Diabetes mellitus is the most common cause of Charcot's Neuroarthropathy (CN). It is a devastating complication of longstanding uncontrolled hyperglycemia. When present, it leads to cascades of interrelated and compounding pathophysiological abnormalities resulting in distal peripheral neuropathy, vasculopathy, inflammation, and arthropathy. If diagnosed early, it responds to conservative medical management with diabetes control, non-weight bearing (offloading), and immobilization; and the foot can regain near normal function. But when discovered late, it leads to advanced arthropathy requiring various complex procedures to correct deformity, and reconstructive surgeries to prevent progressive destruction of the foot and the ankle joints. In the process, these lead to not only significant disability and recurrent hospitalizations but are associated with major complications - soft tissue injury, infection, osteomyelitis, bony fracture, joint dislocation, deformity, ulceration, amputation, and even death.
Diabetes prevalence is on the rise across the world. In the US, it affects 10.7% of the population of 20-79 years, that is 32.2 million people; and in the world, it affects 9.8% of the population, that is 536.6 million in 2021. ( www.diabetesatlas.org/IDF ) [1]. Diabetes is the most common cause of Charcot’s Foot neuroarthropathy in the western world. Its incidence in diabetics ranges from 0.1% to 0.4%, but this increases to 35% in patients with peripheral neuropathy [2,3].
Diabetics with Charcot’s neuroarthropathy are usually in their 50s to 60s, and most have had diabetes for at least 10 years [4]. The most affected joints are in the foot and ankle, although other sites are reported to have been affected including knee, wrist, and spine [2].
Current evidence supports that diabetic peripheral neuropathy, associated with diabetes and its related metabolic abnormalities, predisposes to the development of Charcot’s neuroarthropathy. The neuropathic condition affecting the sensory, motor, and autonomic nerves enhances the local inflammatory response triggered by minor trauma, compounded with vascular dysregulation, soft tissue injury, and bony structural deformities. If not effectively treated early, these lead to progressive destruction of the foot, ankle joints, causing skin ulceration, infection, osteomyelitis, deformity, and limb amputation.
Early stage of DCN, includes unilateral warm, edematous, sometimes painful foot and/or ankle. At this stage it is easily confused with cellulitis, deep vein thrombophlebitis, or acute gout. As a result, appropriate diagnosis and treatment are delayed, leading to advanced arthropathy. This manifests as stable or unstable bony deformities, subluxations, or dislocations in multiple joints of the foot and/or ankle.
Secondly, in the early stage of DCN, the laboratory results are equivocal and plain film radiograph may not show abnormalities. So, in a diabetic individual with evidence of peripheral neuropathy with the above presentation, a high index of suspicion is necessary to reach a definite diagnosis. This can be confirmed by an MRI scan [5], the modality of choice, in detecting bony microfractures and evidence of bone marrow edema. In advanced stages, PET/CT scan has shown promising results, especially when complicated with osteomyelitis [5].
Here is a case presented with early onset of DCN but was treated as cellulitis, leading to advanced arthropathy. This resulted in prolonged medical and surgical interventions to rescue the foot and ankle joints, restoring to some degree of functionality, and in avoiding amputation.
CL is a 54-year-old male was found to have adult-onset diabetes on 10/1/2007 with non-fasting blood glucose of 284 mg/dl and, HbA1c of 7.8%. Additional laboratory evaluations revealed total cholesterol of 204 mg/dl, triglyceride of 163 mg/dl, HDL cholesterol of 44 mg/dl, and LDL cholesterol of 127 mg/dl. But he did not seek medical care until he came to see his PCP on 8/17/2010.
During this office visit, he complained of symptoms of polydipsia and numbness in both feet, right greater than the left. In addition, he had complained of shortness of breath. The pertinent history included a history of light smoking which he had quit in 1975, and he had used alcohol occasionally. He is tall in stature with a height of 6 feet and 4 inches and weighed 117.5 kg (BMI 31.54). Physical examination revealed elevated blood pressure, eye examination revealed arteriolar narrowing, neurologic evaluation confirmed sensory deficit in the feet, and he had footdrop in the right, and foot weakness in the right greater than the left. Bilateral lower extremity peripheral pulses were 2+. The laboratory evaluations revealed markedly elevated blood glucose of 314 mg/dl, HbA1c 8.4%, total cholesterol of 222 mg/dl, triglyceride of 108 mg/dl, HDL cholesterol of 43 mg/dl, and LDL cholesterol of 157 mg/dl, NT-Pro BNP 312 PG/ml (normal < 125 PG/ml). He was diagnosed to have diabetes, hypertension, hyperlipidemia, peripheral neuropathy, and congestive heart failure (CHF). He was treated with Glyset 25 mg po tid, lisinopril 10 mg po daily, zocor 20 mg po daily, Neurontin 100 mg po tid, and Lasix 40 mg po daily.
