Introduction: Hackethal-type fasciculated pinning is a closed-focus osteosynthesis technique for humeral shaft fractures. Our aim was to evaluate the anatomical and functional results.
Methodology: This was a descriptive cross-sectional study covering a 54-month period from January 2019 to June 2023 in the Department of Orthopaedic and Traumatological Surgery. All patients aged 18 or over who underwent surgery and were followed up at SCOT during the study period and had a usable clinical record were included. The AO and Gustillo/Anderson (G/A) classifications were used to classify lesions. Results were assessed using the STEWARD AND HUNDLEY score.
Results: Frequency was 1.15%. Mean age was 31.55 (18 and 68 years). Men accounted for 90% (n = 18), women 10% (n = 2), with a sex ratio of 9 in favor of men. The average consultation time was 6.2 days. Road traffic accidents predominated, accounting for 55% (n = 11). The majority of patients were right-sided, 85% (n = 17), while the left side was affected in 60% (n = 12). There were five cases of cutaneous opening, and AO type 12A3 invoices were frequent in 65% (n = 13). The approach was supraolecranial in 19 (95%). Bone consolidation was achieved in 19 cases (95%). The mean time to consolidation was 11 weeks. Functional and anatomical results were excellent in 80% of cases.
Conclusion: Hackethal skewering remains an easy and rapid technique, but requires perfect mastery of the procedure.
Hackethal pinning humerus N'Djamena
Fractures of the humeral shaft are all solutions of continuity occurring in a region bounded superiorly by the inferior edge of the insertion of the pectoralis major muscle and inferiorly by the inferior edge of the insertion of the brachialis anterior muscle [1]. They are not uncommon, ranking 4th behind leg fractures [2]. They account for 5% of all fractures [3]. Their frequency is increasing due to the growing number of public road accidents [4]. Diagnosis of these fractures is straightforward, based on the clinical X-ray findings. On the other hand, there is far from unanimous agreement on treatment modalities [5]. There are advocates of orthopedic treatment and those of surgical treatment. Hackethal-type fasciculated pinning is a closed-focus osteosynthesis technique, and appears to be an intermediate solution between orthopedic methods and plate or nail osteosynthesis. The aim of our work was to analyze the anatomical and functional results of this technique in order to deduce its advantages and limitations.
We conducted a descriptive cross-sectional study over a 54-month period from January 2019 to June 2023 at the Orthopedic and Trauma Surgery Department (SCOT) of the Renaissance University Hospital. All patients aged 18 or over who underwent surgery and were followed up at SCOT during the study period and had a usable clinical record were included. Patients treated by other surgical procedures and orthopedically, as well as those with incomplete clinical records, were excluded from our study. The AO classification was used for bone lesions and the Gustillo/Anderson (G/A) classification for skin opening. All patients were positioned supine on a standard table under general anaesthesia, with the fractured limb placed on a radiolucent table. Reduction was performed by external maneuvering under the control of a mobile image intensifier, parallel to the operating table. The supra-olecranial approach through an oval hole was used to insert Metaizeau wires of various sizes (Figure 1). The pins were inserted into the fracture site and diverged in the humeral head under image intensifier control (Figure 2), and an immediate control radiograph was taken (Figure 3). Epidemiological, radio-clinical, therapeutic and evolutionary variables were studied on the basis of a data sheet and patient summons. Anatomical and functional results were assessed using the STEWARD AND HUNDLEY score.
 Figure 1: Different sizes of Métaizeau wire and materials for installation.
View Figure 1
Figure 1: Different sizes of Métaizeau wire and materials for installation.
View Figure 1
 Figure 2: (a) Left humeral shaft fracture; (b) Wire insertion.
View Figure 2
Figure 2: (a) Left humeral shaft fracture; (b) Wire insertion.
