Quality, cost, and access are the three primary metrics of the healthcare system. In recent years, the healthcare system has begun to feel a greater push to provide a higher quality of care as payors have adopted Quality-Based metrics and incentive measures. With an expected shortage of up to 48,000 physicians by 2034 [1], a multidisciplinary approach will be crucial in continuing the push to provide high quality care. As the role of a pharmacist continues to evolve towards direct patient care, pharmacists with expertise in medication management are well equipped to serve as an integral part of the healthcare team.
One of the first examples of a value-based, quality-led incentive program was the introduction of the Centers for Medicare & Medicaid Services (CMS) Star Rating system in 2007. CMS created the Part C and D Star Ratings to provide quality and performance information to Medicare beneficiaries to assist them in choosing their health and drug services during the annual fall open enrollment period. Star Ratings include a maximum of 9 domains comprised of a maximum of 40 measures. Measures are assigned a weight of 1, 2, 3, or 5, depending on their value. A measure given a weight of 3 counts three times as much as a measure given a weight of 1. The weighted average of these measures comprises the plan’s overall Star Rating. Health plans are rated annually on a scale of 1 to 5 stars, with 1 star representing poor performance, 3 stars representing average performance, and 5 stars representing excellent performance [2]. Plans that consistently perform high are given incentive bonuses which are returned to beneficiaries in the form of additional benefits, such as reduced co-payments or expanded coverage. Moreover, plans that receive five stars are eligible to enroll patients year-round, increasing their enrollment number and reimbursement. Indirectly, providers can also increase their patient base and incentive potential. Star Rating measures also overlap with other value-based programs scoring criteria, allowing providers to benefit financially. On the other hand, if a plan receives a low Star Rating (less than three stars) for three years in a row, they are placed in a probation period with the possibility of contract termination [3].
Approximately one-half of the CMS Star Rating quality measures can be directly impacted by a pharmacist [4]. In the Star Rating system, medication adherence is a triple-weighted measure and measures the Proportion of Days Covered (PDC) rate for oral anti diabetic medications, anti hypertensive medications Rein-Angiotensin System (RAS) antagonists and statins. An additional triple-weighted measure is HbA1c control which is defined as the percentage of members aged 18-75 with diabetes whose most recent HbA1c is 9% or less [2]. By implementing appropriate pharmacological interventions, ensuring completion of preventative screenings and vaccinations, and providing comprehensive patient education to increase medication adherence, pharmacists can have a direct impact on CMS Star Rating quality measures.
In 2021, a hospital-based ambulatory care pharmacy department partnered with eight providers at five different family medicine clinics to help satisfy CMS Star Rating quality measures. A collaborative practice agreement was created and signed by the eight providers allowing pharmacists in the clinic to adjust diabetes medications, order necessary labs and durable medical equipment, and provide new and refill prescriptions. During the initial pilot program, conducted from December 15, 2021, to May 25, 2022, pharmacists focused on one triple-weighted Star measure: C11: Diabetes Care - Blood Sugar Controlled. This measure includes the percentage of diabetic Medicare Advantage enrollees aged 18-75 whose most recent HbA1c level is greater than 9%, or who were not tested during the measurement year. Five hundred thirty-eight patients were screened for eligibility. One hundred ninety patients met inclusion criteria and were contacted by a pharmacist for enrollment. One hundred eleven patients received pharmacist intervention. By the end of the study period, pharmacist intervention led to sixty patients meeting the quality measure of HbA1c 9% or less. Of those sixty patients, five patients had a repeat A1c completed during the study period, with an average reduction of 3.74% [5].
Based on the positive results and at the request of the primary care physicians, the service was continued and expanded to include eight quality measures: D08: Medication Adherence for Diabetes Medications, D09: Medication Adherence for Hypertension (RAS antagonists), D10: Medication Adherence for Cholesterol (Statins), D12: Statin Use in Persons with Diabetes (SUPD), C09: Diabetes Care- Eye Exam, C10: Diabetes Care - Kidney Disease Monitoring, and C03: Annual Flu Vaccine. From October 21, 2022, to December 31, 2022 one hundred sixty-five patients were screened for eligibility. One hundred six patients met inclusion criteria and were contacted by a pharmacist for intervention.
Interventions included patient education, patient reminder, sent lab order, CPT level 2 supplementary tracking code billed to satisfy the measure, or prescription ordered (Figure 1). By December 31, 2022, the following measures were satisfied: Medication Adherence for Diabetes Medications 100% (n = 14), Medication Adherence for Hypertension - RAS antagonists 100% (n = 8), Medication Adherence for Cholesterol - Statins 100% (n = 38), Diabetes Care - Eye Exam 100% (n = 29), Diabetes Care - Blood Sugar Controlled 88% (n = 14), Diabetes Care - Kidney Disease Monitoring 76% (n = 25), Annual Flu Vaccine 74% (n = 14), and Statin Use in Persons with Diabetes 53% (n = 10) (Figure 2). These findings suggest that pharmacist intervention can help improve quality measures and potentially lead to an overall increase in Star Ratings. As the role of a pharmacist continues to expand nationwide, this program has the potential to develop into a permanent service line within the family medicine clinic.
