The measurement of heart rate variability (HRV) allows a noninvasive investigation of the functioning of the autonomic nervous system, especially the balance between sympathetic and vagal activity. Pregnancy after bariatric surgery has some peculiarities that may interfere with its course and evolution. Studies have investigated the variability of maternal heart rate and its relationship to the prognosis for pregnancy development about the risks of eclampsia and pregnancy complications. This paper proposes to present data from the autonomous system of post-bariatric pregnant women over the nine months to 15 days after delivery, based on the analysis of heart rate variability. Collections were carried out once a quarter and after delivery, along with filling out a questionnaire at each meeting. They were further analyzed applying signal processing tools to extract statistical features. The highest HRm value at rest was in the 3rd trimester, even with the self-report of feeling well. The highest sympathetic activation occurred in the 2nd trimester, both at baseline and in the active stand test. Running 15 days postpartum, the increase in baseline sympathetic modulation remained. It was possible to verify the autonomic alteration during pregnancy and up to 15 days after childbirth in post-bariatric pregnant women.
Pós-bariatric, Pregnant, Heart rate variability, Case report, Autonomic nervous
Pregnant women after bariatric surgery have reduced risks related to the comorbidities of obesity itself, but, on the other hand, as a result of the surgery, they are susceptible to nutritional deficiencies that may complicate the healthy development of the fetus [1].
The typical pregnancy is inextricably linked to changes in the woman's body, including physiological, metabolic, hormonal [2], emotional and psychological [3]. In this line, pregnancy causes several hemodynamic changes, including an increase in heart rate, plasma volume and cardiac output, in addition to attenuating systemic vascular resistance and mean arterial pressure [4-7].
Changes in the cardiovascular system associated with pregnancy, with hemodynamic repercussions, are intrinsically related to the modulation of the activity of the sympathetic and parasympathetic systems [8]. The antagonistic oscillatory relationship of the sympathetic and parasympathetic (vagal) branches of the autonomic nervous system over the sinus node can be estimated by measuring heart rate variability (HRV) [9-11]. Several studies have already sought to assess variations in HRV during pregnancy [12-17]. This way, differences in HRV seem to be more significant than the increase in heart rate and volumetric load also identified by the end of the 2 nd trimester in normal pregnancy [18].
The alterations express the organism's physiological adaptation, and which were associated with a normal pregnancy with a facilitation of sympathetic regulation, expressed by an increase in the low frequency component (low frequency - LF) and attenuation of the parasympathetic influence, characterized by a decrease in RMSSD, pNN50 and HF (high frequency - HF) [13]. Such alterations may be due to the mechanical-electrical feedback evoked by the elongation of the sinoatrial node observed in pregnancy [13,19].
Few studies have been carried out analyzing the effect of bariatric surgery during pregnancy, and no study was found analyzing from the perspective of this follow-up through HRV, with metrics in the domain of time and frequency. It is understood that there is a scarce window of data on the state of cardiac regulation in pregnant women after bariatric surgery, throughout the entire pregnancy. Thus, given the character of the theme of HRV in post-SB pregnant women; longitudinal follow-up during pregnancy; the number of evaluations carried out, including a postpartum one as well; the protocol used, including the baseline assessment, in the sitting and orthostatic position, and guided deep breathing, are different from what has been found in the literature so far.
The aim of this study was to analyze the cardiac autonomic control of a post-bariatric pregnant woman, throughout different stages of pregnancy, longitudinally.
The case study research is characterized as to the approach as quali-quantitative; of an applied nature and with an exploratory objective.
The research project was submitted to the Research Ethics Committee through Plataforma Brasil and was approved under CAAE No. 25764819.6.0000.5505. To carry out the research, the precepts of Resolution 466/12 of the National Health Council were respected, in which the participation of the subjects occurred by signing the Informed Consent Form elaborated for the specific purposes of this research, guaranteeing anonymity to the participants as well.
The research consisted of collecting data at four different times: 1 st trimester of pregnancy (with 7 weeks), 2 nd trimester (20 weeks), 3 rd trimester (37 weeks) and 15 days after delivery.