View Figure 2
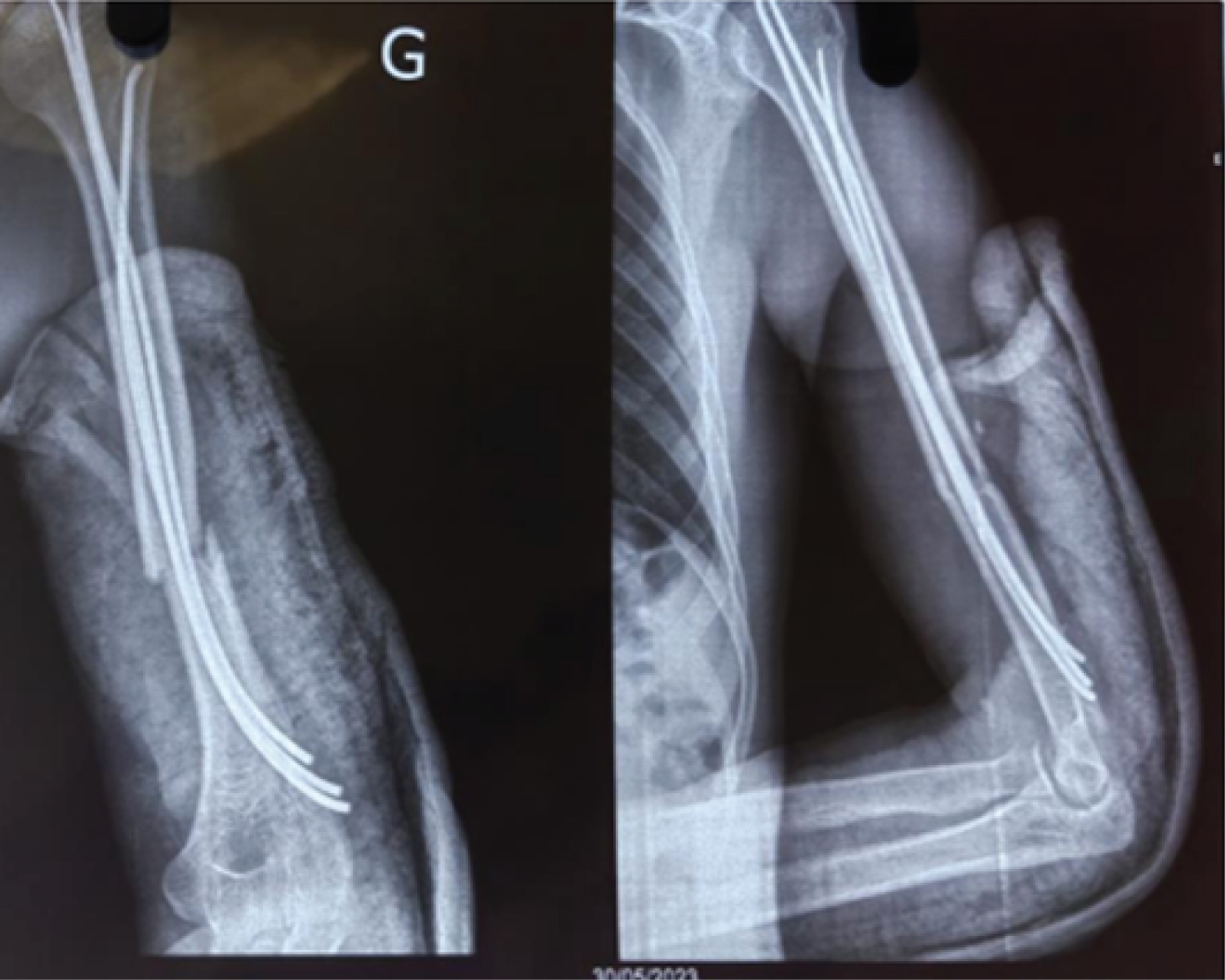 Figure 3: Control X-ray (a) front (b) profile.
View Figure 3
Figure 3: Control X-ray (a) front (b) profile.
View Figure 3
We recorded 1,729 cases of compound fractures in the Department of Orthopaedic Surgery and Traumatology (SCOT) at CHU-R, including 20 cases of diaphyseal humeral fractures meeting the inclusion criteria, representing a frequency of 1.15%. The mean age was 31.55, with extremes of 18 and 68 years. Males accounted for 90% (n = 18), females 10% (n = 2), with a sex ratio of 9 in favor of males. School children/students were the most affected in 40% (n = 8), followed by military personnel in 30% (n = 6). Three patients (15%) were referred to traditional practitioners.
The average consultation time was 6.2 days, with extremes ranging from one hour to 16 days. The circumstances of onset were dominated by road traffic accidents 55% (n = 11), followed by firearm injuries 25% (n = 5) and falls 20% (n = 4). The majority of patients were right-sided, i.e. 85% (n = 17), while the left side was affected in 60% (n = 12). There were no cases of bilateral fractures. Five cases of skin opening, three of which were G/A type I and two type II. Inclusions classified as AO type 12A3 were frequent in 65% (n = 13), and one case of bifocal fracture following ballistic trauma. In 7 cases (35%), the fracture was part of a polytrauma.
