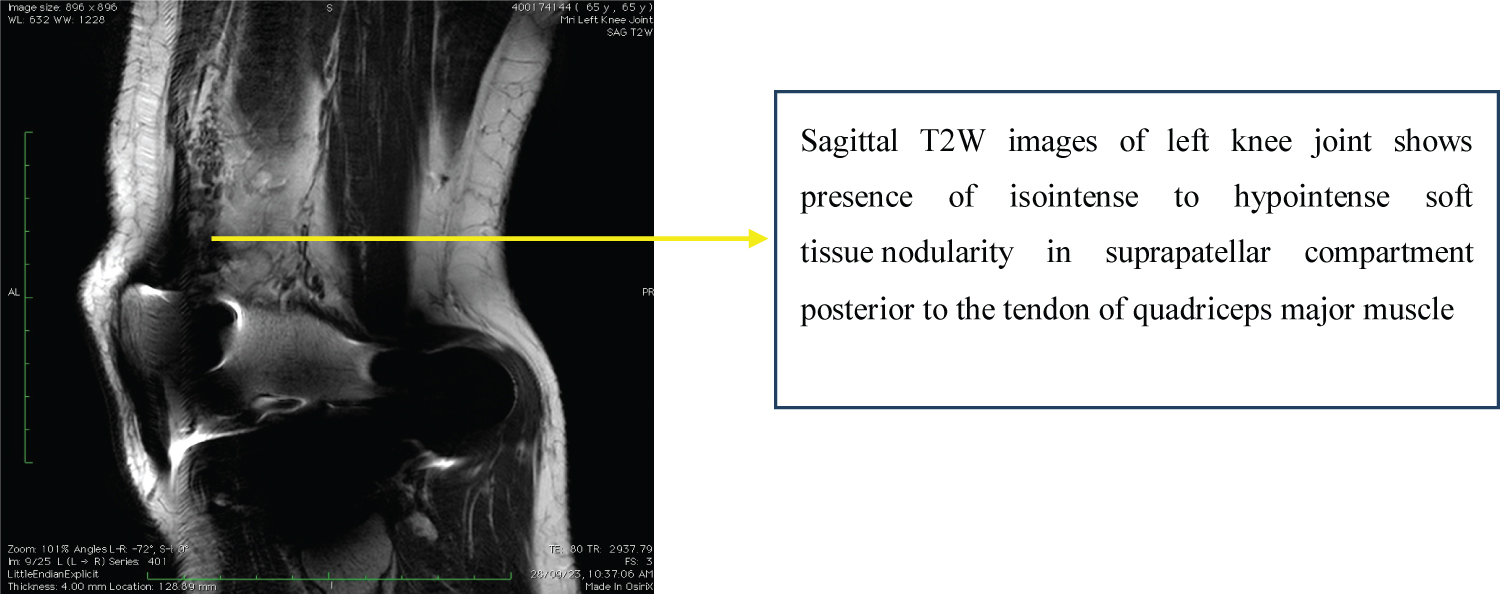 Figure 6: MRI (Left knee, Sagittal view).
View Figure 6
Figure 6: MRI (Left knee, Sagittal view).