The following precautions and recommendations for the pregnant woman were carried out during all appointments:
• Not having performed heavy aerobic exercise for at least one hour before the assessment.
• Must not have consumed coffee, tea or other caffeinated beverages within an hour of the assessment.
• No cigarettes should be smoked for at least thirty minutes before the assessment.
• Wait at least 1.5 hours after a heavy meal to do the assessment.
• For repeat measurements, it is best to acquire them at the same time of day to avoid circadian variation in heart rate and HRV.
• Inform about the use of any medication, before the evaluation.
In the first data collection of the 1 st trimester, the pregnant woman answered a questionnaire with identifying information (name, date of birth, education, profession, address and telephone); medical history (height, weight, previous pregnancies and illnesses); data on the current pregnancy (whether it was scheduled, when it was discovered, data up to the time of the first session, nausea, mood swings, sleep characteristics, delivery expectations, fluid intake, physical activity, bowel function, psychological aspects, medications).
In subsequent meetings, data on the evolution of pregnancy were collected, such as: Complications, risk factor, rest, medication, gestational age and weight, nausea, fluid intake, bowel function, mood, sleep.
In the postpartum session, data on the delivery and the newborn were collected, such as: Gestational age at which the NB was born, type of delivery, pre-delivery and current weight, delivery time, intercurrence, length of stay, postpartum recovery, postpartum depression, breastfeeding, fluid intake, mood, sleep, NB APGAR, gender, weight and length, whether there was a need for a neonatal ICU or incubator, complications.
In every evaluation, there was a topic of data about how the patient was feeling at the time of collection: if she was feeling sick and if she had slept well the night before.
The assessment of autonomic control was performed from heart rate recordings performed continuously using the HeartMath emWave pulse interval acquisition system (sampling frequency of 370 Hz), with the photoplethysmograph placed on the earlobe and the recording it was done in the morning.
Records were made in three situations: (1) Baseline assessment with the patient sitting for 3 minutes; (2) Baseline assessment with the patient in the standing position for 3 minutes, and (3) Assessment with guided breathing for 3 minutes with a pacer with the patient in the sitting position.
RR data.txt files were exported from the emWave Pro Plus (version 3.12.0.11458; HeartMath LLC, Boulder Creek, EUA) app then processed by Kubios HRV Premium Software version 3.5 (Biosignal Analysis and Medical Imaging Group, Department of Physics, University of Kuopio, Kuopio, Finland). Stationary stretches of 256 beats were selected in each protocol situation. The spectra of the time series of pulse intervals, referring to each selected segment, were quantitatively evaluated considering the heart rate variability values, normalized powers of the LF and HF frequency bands and the relationship between the powers of the LF/HF components (balance sympathovagal).
The frequency bands analyzed were: VLF (0-0.04Hz), LF (0.04-0.15Hz) and HF (0.15-0.40Hz) [18,20].
Female, 24-years-old, completed 3 rd degree (bachelor's degree in administration), 1.65m tall, weighed 63 kg before becoming pregnant, post-bariatric patient, no history of disease, non-smoker, sedentary. The gastrectomy surgery was performed 1 year and 9 months before she became pregnant. The patient was unable to inform whether the technique used in the gastrectomy was partial or by-pass. There was no occurrence of postpartum depression or risk complications at the time of delivery and/or after.
st trimester gestational data: Performed at 7 weeks, the patient weighed 62 kg (lost 1 kg after becoming pregnant), did not complain of nausea, reported ingesting an average of one liter of water per day, bowel function with a frequency of 1 to 2 times a week, quality of sleep bad, no mood swings. On the day of data collection, she said she was feeling sick and had slept badly at night.
2 nd trimester gestational data: At 20 weeks, weighing 67 kg, with no report of need for rest or risk intercurrence, she reported having dizziness; absence of nausea; making use of ferripolymaltaser (myrafer), vitamin supplement (baristar) and vitamin D 7000 IU, according to medical indication; not performing physical activity, maintained intake of one liter of water daily, bowel function 1 to 2 times a week; no perception of mood change; sleep quality reported as poor.
