We present the case of a young female who presented with a giant infratentorial and supratentorial epidermoid cyst. Due to the size of the cyst, the decision was made to stage the surgical resection across two operations rather than undertake a single radical surgical approach. This presented the dilemma of timing for the second stage given the risk of aseptic meningitis occurring with an incompletely resect epidermoid cyst, making the second surgery more challenging due to scarring. The patient presented 15 days following the first operation with aseptic meningitis, which was managed medically. They underwent surgical resection of the residual epidermoid cyst 4 weeks following the first operation. The aim of this case report is to review the challenges with giant epidermoid cysts and how to balance the risks and benefits of different management strategies.
We present the case of a female in their late 20’s who presented with a chief complain of 12 months of right sided tinnitus that was worsening. These symptoms had been present for years prior but had not been bothersome to the patient. Neuroimaging demonstrated a giant infratentorial and supratentorial epidermoid cyst.
Aseptic meningitis secondary to rupture of an epidermoid cyst into the cerebrospinal fluid (CSF) spaces is a rare, but previously documented event [1]. Aseptic meningitis following posterior fossa surgery is not an uncommon complication, however it appears to occur more frequently in patients having epidermoid cysts resected [2].
Epidermoid cysts are rare, accounting for 0.2-1.8% of all intracranial tumours [3]. Of these tumours, only a very small number are giant in size with a recent review identified only 12 cases in the literature [3].
Our case involved a giant intracranial epidermoid cyst that differed from what has been previously reported because it could not be easily resected through a single craniotomy. The management option selected was to perform staged surgeries separated by a period of weeks. The challenge we experienced was how to balance the increased surgical risk of subjecting the patient to two craniotomies compared to the risk of developing post-operative aseptic meningitis from subtotally resected epidermoid cyst between treatment stages, which would make achieving gross total resection more challenging.
We present this case to supplement the existing literature and improve decision making for these complex cases.
The patient was a female in their late 20's who presented following neuroimaging organised by their family doctor to investigate right sided tinnitus that had been progressively worsening for the past 12 months. In addition, the patient also had numbness and tingling of their right cheek and headaches. The patient did not have any significant medical background and had no relevant family history.
On examination the patient had a mild right sided numbness in V2 and V3, with all other cranial nerves being intact. Limb and gait examination was completely normal.
The MRI head demonstrated a large extra-axial lesion that was T2 bright with diffusion restriction. The lesion extended from the jugular foramen up to the interpeduncular fossa and laterally towards the right middle cranial fossa, demonstrated in Video 1.
Video 1: Pre-operative MRI.
Indications for treatment were considered based on: the patients young age, the size of the tumour and the likely tumour histology.
The goal of surgery was to decompress the brainstem, confirm the histological diagnosis and decompress and preserve the critical neurovascular structures. If the entire capsule could be removed safely that would be a secondary goal, but it would not be pursued at the expense of neurological morbidity.
There were three potential management strategies that were considered.
1. Observation was dismissed immediately due to the size of the tumour and the patients age. Avoiding further symptomatic progression due to tumour growth was extremely unlikely.
2. A single operation either through two separate craniotomies, or an extensive skull base approach like a combined petrosal approach to remove the tumour in one operation. This was not felt to be best for a few reasons. There was no surgical benefit from removing a portion of the petrous bone, unlike a meningioma where devascularisation can greatly improve the safety of surgery. The minimal symptoms the patient was experiencing did not justify such a radical approach. However, it would potentially give a slightly higher chance for complete resection.
3. A staged surgery through two approaches separated by four to six weeks. This was the management strategy of choice because it allowed the optimal operative corridors to safely remove as much tumour as possible, while allowing preservation of neurovascular structures. It allowed the patient to completely recover between operations and would therefore reduce the rate of complications. Post-operative aseptic meningitis was considered, but it was felt that a weaning course of steroids post-operatively would mitigate this risk.
Operation one involved a right sided retrosigmoid craniotomy which was undertaken with neuronavigation and facial nerve monitoring. During this operation the tumour was dissected from the upper, middle and lower neurovascular complexes. The tumour was dissected from both sides of the basilar artery and maximal safe removal of the tumour in the interpeduncular cistern was achieved. Residual was left in this area and in the middle cranial fossa. Reconstruction was completed with a watertight dural closure and copious Ringer’s lavage, refer to Figure 1 and Figure 2. The patient was discharged home with a weaning dose of steroids over 7 days from the date of their operation.