He was referred to a cardiologist for evaluation of newly diagnosed CHF. An echocardiogram revealed left ventricular ejection fraction (EF) of 35%. Cardiac catheterization revealed normal right heart pressures, and patent coronary arteries. The medical management was optimized with the addition of carvedilol 25 mg po BID and Aldactone 25 mg po daily. Later, Victoza 0.2 ml (1.2 mg) was added to Glyset to improve diabetes control. During acute illness from sepsis, Glyset was replaced with insulin.
On 1/18/2013, he presented to the Emergency Room (ER) due to swelling in the right leg starting around 12/25/2012 associated with pain. Examination revealed leg edema in the right foot extending up to knee, the skin was warm, and slightly erythematous. There was no tenderness and no crepitation. The HR was 78/minute, BP 157/88 mm of Hg, O 2 saturation 97%, temperature 98.2 F. Blood chemistry and hematological analysis revealed elevated blood glucose of 352 mg/dl, WBC 7.7 k (4.5-10.5 k/mm 3 ), segmented neutrophil count of 65% (40-75%), lymphocytes 26% (27-45%), Monocytes 8% (3-9%), Eosinophils 2% (0-6%), Basophils 0%. The D dimer level was < 0.48 mcg/ml (0.00-1.19 mcg/ml). A PVL study was negative for DVT. He was diagnosed to have cellulitis and was placed on Keflex 500 mg po Q6 hrs, for 7 days with recommendation outpatient follow up with his PCP in a week, when he received a second course of antibiotics for unresolved suspected cellulitis.
Additional specialized laboratory evaluations from 2/10/2013 revealed Rheumatoid Factor < 20 IU/ml (0-20 IU/ml), ANA positive in 1:1280 and speckled pattern, C- Reactive Protein 0.7 mg/dl (0-5 mg/dl), Uric Acid level 7.8 mg/dl (3.9-9.0 mg/dl), and Sed Rate 66 mm/hour (0-2 mm/hour).
On 2/2/2013 foot and ankle X-rays revealed advanced degenerative changes of the midfoot including talonavicular joint (Figure 1). There was no fracture, dislocation, or malalignment. There was no osseous abnormality of the ankle. Charcot’s arthropathy was entertained and he was referred for podiatric care. The podiatrist concurred with the diagnosis and treated the right lower extremity with a cast for offloading. In addition, patients used crutches and a wheelchair to get around. From 4/16/2014 through 12/10/2016, he had undergone multiple foot and ankle surgeries which include triple arthrodesis, Lisfranc’s fusion, tendoachillis lengthening [6] bone marrow aspiration, internal and external fixations, osteotomy, and finally arthrodesis. In the process, he was treated for foot wound infection, sepsis, osteomyelitis, and reconstructive surgery. Finally, on 11/30/2016 he was treated by plastic surgery with wound debridement and free muscle flap attachment with microvascular anastomosis facilitating wound healing. In total, he has required 13 surgical procedures (5 orthopedic surgeries involving the ankle, midfoot, and forefoot, 7 applications of internal/external fixator implant and explant, and at last reconstructive plastic surgery). Later, he was transitioned to an orthopedic fitted boot resuming full weight bearing and ambulation.