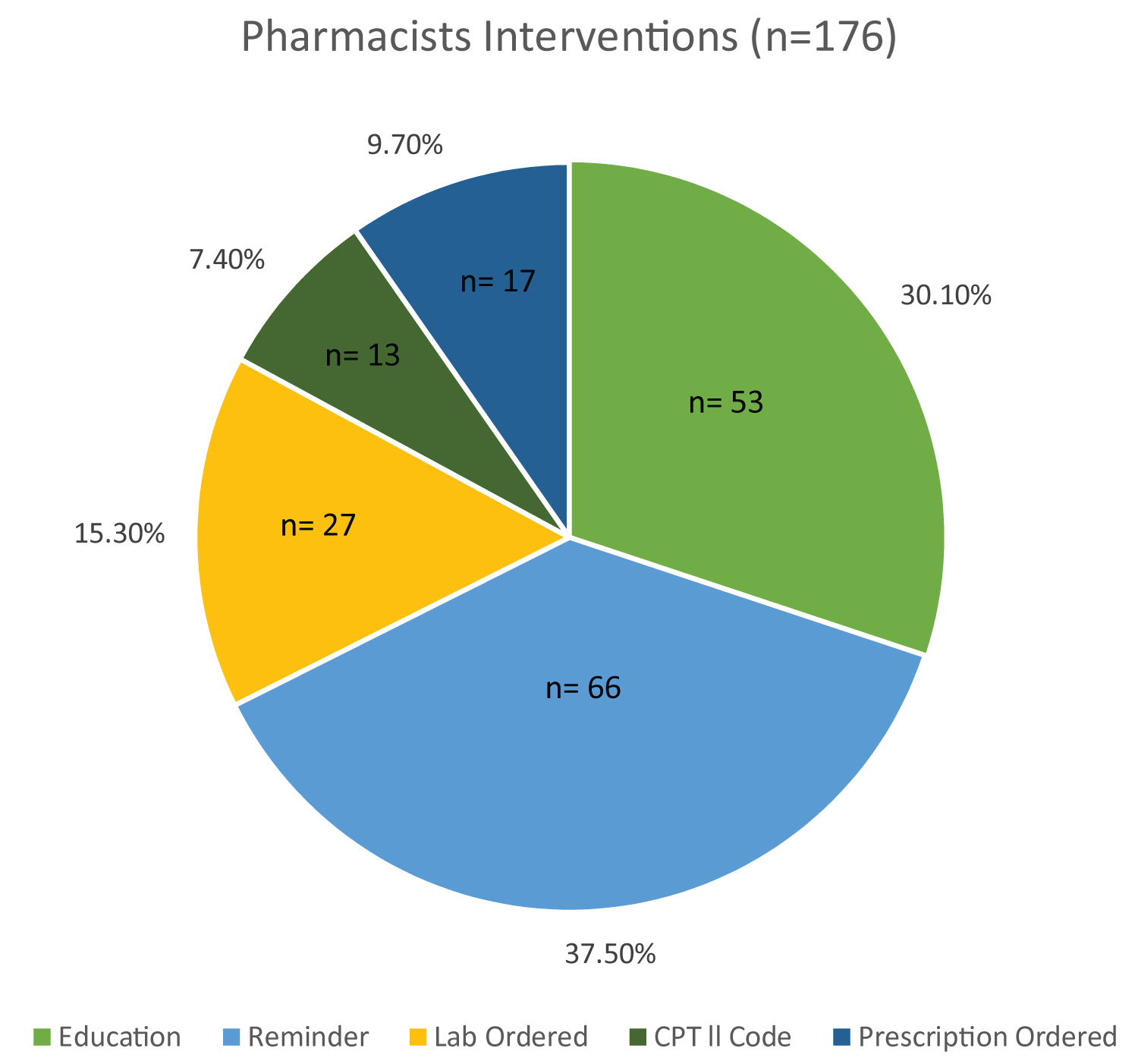 Figure 1: Pharmacist Interventions. This figure depicts the various types of pharmacist interventions. CPT indicates Current Procedural Terminology. CPT ll Codes are supplementary tracking codes that can be used to satisfy quality measures.
View Figure 1
Figure 1: Pharmacist Interventions. This figure depicts the various types of pharmacist interventions. CPT indicates Current Procedural Terminology. CPT ll Codes are supplementary tracking codes that can be used to satisfy quality measures.