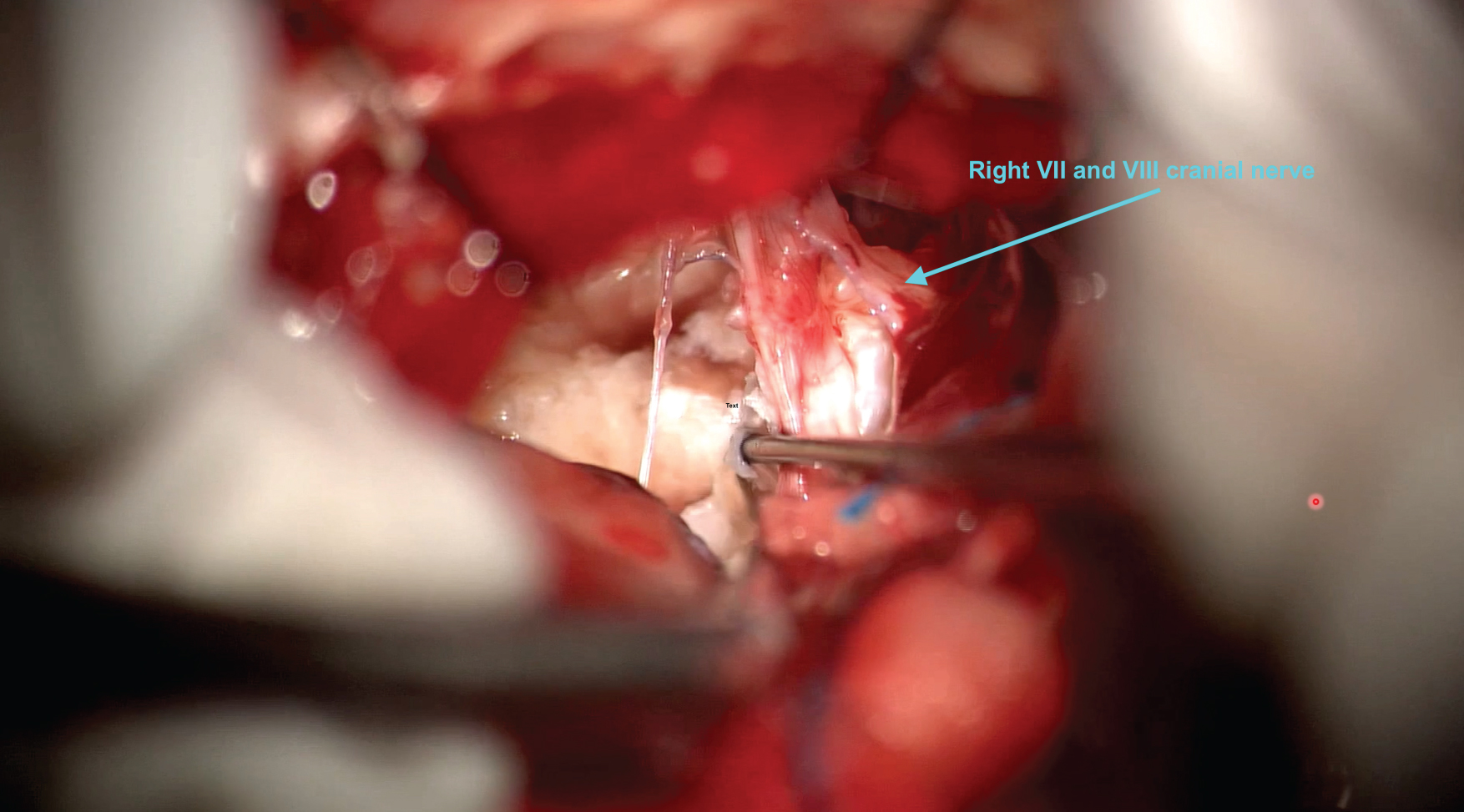 Figure 1: Photograph during the resection phase of the first operation. The view is through a right sided retrosgimoid craniotomy focusing on the middle neurovascular complex of the cerebellopontine angle cistern demonstrating the dissection of the epidermoid tumour off the VIIth and VIIIth nerves.
View Figure 1
Figure 1: Photograph during the resection phase of the first operation. The view is through a right sided retrosgimoid craniotomy focusing on the middle neurovascular complex of the cerebellopontine angle cistern demonstrating the dissection of the epidermoid tumour off the VIIth and VIIIth nerves.