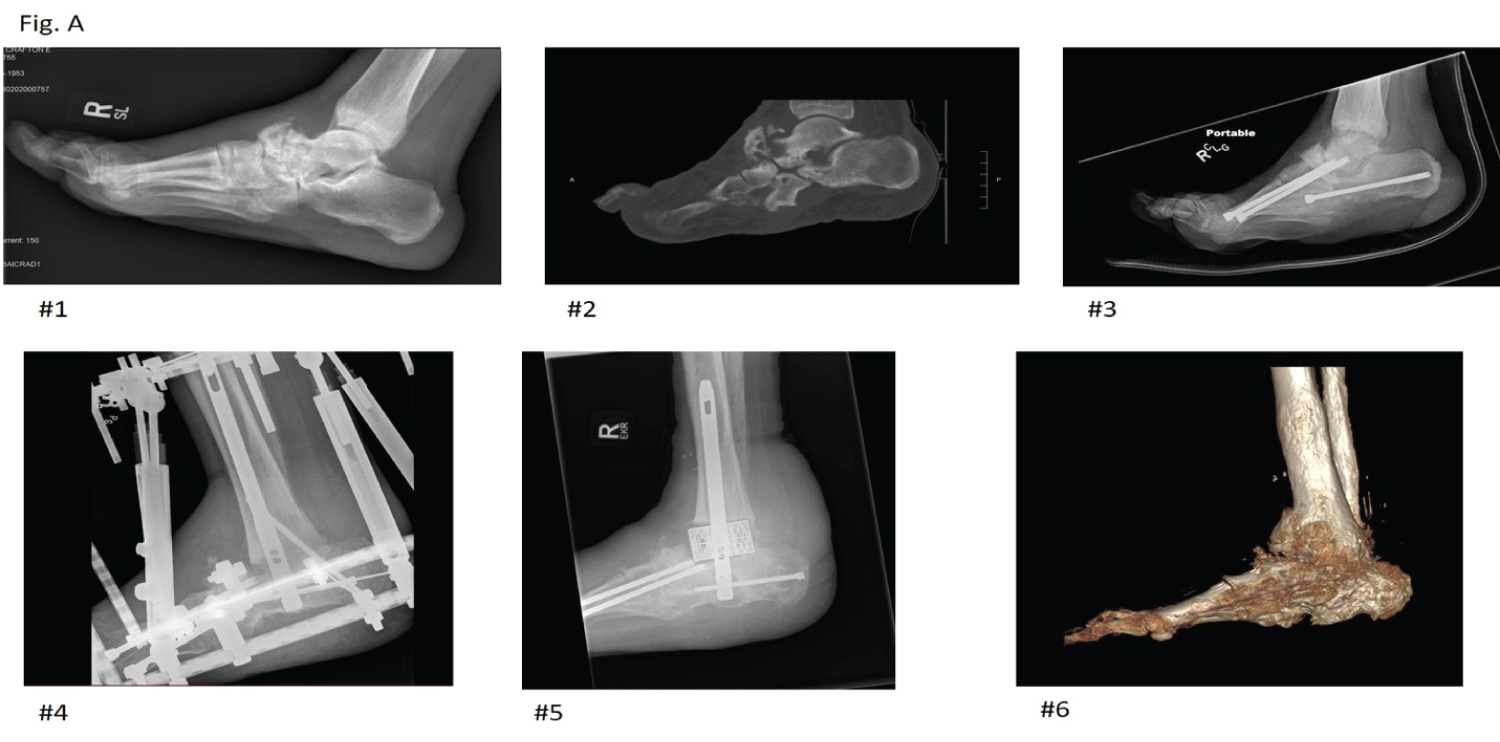 Figure 1: Right foot and ankle images.
Figure 1: Right foot and ankle images.
1. Right ankle X-ray (2/2/2013)
Advanced degenerative changes of the midfoot including the talonavicular joint.
2. Right foot CT scan (2/11/2014)
Neuropathic joint at the midfoot and hindfoot including chronic fracture at the distal talus, medial subluxation at the talonavicular joint.
3. Right foot and ankle X-ray (7/19/2014)
Charcot changes throughout the foot, status post triple arthrodesis and Lisfranc fusion
4. Right ankle and foot X-ray (8/28/2015)
Impression: Hindfoot fusion. Resection of distal fibula. Large defect in the distal tibia is suggestive of osteomyelitis.
5. Right foot and ankle X-ray (5/8/2017)
(1) Previous cage placement between distal tibia and calcaneus, with no significant residual talus, with incomplete osseous union. (2) Solid-appearing osseous union hindfoot, midfoot, and portion of visualized tarsometatarsal joints. (3) Extensive soft tissue swelling around ankle, hindfoot, and midfoot. (4) Nonspecific diffuse periosteal reaction distal fibula and tibia but no evidence of focal bony destruction.
6. Right foot and ankle CT scan (8/15/2021)
(1) There is evidence of interval healing with decreased lucency about hardware and robust osseous ingrowth at buttress cage. (2) No acute fracture or erosion. (3) Persistence of sever extensive tissue thickening/edema.