On that collection day, the patient reports having felt palpitations and feeling sick, described as tiredness and the feeling that she was going to faint, about 20 minutes before our consultation.
3 rd trimester gestational data: Pregnancy at 28 weeks, weighing 74 kg, absence of rest or intercurrence, presence of nausea eventually, without physical activity, maintained daily intake of one liter of water, bowel function 1 to 2 times a week, perception of mood swings eventually, sleep quality improved and was considered good. On the day of collection, she reported feeling well and that she had slept well the night before. He complained that sometimes, especially after meals, he felt his heartbeat speed up; such a report was not observed in today's collection.
Pregnancy at 37 weeks, weighing 79 kg, no rest or intercurrence, no nausea, no physical activity, maintained daily intake of one liter of water, bowel function 3 to 4 times a week, no change in mood, quality of sleep considered as regular. On the day of collection, he reported feeling well and that he had slept well the night before.
Postpartum data: Performed 15 days after delivery, weighing 73 kg (in the week of delivery she was 80 kg, in a total gain of 17 kg during the entire gestational period), reported drinking 2.5 to 3 liters of water daily, bowel function 3 to 4 times a week, without mood swings and poor sleep quality due to the baby crying a lot at night due to colic.
Regarding the delivery, she informed that it was at 39 weeks, a cesarean section was performed because the baby was very high and not in the expected pelvic position. She reported good postpartum recovery and no complaints of postpartum depression.
Newborn, female, was born with a length of 49.5 cm and 3170g, without intercurrence of risk and without the need for an incubator and/or prolonged hospitalization, with an APGAR score of 9-9. Patient remained not doing any physical activity during pregnancy and after.
Analyses of cardiac autonomic modulation are represented in Table 1.
Table 1: Spectral analysis on frequency domain in the 1T, 2T, 3T and PP intervals. View Table 1
The power spectrum of the high-frequency (HF) band, expressed in normalized units (HFnu), was significantly greater after deep breathing than at rest and after the active stand test (P = 0.008) for 1T, 2T, 3T, and PP measures. Também há diminuição significative da HF (nu) do 1° para o 3° trimestre de gestação.
The respiratory rate was significantly lower during deep breathing than at rest and during active stand test for 1T, 2T, 3T, and PP measures (P = 0.001).
About mean heart rate (HRm), the highest heart rate captured at rest was in the 3rd trimester, even with the patient reporting self-perception of feeling good and having slept well. Regarding the deep breathing test, the highest HRm index was in the 1 st trimester of pregnancy. It is noticed that in the postpartum moment it was the one with the lowest HRm in the active stand test and that this test in all periods was what can be considered the most stressful causing an increase in HRm, as shown in Figure 1.