View Figure 6
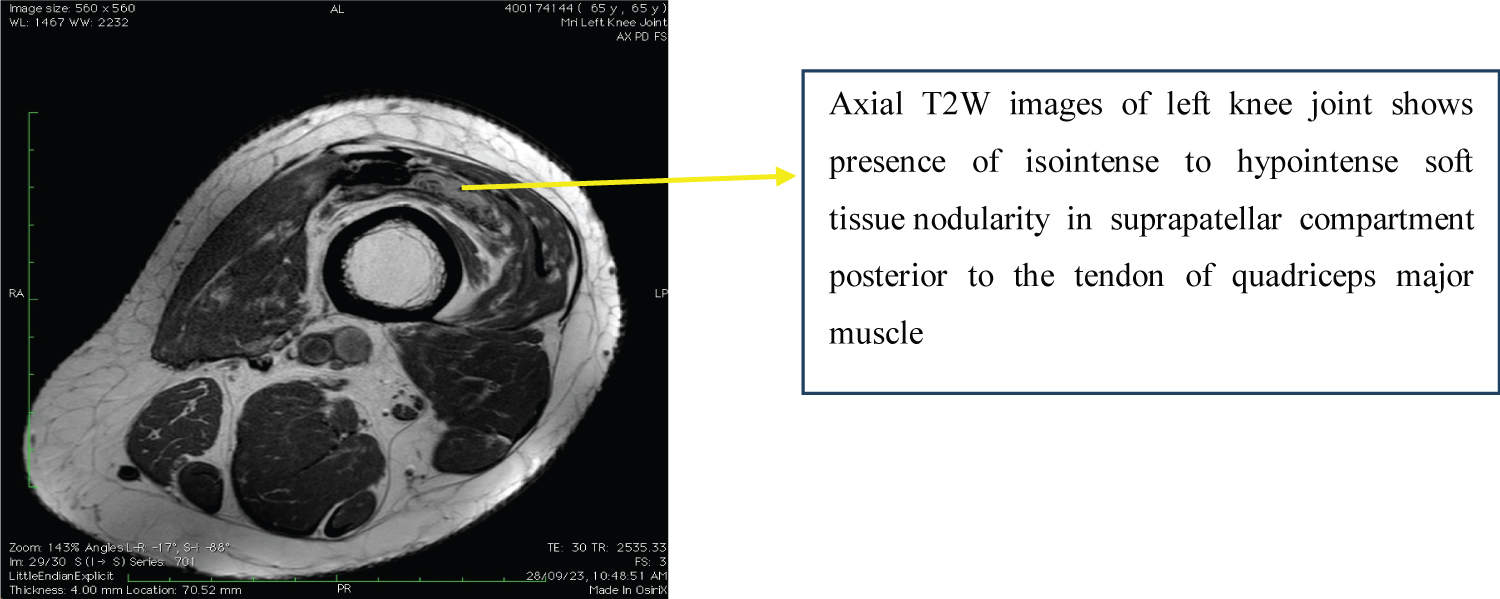 Figure 7: MRI (Left knee, Axial view).
View Figure 7
Figure 7: MRI (Left knee, Axial view).
View Figure 7
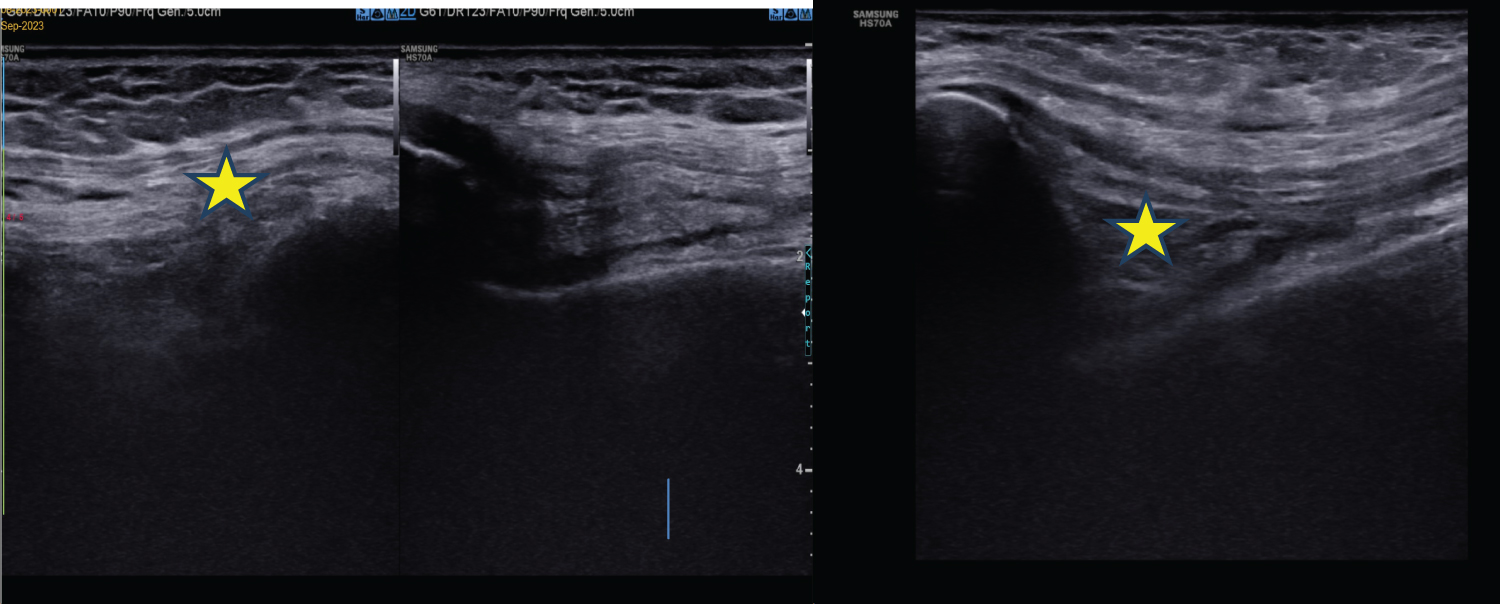 Figure 8: Ultrasound B/L knee joint shows presence of irregular hypoechoic soft tissue component in suprapatellar compartment posterior to quadriceps tendon.
View Figure 8