View Figure 1
During this period, his medical management of diabetes and its associated complications namely, acute heart failure, acute respiratory insufficiency, sepsis, and acute kidney failure, were managed medically involving respective specialists, including care in the intensive care unit (ICU). He recovered from these life-threatening complications and was discharged from the hospital for outpatient care.
He was seen in consultation in our Wellness Clinic on 11/19/2016 and was recommended to adopt a whole food plant-based diet (75% complex carbohydrate, 15% protein (plant) and 10% fat) [7]. He achieved remission of diabetes, went off insulin and oral antidiabetic medications, and maintained HbA1c lower than 6.0% (Figure 2, Figure 3 and Figure 4). In the meantime, his heart function by echocardiographic evaluation revealed improved EF from 35% on 1/7/2011 to 55% on 5/6/2016. His renal function also stabilized with GFR of 31 to 34 ml/min/1.73 m 2 (improved from 11.6 ml/min/1.73 m 2 on 7/29/2016 when he was treated for sepsis and acute renal failure). Since 4/20/2016, his HbA1c has stayed lower than 6.1% (range: 4.7% to 6.1%) up until 11/18/2021.
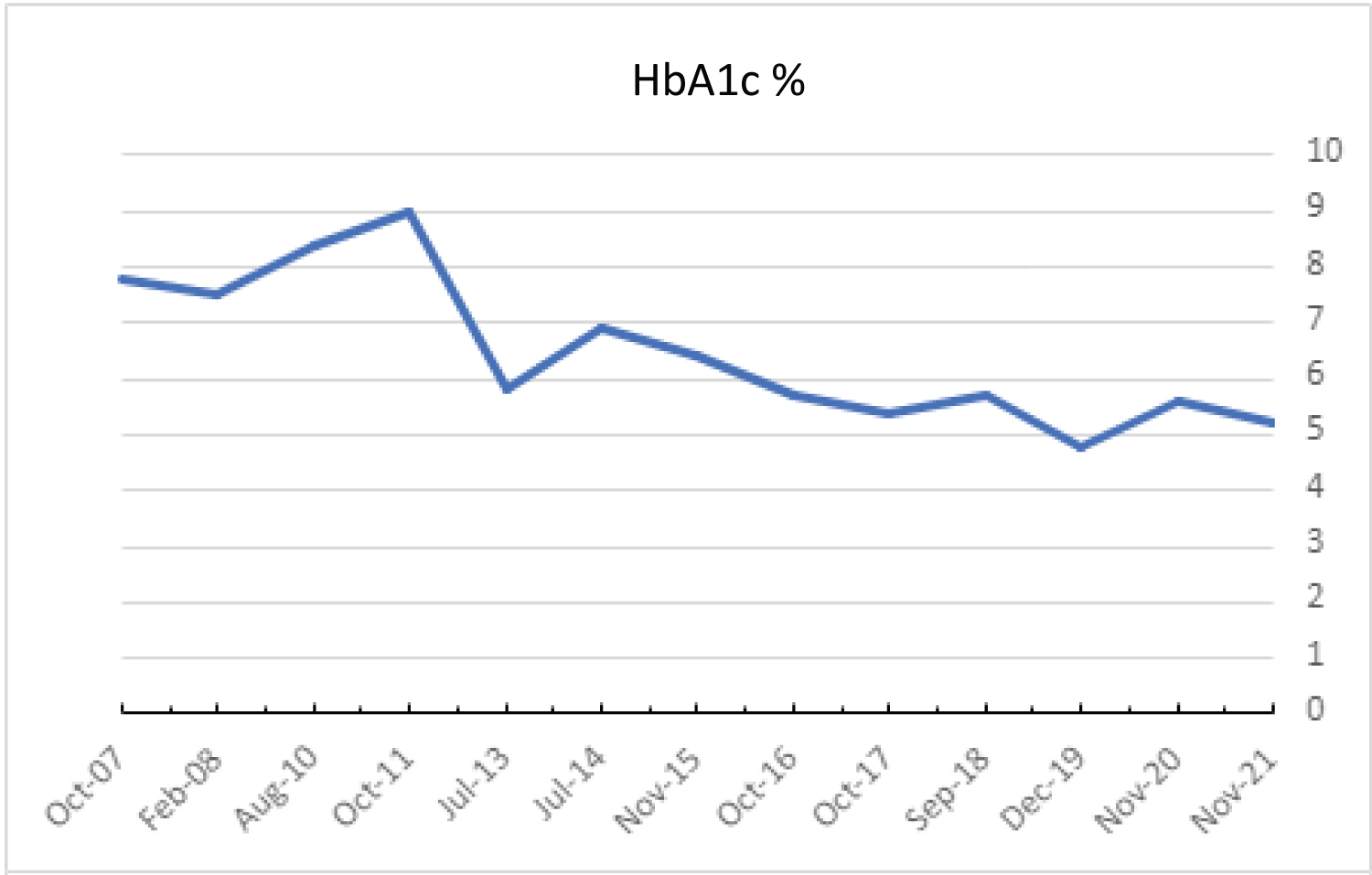 Figure 2: Trend in the yearly averaged level of HbA1c %.