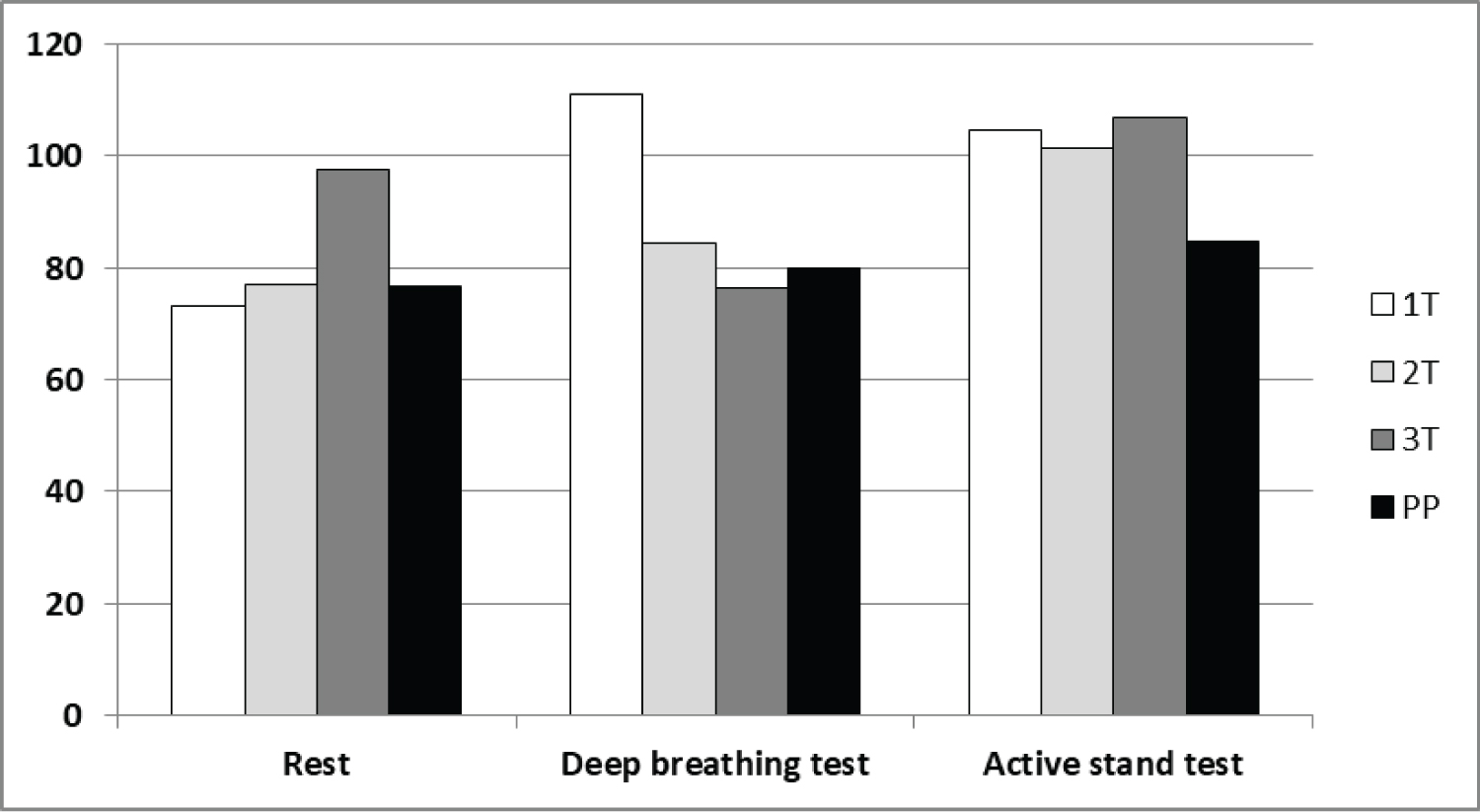 Figure 1: Heart Rate at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals.
View Figure 1
Figure 1: Heart Rate at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals.
View Figure 1
Regarding sympathetic modulation, it can be seen in Figure 2 that the 2 nd trimester was the one with the highest sympathetic activation both in the resting test and in the active stand test. It turns out that deep breathing, in all periods, causes a large decrease in sympathetic modulation. The 3 rd trimester was the gestational period that had the lowest sympathetic activation in the deep breathing and active stands tests. There is an increase in baseline sympathetic modulation during pregnancy that remains 15 days after delivery.