View Figure 1
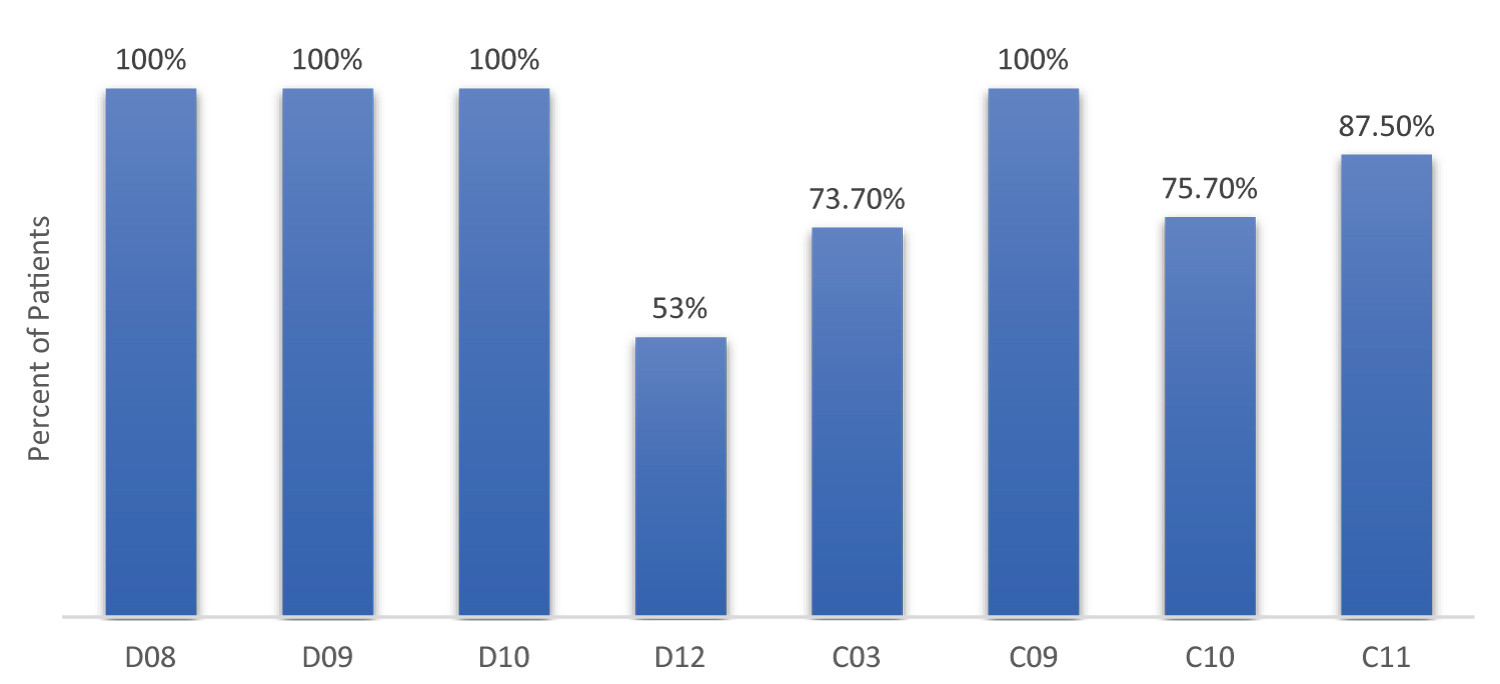 Figure 2: Quality Measures Satisfied. This figure depicts the percent of patients who satisfied the following CMS Part C and D quality measures after pharmacist intervention: D08: Medication Adherence for Diabetes Medications, D09: Medication Adherence for Hypertension (RAS antagonists), D10: Medication Adherence for Cholesterol (Statins), D12: Statin Use in Persons with Diabetes (SUPD), C03: Annual Flu Vaccine, C09: Diabetes Care - Eye Exam, C10: Diabetes Care - Kidney Disease Monitoring, and C11: Diabetes Care - Blood Sugar Controlled.
View Figure 2
Figure 2: Quality Measures Satisfied. This figure depicts the percent of patients who satisfied the following CMS Part C and D quality measures after pharmacist intervention: D08: Medication Adherence for Diabetes Medications, D09: Medication Adherence for Hypertension (RAS antagonists), D10: Medication Adherence for Cholesterol (Statins), D12: Statin Use in Persons with Diabetes (SUPD), C03: Annual Flu Vaccine, C09: Diabetes Care - Eye Exam, C10: Diabetes Care - Kidney Disease Monitoring, and C11: Diabetes Care - Blood Sugar Controlled.
View Figure 2
Quality healthcare is a high priority for CMS. With physician shortages on the rise, pharmacist involvement will be vital in continuing the progression towards value-based care. By utilizing a value-based care model, pharmacists in a hospital-based ambulatory care setting created the potential to have an impact on the CMS overall Star Rating for the healthcare plan, ultimately paving the way for incentive bonuses, reduced co-payments, expanded coverage, and increased patient enrollment. With an expertise in medications and chronic disease state management, pharmacists are in a key position to educate patients about their medications and develop patient-specific care plans for chronic disease states, and in turn, reduce potential healthcare expenditures due to inappropriate use of a medication or complications from an uncontrolled disease state.
The data underlying this article are available in the article.
This manuscript has not been presented at a conference or published elsewhere.
The authors have no relevant conflicts of interest to disclose.
This work was not supported by any funding source.