The mean time from trauma to surgery was 5 days, with extremes of 10 hours and 16 days. General anaesthesia was used in 18 patients (90%), versus 10% with plexus block. The approach was supraolecranial in 19 (95%). Only one patient with radial nerve damage underwent neurolysis. The number of pins used varied between 2 and 4, depending on the diameter of the medullary canal. Average hospital stay was 5 days, with extremes ranging from 2 to 21 days.
Bone consolidation was achieved in 19 cases (95%). Mean time to consolidation was 11 weeks. Mean time to removal of osteosynthesis material (AMOS) was 7 months, with extremes of 2 months and 13 months. Five patients developed complications (Table 1).
Table 1: Distribution of complication types. View Table 1
When evaluating our results, we noted 80% of very good and good results (n = 16); 15% of fairly good results (n = 3); 5% of bad results (n = 1). The latter was a case of vicious callus (Table 2).
Table 2: Assessment using the Modified Stewart & H score. View Table 2
Humeral shaft fractures are relatively common in our practice. The epidemiology of our work is unremarkable. It shows a clear predominance of young men following road traffic accidents. It also shows that medio-diaphyseal fractures are more frequent, as reported in the literature [6]. On the other hand, left-sided involvement predominates in our series, a result which is superimposed on that of Haider, et al. [7] in Iraq. On the other hand, Abiome, et al. [8] in Gabon and Moykoua, et al. [9] in India note a predominance of right-sided involvement. This could be explained by the high number of right-handers in our population, who tend to protect their dominant side, which is the right side. With regard to skin lesions, the fracture was open in 25%, i.e. 5 cases. This result is superior to those of Dayez, et al. [10] in France and Bouyarmane, et al. [11] in Morocco, who found 5.5% and 12.5% open skin respectively. The small size of our sample and ballistic trauma, the second most common etiology in our series, explain this frequency. Humeral diaphyseal fractures pose a real therapeutic problem, with several complications. Fasciculated hackethal pinning remains a reliable technique, with a lower risk of both infectious and neurological complications. We have only recorded one case of post-fracture radial nerve damage, which required an approach to the site and neurolysis. Omar, et al. [6] noted a rate of 8.57% of post-traumatic radial paralysis, which is comparable to the average in the literature: 7.73% for Putz, [12] and 10% for Coudane, [13]. Systematic exploration in cases of radial nerve damage has been reported by several authors [14,15], as in our series. Post-osteosynthesis radial paralysis using screw plates varies from 6.5% to 12% in the literature [3]. In the case of anterograde centromedullary nailing, Blum, et al. [16] reported a rate of 4%, with a non-negligible rate of abduction limitation due to rotator cuff damage. Schvingt, et al. [17] reported a 19% rate of abduction limitation beyond 20 degrees. In our series, no radial paralysis secondary to osteosynthesis was noted; however, the main complications encountered were elbow stiffness and one case of pseudarthrosis. These complications have been reported by several authors [18-20]. Secondary immobilization in our series could explain the frequency of elbow stiffness, and also the association with other lesions forming part of the polytrauma picture. The lack of impaction at the fracture site explains the occurrence of pseudarthrosis. The biomechanical problems encountered in most studies of fasciculated pinning are secondary to defective fixtures with reduced mechanical properties. This can be seen, on the one hand, in the failure to fill the medullary canal and, on the other hand, in the pins being too short and not bearing in the metaphyseal cancellous zone. Pin migration, encountered in 7% of cases in the study by Gayet, et al. [18], was not recorded in our series. The mean time to consolidation was 11 weeks, close to those reported by Ouahidi, et al. [21], and Mardar, et al. [6], who found 9.6 and 10 weeks respectively. In the study by Pidhorz, et al. [3] of recent and old humeral shaft fractures, the time to consolidation after screw-plate osteosynthesis ranged from 11 to 19 weeks. For anterograde nailing, the team of Ingman, et al. [22] reported a consolidation time of 12.6 weeks. Functional and anatomical results were very good, and good in 80% of our series. This very satisfactory result could be explained by the mastery of the surgical technique and the reduced time required for management.
Hachethal-type fasciculated pinning appears to be a genuine intermediate solution between orthopedic and surgical methods using plates or nails. It is quick and easy to perform, but requires mastery of the closed-focus technique. This procedure avoids intraoperative damage to the radial nerve and rotator cuff, and reduces the risk of infection. The accessibility and lower cost of metaizeau wires are major advantages in the therapeutic arsenal.
We declare no conflicts.
All data are included in the content of the article.
We have received no funding for this research.
This study complies with the Helsinki ethical principles for medical research involving human subjects. We have obtained the informed consent of all our patients and the authorization of the competent institutional body, which is the medical management of our Centre Hospitalier Universitaire la renaissance.