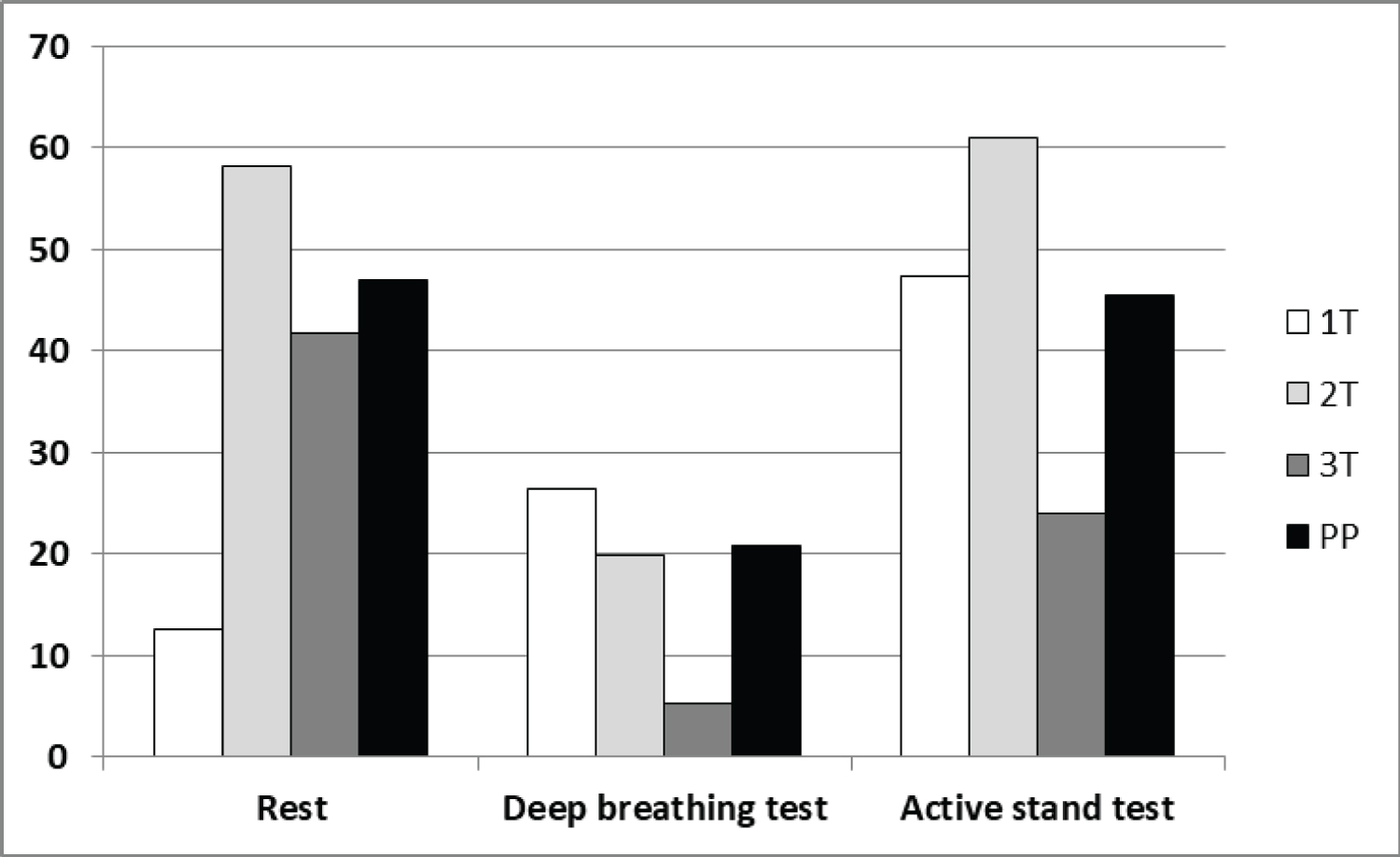 Figure 2: Sympathetic modulation, expressed by LF nu (power spectrum of Low Frequency component in normalized units), at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals.
View Figure 2
Figure 2: Sympathetic modulation, expressed by LF nu (power spectrum of Low Frequency component in normalized units), at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals.
View Figure 2
It can be seen in Figure 3 that there is a large increase in vagal modulation in the guided deep breathing test, inversely proportional to the active stand test. The 3 rd trimester showed the greatest sympathetic activation in the deep breathing and active stand tests, in which this antagonistic relationship with what is shown in Figure 2 is expected.