View Figure 2
Figure 2: Trend in the yearly averaged level of HbA1c %.
View Figure 2
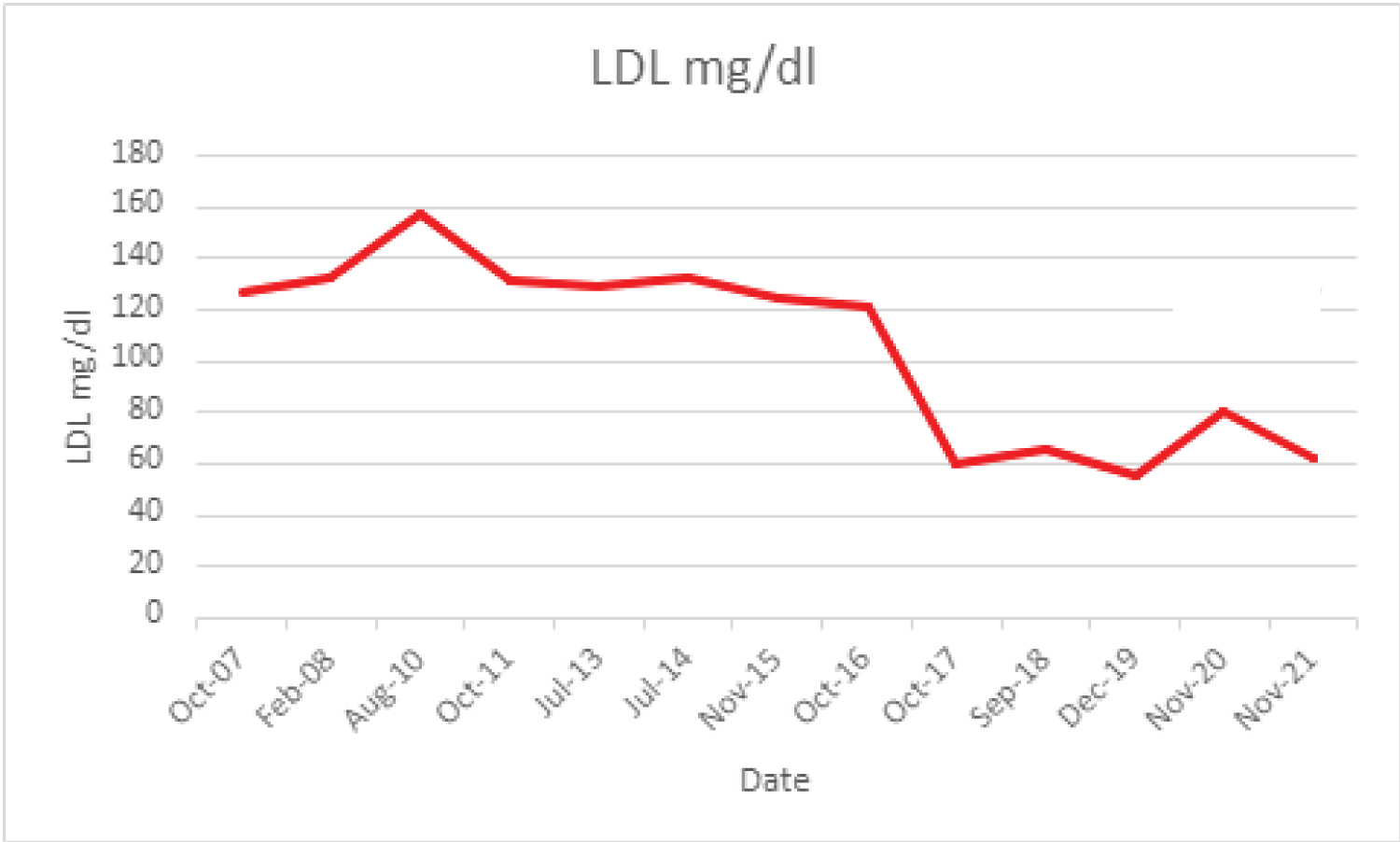 Figure 3: Trend in the yearly averaged level of LDL cholesterol (mg/dl).