Figure 8: Ultrasound B/L knee joint shows presence of irregular hypoechoic soft tissue component in suprapatellar compartment posterior to quadriceps tendon.
View Figure 8
Once patient was diagnosed with PCS, he was taken for arthroscopic debridement where the surgeons also observed fracture of Post of Polyethylene liner (Figure 9 and Figure 10) along with PCS which was eventually removed.
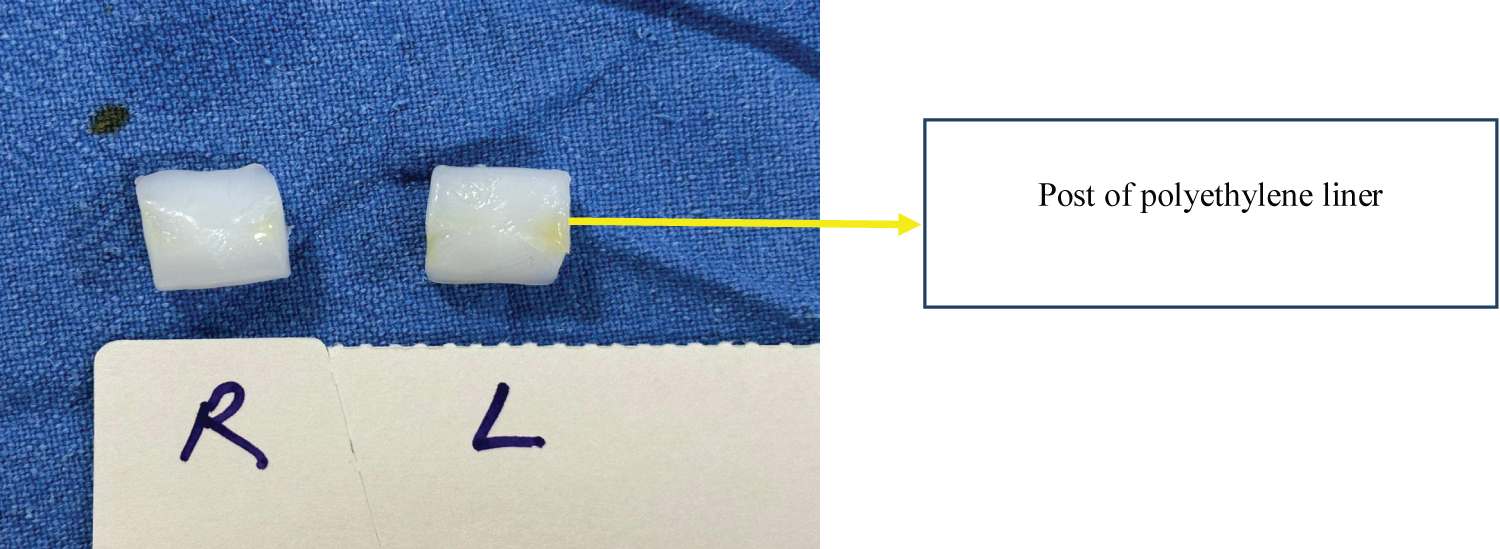 Figure 9: Fracture cam post of polyethylene liner (Right, Left).