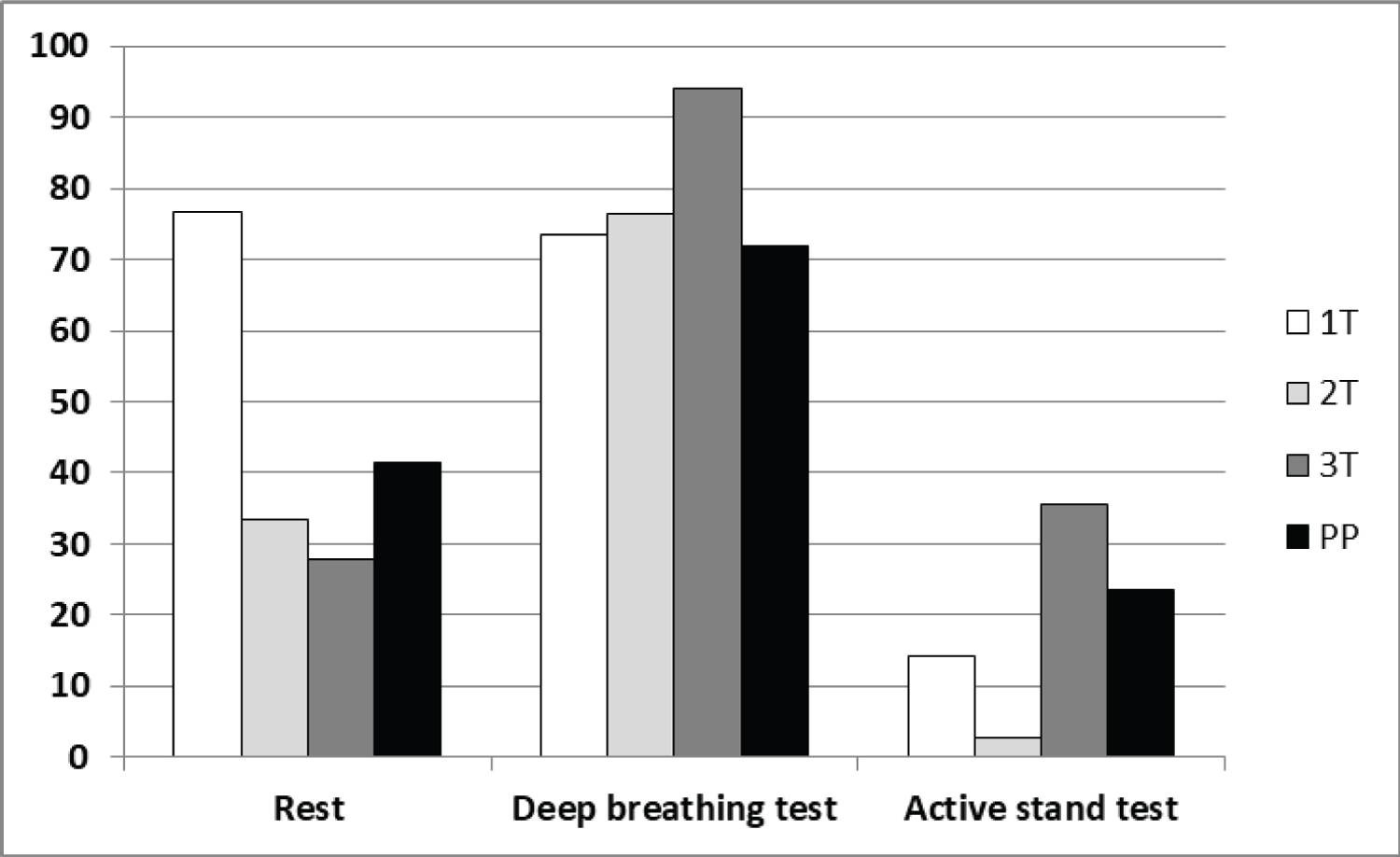 Figure 3: Vagal modulation, expressed by HF nu (power spectrum of High Frequency component in normalized units), at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals. There is a statistically significant difference (P = 0.024) in deep breathing condition, compared to a rest and stand test.