View Figure 3
Figure 3: Trend in the yearly averaged level of LDL cholesterol (mg/dl).
View Figure 3
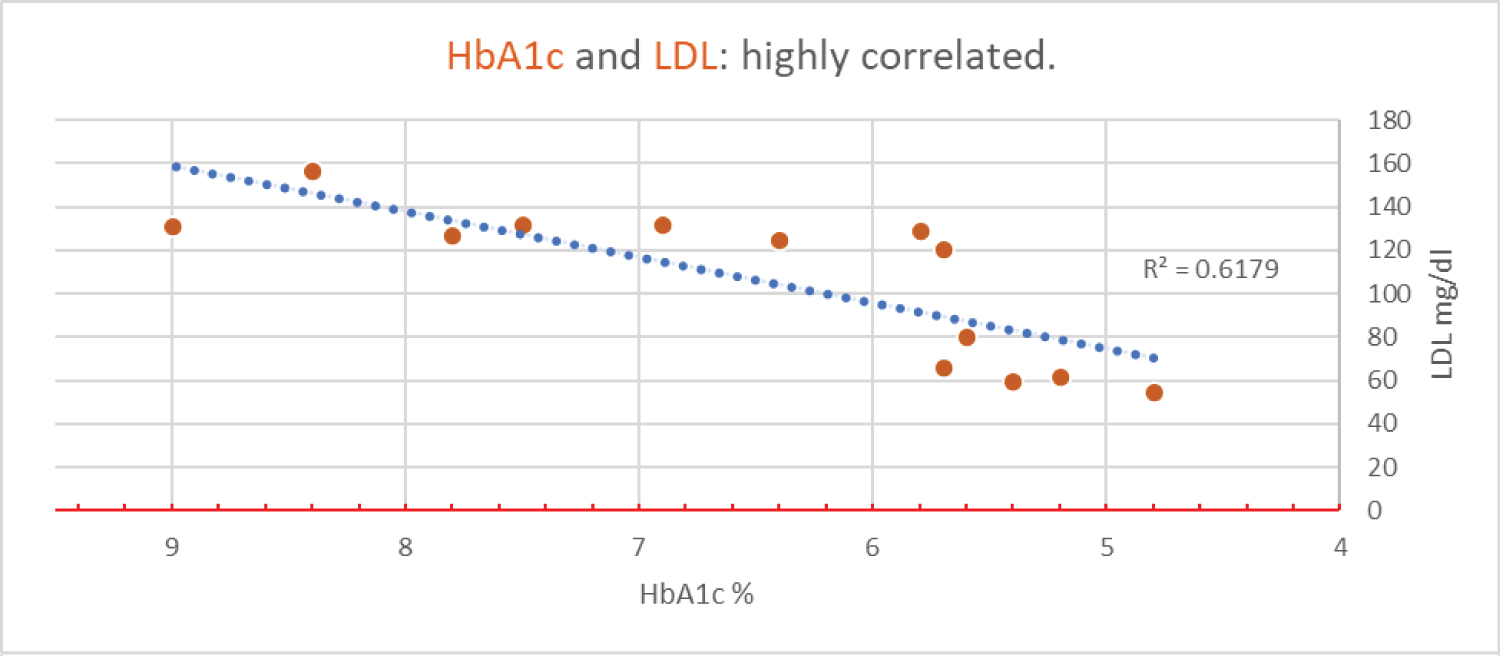 Figure 4: HbA1c and LDL: Highly correlated.
View Figure 4
Figure 4: HbA1c and LDL: Highly correlated.