View Figure 1
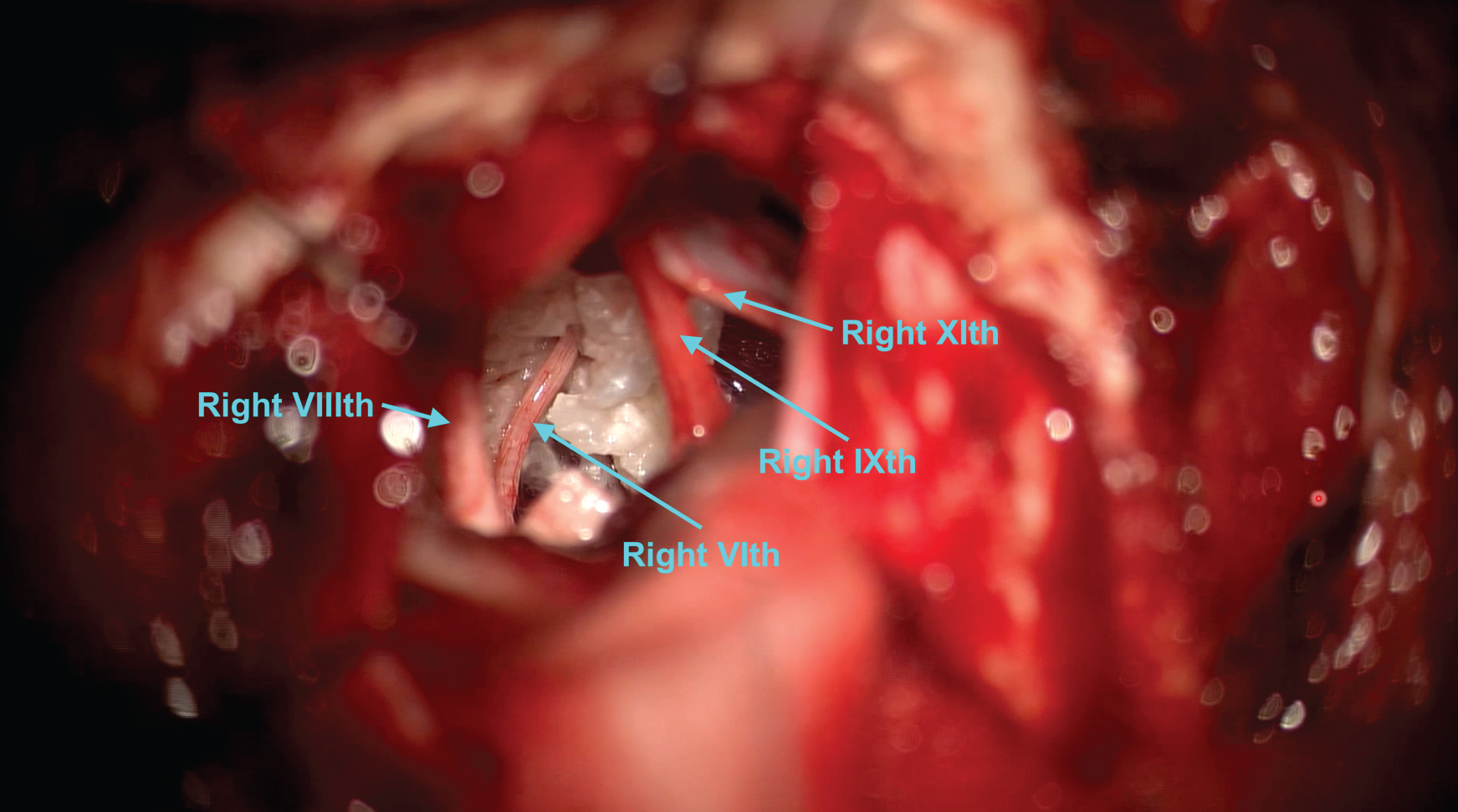 Figure 2: Photograph during the resection phase of the first operation. The view is through a right sided retrosgimoid craniotomy focusing on the lower neurovascular complex of the cerebellopontine angle cistern. The VIth, IXth and XIth cranial nerves can be seen.
View Figure 2
Figure 2: Photograph during the resection phase of the first operation. The view is through a right sided retrosgimoid craniotomy focusing on the lower neurovascular complex of the cerebellopontine angle cistern. The VIth, IXth and XIth cranial nerves can be seen.
View Figure 2
Operation two involved a right frontotemporal craniotomy with a transsylvian and pretemporal approach to the residual tumour with a watertight reconstruction, refer to Figure 3.