View Figure 3
Figure 3: Vagal modulation, expressed by HF nu (power spectrum of High Frequency component in normalized units), at rest and after deep breathing and active stand tests, in the 1T, 2T, 3T and PP intervals. There is a statistically significant difference (P = 0.024) in deep breathing condition, compared to a rest and stand test.
View Figure 3
The impact of different bariatric procedures on pregnancy and fetal outcome also be discussed, as well as general considerations on monitoring and managing post-BC pregnancies [21]. Most pregnancies after bariatric surgery have successful outcomes with decreased occurrence of gestational diabetes and hypertension and lower birth weight compared to control patients [21-23].
Pregnancy after bariatric surgery has some peculiarities related to obesity, type of surgery, amount of weight loss, time elapsed since surgery and adherence to medical prescriptions [24,25]. Findings highlight the importance of a healthy lifestyle and multidisciplinary prenatal care [26]. In this case study, the patient had good prenatal attendance, but attention is drawn to the absence of physical activity during pregnancy and the total weight gain of 17 kilos.
The findings of this study, even in a post-bariatric pregnant woman, corroborate with other studies of pregnant women [18,27-29] with regard to the decrease in HRV and lower sympathetic modulation in the 2 nd trimester of pregnancy, in opposition to the findings of another study in which the decrease in HRV occurred in the 3 rd trimester [30]. However, it corroborates the finding of this study regarding the LF/HF ratio, which is lower in the 1 st trimester and increases significantly in the 2 nd and 3 rd trimester [30]. The significant decrease in FH (nu) from the 1 st to the 3 rd trimester of pregnancy corroborates the findings of another study [31].
In this case study, the pregnant woman did not have gestational hypertension or diabetes, corroborating findings from other studies [20,21,32-34], and no heart changes [35]. Um estudo realizado comparando dados do sistema cardiovascular de gestantes sem e com bariátrica, todas com a mesma faixa de IMC pré-cirurgia, mostraram uma melhor adaptação cardiovascular nas gestantes CB em comparação com as grávidas sem cirurgia para perda de peso [36].
The fetus is at high risk of prematurity and fetal growth restriction but appears to have no increased risk of birth defects, which is in line with the findings of our case study, where the newborn's APGAR score was 9, with weight within the expected range for gestational age, in opposition to the findings of other studies in which babies had lower weight for gestational age in CB pregnant women [21].
Regarding the evaluation of the pregnant woman in the orthostatic position, studies mentioned the importance, as the orthostatic test provides information on the baroreflex and sympathetic control in hemodynamics [7,27,37]. Standing position is adopted in the assessment to increase sympathetic tone [37] and, active orthostatism induces, in the early stages of pregnancy, a significant increase in the LFRR and LF/HF ratio and a reduction in the HFRR [7].
It is noteworthy that, with the exception of the 1st semester, at all other times, the deep breathing test showed less sympathetic modulation and a large increase in parasympathetic modulation, validating findings that indicate decreased sympathetic activity with guided slow breathing [38].
As a suggestion for future research, an indication was found that HRV is an important tool in the analysis of the evolution of pregnancy and even in the diagnosis [39]. It should be noted that although HRV analysis is not a new area, several topics remain open for discussion: Predictability of pathological events, sympathetic/parasympathetic balance, as well as the influence of various factors such as maternal age, smoking, parity, fetal sex and family history of hypertension or diabetes [40].
In view of all the data presented, no finding was found that was contrary to reports in the literature regarding the sympathovagal balance in normal pregnant women. Another point to be discussed is that 15 days after delivery were not enough for the return of parasympathetic modulation values at rest equal to those presented at the beginning of pregnancy.
The authors would like to thank Dr. Orlando Freire de Faria Jr. for him help in implementation this research and get all the pregnant who took part in the study.
Tavares RSCR, Cunha TS, Casali KR: Formal analysis (equal), investigation (equal), methodology (equal), writing-original draft (equal) and writing-review and editing (equal). All authors provided substantial contributions to the manuscript. They reviewed and approved the final version of the manuscript, and they guarantee the integrity of the article.
None.
None.