View Figure 4
The results are summarized in Table 1 and Table 2. Transitioning from the Standard American Diet (SAD) to a Plant-Based diet improved diabetes with decrease in mean HbA1c and Fasting Blood Glucose (FBG). Although the mean GFR was lower compared to before plant-based diet, it had improved from the lowest GFR of 11.6 ml/min/1.73 m 2 during the acute phase of renal insufficiency and reached a platau with plant-based diet [8]. All the components of lipids have improved after adopting a plant-based diet. His weight has gradually increased, partly due to sedentary lifestyle and wearing the heavy boot in the right foot. Similarly, the systolic blood pressure had increased, but the diastolic blood pressure was lower.
Table 1: Averaged clinical parameters - before and after dietary intervention. View Table 1
Table 2: Yearly averaged hemoglobin A1c and LDL cholesterol. View Table 2
The neuropathic condition affects the sensory-motor nerves along with the autonomic nerves, commonly in the lower extremities involving the foot and ankle. Long-term hyperglycemia leads to excess neuronal glucose absorption [9,10] which affects cellular metabolism through (1) Increased flux of glucose and other sugars through the polyol (sorbitol) pathway, (2) Overactivity of the hexosamine pathway, (3) Increased formation of advanced glycated end products (AGEs), (4) Increased expression of the receptor for AGEs and its activating ligands, (5) Activation of protein kinase (PK) C isoforms, (6) Over production of reactive oxygen species (ROS), leading to mitochondrial and cellular damage [11]. In addition, saturated fatty acids (SFA) put excess metabolic demand on the mitochondrial oxidative phosphorylation there by increasing formation of oxygen species, further damaging the mitochondria, and affecting mitochondrial bioenergetics [12]. Functionally impaired mitochondria are unable to produce sufficient neurotrophin-3 (NT-3) and nerve growth factor (NGF) to enable nerve repair and regeneration [12,13].
The extremely long axons of the lower extremities (some more than 3 feet), originating from a small neuronal body, are vulnerable at its distal site because of insufficient nutritional support and environmental factors leading to increased susceptibility to degeneration and dysfunction [14]. Furthermore, the peripheral nerve has sparse vascular supply with impaired autoregulation and is likely incurring hypoxic damage [15]. Recently it has been shown that autonomic neuropathy in the bone marrow impairs activation and migration of endothelial precursor cells (EPC), thereby affecting angiogenesis and neurotrophic function [16-18].
These complex factors lead to neurodegeneration, and it is understandable that inhibition of a single metabolic factor might not be sufficient to treat neuropathy [15].