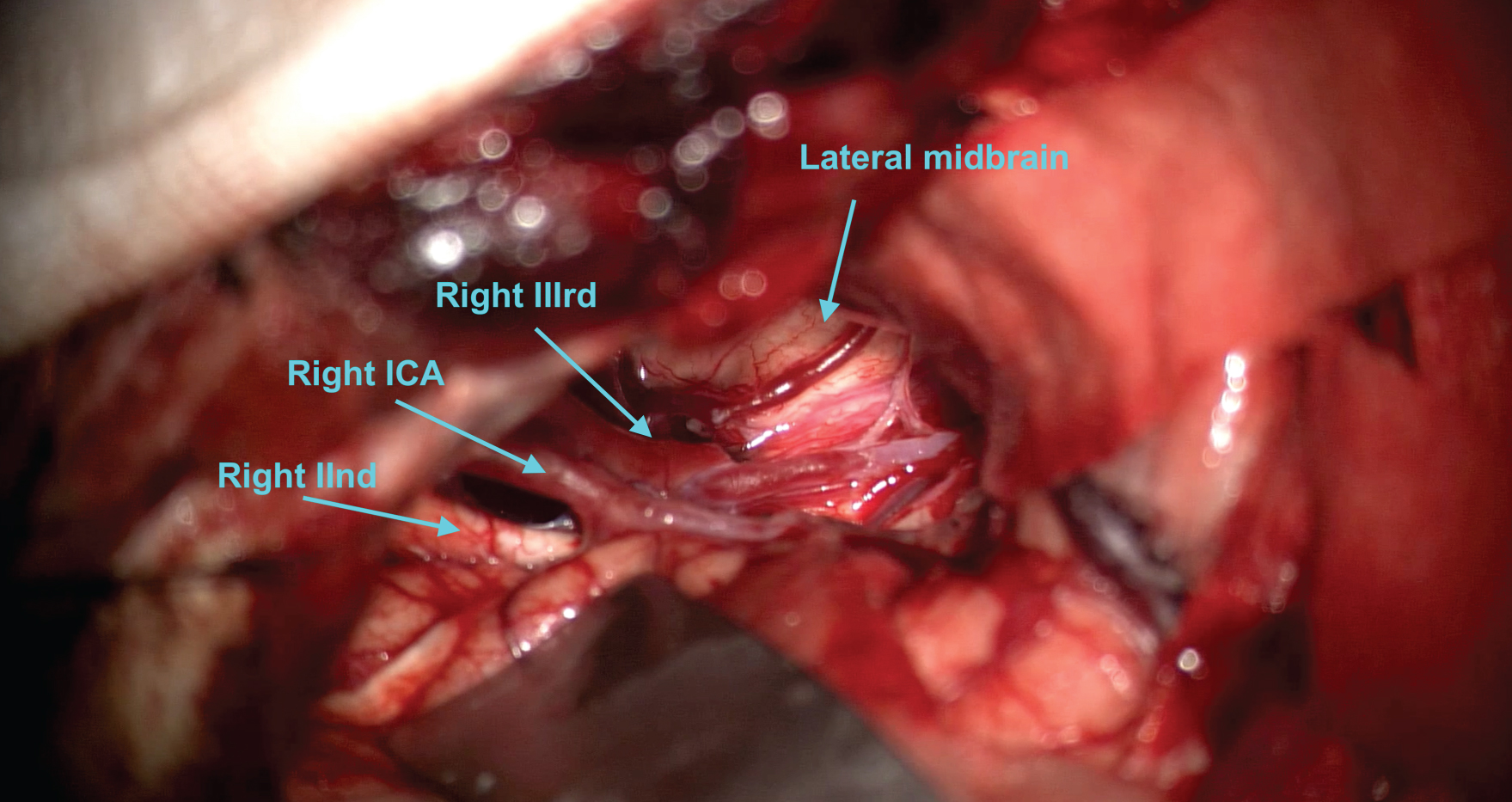 Figure 3: Photograph at the conclusion of the resection in the second operation. The view is through a right sided front osphenotemporal craniotomy with pretemporal approach. The lateral surface of the midbrain is decompressed and the right IIIrd nerve and optic nerve are visualised.
View Figure 3
Figure 3: Photograph at the conclusion of the resection in the second operation. The view is through a right sided front osphenotemporal craniotomy with pretemporal approach. The lateral surface of the midbrain is decompressed and the right IIIrd nerve and optic nerve are visualised.