View Figure 9
Figure 9: Fracture cam post of polyethylene liner (Right, Left).
View Figure 9
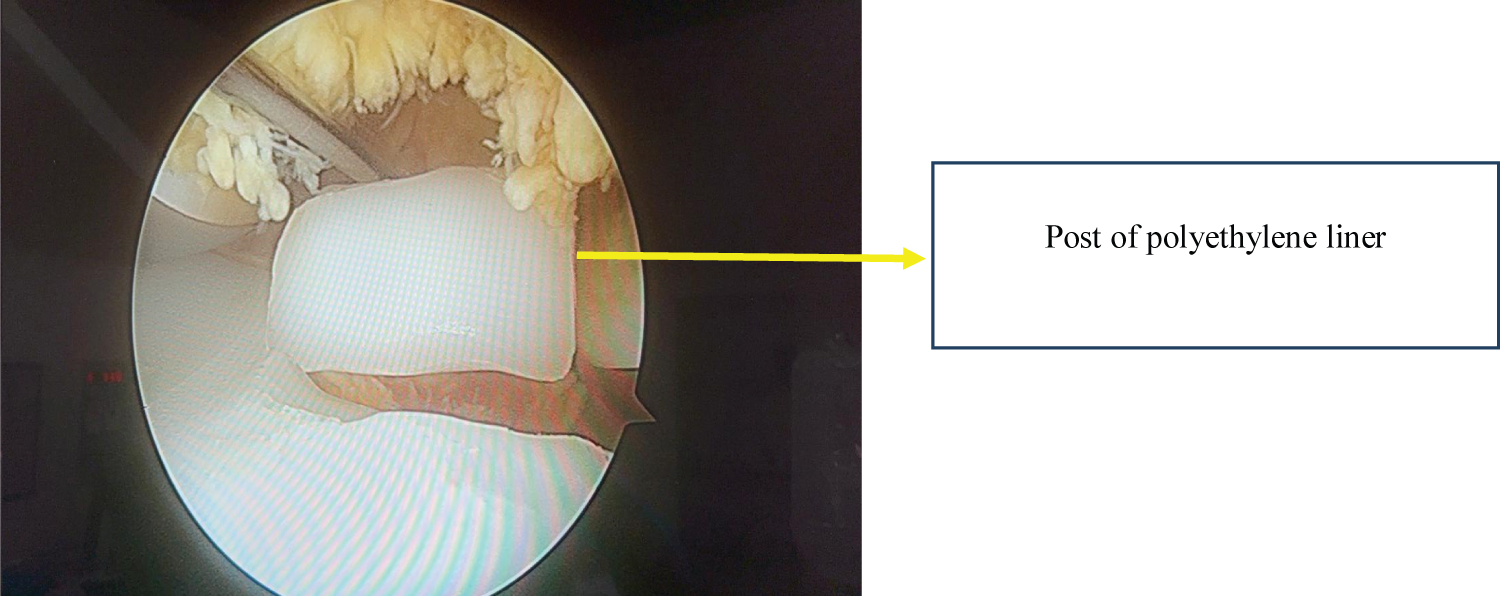 Figure 10: Arthroscopic view of fracture cam post of polyethylene liner.