View Figure 3
On day 16 following the first operation the patient returned to hospital with a headache and a CSF leak through her wound. A lumbar puncture demonstrated clear CSF with an opening pressure of 34 cm H2O, 1 mononuclear cell and 1 polymorphonuclear cell and no bacteria. The patient was recommenced on steroids with a weaning plan over 2 weeks.
On day 8 following the second operation the patient returned with shortness of breath and tachycardia after collapsing at home. A subsequent CT pulmonary angiogram demonstrating a large pulmonary embolus. She was monitored in the intensive care unit for one night as she had developed hypotension. Decision was made to commence a heparin infusion initially given the recent surgery, which was transitioned to an oral anticoagulant after 48 hours.
The patient was reviewed at 6 weeks, 3 months and 12 months post-operatively. Their tinnitus improved but did not completely resolve. A mild right sided facial nerve and oculomotor nerve palsy present after the surgeries had completely resolved by 12 months. The patient has subsequently returned to work full time. A post-operative MRI scan at 3 months demonstrates no residual tumour, but she will be under surveillance for at least 10 years, refer to Video 2.
Video 2: Post-operative MRI.
Epidermoid tumours are due to incomplete cleavage of neural from cutaneous ectoderm during development. This results in inclusion of epiblasts in the neural groove at the time of closure [1]. The epidermoid tumour enlarges through desquamation of epithelial cells. This cellular debris then breaks down as keratin and cholesterol within the tumour capsule, as such they tend to follow a slow linear growth pattern.
A definition for what constitutes a giant intracranial epidermoid tumour does not appear to exist. A review by Spinato, et al. in 2021 reviewed giant epidermoid cysts of the posterior fossa, but do not define a minimum size requirement [3]. They report on a 8.4 cm tumour arising from the cerebellopontine angle and posterior petrous bone where it extends extracranially to the skin of the scalp. The maximal dimension of the tumour we report is 5.6 cm, but this is difficult to measure given the extension that goes perpendicularly across the middle fossa floor from the interpeduncular fossa.
There appears to be one contemporary series of giant intracranial epidermoid tumours published by Al-Mefty, et al. in 2015 [4]. The article reports excellent long-term results for patients with complete resection of the epidermoid tumour and the capsule. They do not have a clear definition for what constitutes a giant epidermoid tumour. The main focus of the article was regarding the significantly greater chance of cure being achieved on the index operation compared to when the patient presents with a recurrence. It was for this reason they employed a combined petrosal approach for 8 of the 38 cases, however the anatomical considerations of these tumours are not discussed. In addition, they do not go into granular detail regarding specific complications such as aseptic or Mollaret’s meningitis.
The rate of post-operative aseptic meningitis can be as high as 50% in patients having epidermoid tumours removed [5]. This episode of inflammation can increase scarring and make further surgery more challenging. In our case the second stage of the operation was more challenging with some areas of the tumour requiring subpial dissection. It’s not known whether this was the nature of the tumour, or it was caused by the episode of aseptic meningitis. Al-Mefty, et al. [4] discuss the challenge giant tumours present when trying to achieve gross total resection, and thus advocate for full exposure through a skull base exposure.
Our patients post-operative course was complicated by a pulmonary embolus, a well-known complication from major surgery. This was the type of complication we had hoped to avoid by staging the management of the patient between two short surgeries. During the episode of aseptic meningitis after the first operation the patient had significantly reduce mobility due to headache. It is possible that this increased their risk of a pulmonary embolus, especially when combined with the second surgery. However, this is entirely speculative. Interestingly the article by Al-Mefty [4] reported using a post-operative weaning steroid regimen lasting 14 days. It is unknown if an extra 7 days of steroid weaning in our patient would have avoided their episode of aseptic meningitis.
Overall, in our attempts to avoid a complication from a prolonged surgery this still occurred. Despite this, the patient has done well, and we believe a complete resection of the tumour and capsule was achieved. Upon reflection, it would be reasonable to consider a longer period of steroid weaning to potentially reduce the risk of aseptic meningitis or consider a more radical surgical strategy so that the tumour could be removed in a single operation.
• Gross total resection at the index operation is the best chance to achieve cure in epidermoid tumours.
• Prolonged post-operative steroids may be reasonable to consider, particularly in a case of staged surgery.
• It would be reasonable to consider a more radical surgical strategy to ensure complete resection can be achieved in a single operation, if can be done safely.
I was in continuous pain daily, I also found that I had faster than normal hair growth on my head, with hair strands falling out constantly, if I brushed, it would be close to a handful of hair pulled from cleaning my brush, my eyes occasionally twitched/moved to the side rapidly out of the blue, I was exhausted all the time and didn’t have the energy to do daily tasks some days and my body needed to “shut down” so I had to have naps, no matter how hard I tried not to. My headaches were progressively worsening, with daily headaches and migraines (where two were so bad, I was required to stay in a dark room and vomited if I sat up), neck, back, and jaw pain, with some facial sensitivity. There was little relief with specialist appointments to try and manage the pain. I began experiencing worsening tinnitus which finally got me a referral to a specialist, who then granted an MRI with contrast to investigate.
42 days after my first MRI with contrast, I received word that it was a large epidermoid tumour on/around my brain stem causing issues with my ears and little did I know, it was causing other symptoms as well (which I didn’t realize at the time) and it will require surgery. I honestly was shocked that it was a tumour of all things, the positioning and location of it concerned me as it came with a list of complications when signing the paperwork, one being death.
I had my first operation in June 2021, with the first one being behind my right ear, the incision being the shape of a crescent moon. It wasn’t very painful after surgery, but I am aware, some pretty strong medications assisted with reducing pain. As this was mainly a debulking surgery, I did still have headaches, but they weren’t as bad as they had been. I had light sensitivities after waking up from surgery, as well as double vision, so wore an eye patch as soon as one was available. I did feel weaker than normal, so had to take things slow as I feel my balance was off. While at home, there were two occasions I had shortness of breath and had to sit down and take some slow deep breaths.
16 days after my first surgery, I presented to the ER with a small leak from my incision. This required me to have multiple attempts at a lumbar puncture in the ER that were unsuccessful, then a guided CT lumbar puncture the next day, which included swabs/cultures to rule out any infections that could escalate the situation. Thankfully, the CSF showed no infections, and I was allowed to go home a couple of days later, as we needed to wait for the “negative” results, so I could continue to recover comfortably at home.
28 days after my first procedure, I was in for my final surgery to get the remainder of my tumour. This time, it was the larger incision, starting from the left side of my forehead, just above my hairline, going across and down to my right ear. With the recovery starting from this second surgery, I still experienced light sensitivities and double vision, still felt weaker, and was also a bit more emotional. I wore eye patches constantly, to assist with daily tasks and walking around.
Unfortunately, 8 days after this surgery, I collapsed at home and required attendance to the emergency room via ambulance. I didn’t completely know what was going on at the time, I remember a loud ringing in my ear, then slowly lowering myself down onto the floor. There is a possibility of me passing out for a split moment. After coming out the other side and talking with others about it, I found out, that I nearly died that day from saddle pulmonary embolisms.
After the correct dosage of blood thinning medication was given, as my surgeries had to be factored in, to prevent brain bleeds, it became a balancing act with my blood. I was in ICU classified as critical for a day and in ICU for another 3 days for observations. I was on blood thinning injections when I went home, those continued for a week, then I continued with blood thinning tablets for a couple of months, until the clots were confirmed to have dispersed.
After being informed about blood clots and the symptoms they can present with, I can see I missed a sign, within those 8 days after my second surgery, when I was stretching, I felt a slight pain in my right calf muscle, I didn’t think anything of it then, as I just woke up. The pain was for only a minute and then it was gone. I now know to point my toes when stretching, and if I get that sharp “pull” feeling in my calf like I did during recovery, to question it.
Once I was home, the light sensitivities lessened over time, and a couple of months later I was able to be without an eye patch. I followed up with specialists to get my double vision under control, as a result, I was able to purchase prism glasses 21 days after my second surgery, which removed the double vision and made it easier for me to navigate around unassisted and read with both eyes.
4 months after my second surgery, I received confirmation that there was no evidence of my epidermoid tumour.
Once I was cleared by my numerous specialists, I was able to get back to driving.
4 and a half months after my second surgery, I was off my blood thinners and I was back at work, with reduced duties to start with, but back to normal functioning duties after a week to ensure no complications arise during my shift.
I have been living without continuous pain, since recovering from this surgery. It has been a learning experience, one I will never forget, and I can’t believe how much this tumour affected my life physically and mentally.
I can say, having it removed, has bettered my quality of life, I feel this approach is effective, under my circumstances, even though I did encounter some serious complications along the way.