View Figure 10
Figure 10: Arthroscopic view of fracture cam post of polyethylene liner.
View Figure 10
Here, MRI and Ultrasound findings were consistent with PCS. This lead to the operative treatment with arthroscopic debridement. Patient also achieved complete Range of Motion without any further clunk sound (Figure 11).
 Figure 11: Range of motion (Right, Left).
View Figure 11
Figure 11: Range of motion (Right, Left).
View Figure 11
Till date, here are many documented publications around usage of MARS protocol of MRI in diagnosis of PCS. At the same time, here is dearth of literature on the role of MARS MRI in diagnosing Fracture post of polyethylene Line in PCS. A metal artifact reduction sequence (MARS) is intended to reduce the size and intensity of susceptibility artifacts resulting from magnetic field distortion. A variety of techniques are used for reducing metal artifacts at MRI, both for addressing artifacts due to the presence of metal in the image plane (in-plane artifacts) and for artifacts due to metal in an adjacent plane (through-plane artifacts).
PCS is a postoperative complication of TKA [3]. While the exact etiology behind the formation of the nodule is unclear, it is thought to arise either due to the placement of a patellar button when the patella is resurfaced or due to the design and geometry of the intercondylar notch of the femoral prosthesis or can occurs due to development of fibrous nodule at the junction of the posterior aspect of the quadriceps tendon and the proximal pole of the patella [3]. With flexion of the knee, this nodule enters the intercondylar notch of the femoral prosthesis. As the knee is extended, the nodule becomes entrapped within the notch as the quadriceps tendon and the patella migrate proximally [10,11]. At 30-45° from full extension, enough tension is placed on the fibrous nodule to cause it to clunk out of the intercondylar notch [12] and these patients may present with painless or painful clunk and/or catching of the patella prosthesis as the knee is actively extended from a flexed position. Pain is often localized to the anterior aspect of the knee2 and persistent symptoms may be managed by open or arthroscopic debridement of the fibrous nodule.
Newer techniques of MRI such as Multi Acquisition Variable-Resonance Image Combination (MAVRIC) and Section Encoding for Metal Artifact Correction (SEMAC) have shown to reduce to susceptible artifacts providing high-resolution images with exceptional osseous and soft tissue contrasts6. Thereby drastically improving MRI imaging along with implant-tissue interfaces. Although (SEMAC & MAVRIC) techniques of MRI are not performed at our Institute, we were able to diagnose PCS using MARS technique of MRI with good correlation using Ultrasound. All diagnostic that were used had limited role in assessing fracture of Post of Polyethylene Liner.
A study by Kumar, et al. [13], reported a case of fracture of Tibial polyethylene post fracture in 56-year-old women with posterior stabilized TKA following minor trauma. Here, they suggested that diagnosis of fracture CAM may be made over plain radiograph when knee is placed in more than 90 degrees of flexion (posterior subluxation of femoral component) or computed tomographic arthrography.
MRI is effective in the confirmation of clinically evident PCS after TKA by directly visualizing the intra-articular soft tissue proliferation proximal to the patella, thereby directing appropriate management and MRI is a powerful tool for assessment of a painful TKA. However, Ultrasound can also be considered as a diagnostic tool in suspected case of PCS, as it can also detect soft tissue in suprapatellar region given the cost effectiveness, less time consumption and ease of availability of the modality.
Indications for MRI following TKA are still getting established with the advent of new pulse sequences and technical refinements in MRI.
As in our case fracture post polyethylene liner was also detected during Arthroscopy, which stresses on the importance of further development in advance imaging to address issues of Polyethylene fracture for appropriate evaluation and diagnosis. We may also suggest that Orthopaedicians should clinically look for other abnormalities related to native implant during Arthroscopy along with debridement of soft tissue nodule related to PCS in Posterior Stabilized TKA design.