There is evidence of significant arteriovenous shunting in the neuropathic limb. Blood flow by doppler studies have demonstrated markedly abnormal blood velocity profiles (sonograms) in diabetic autonomic peripheral neuropathy. This is characterized as increased diastolic flow, loss of pulsatility, decreased transit time, raised ankle systolic pressure, and associated arterial medial wall calcification (Figure 5) [19]. In addition, there is reduced arteriovenous oxygen saturation in the neuropathic limb [20]. The capillary network is short circuited resulting in less oxygen and nutrients delivered to the surrounding tissue. Thirdly, when the arteriovenous anastomoses are open (loss of sympathetic tone) there is a rise in venous pressure which spreads to the capillary bed, raising capillary pressure. This would partially account for the edema in the affected neuropathic limb [19].
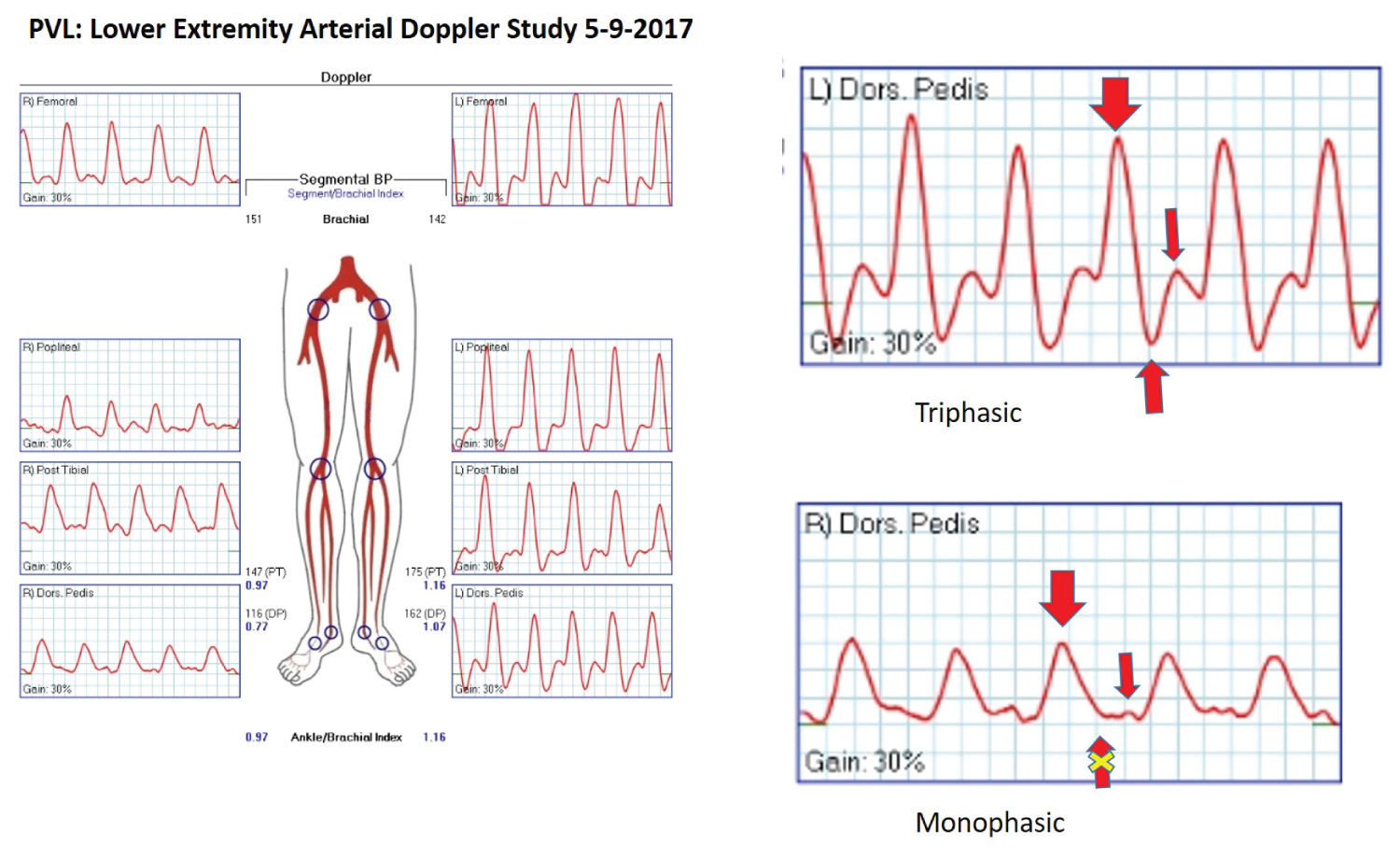 Figure 5: PVL - Lower extremity arterial doppler study.
Figure 5: PVL - Lower extremity arterial doppler study.
Right Leg: Biphasic to monophasic flow pattern. As illustrated in the right-side panels: upper right dorsalis pedis artery flow dynamics is triphasic, in contrast to the bottom right dorsalis pedis artery flow dynamic is monophasic (early diastolic flow reversal is absent, marked as "x" on the bottom arrow). This indicates continuous blood flow both during systole and diastole of cardiac cycle (hyperemic).
Left Leg: Multiphasic in all levels, which is normal flow pattern.
View Figure 5
The recognized predisposing factors are neuropathy and increased mechanical forces, bone resorption and fractures, trauma, and inflammation. Patients with diabetic neuropathy have limited joint mobility, increased plantar pressure, abnormal gait, and sensory-motor deficit which subject them to frequent injury due to internal instability and external trauma [21].
These combinations of factors perpetuate an inflammatory condition from acute to progressive chronic arthropathy incurring damages, deformity, fractures, dislocations, subluxations, ulceration, osteomyelitis, and surgical trauma.
Hyperglycemia causes direct nerve toxicity via several mechanisms: (1) Increased oxidative stress, (2) Increased formation of diacylglycerol (DAG) with subsequent activation of protein kinase C (PKC), and accumulation of advanced glycated end products (AGEs), and increased flux through the polyol pathway [22]. These combine to disrupt axonal mitochondrial metabolism and impair fast and slow axonal transport necessary for trophic support of distal axonal tips. In addition, metabolic abnormalities associated with hyperglycemia, hyperlipidemia, circulating free fatty acids, hypertension, and adipocytokines, independently and in combination, impair vascular endothelial function, impair nitric oxide-mediated vasodilation ultimately leading to nerve and tissue hypoxia, and finally tissue degeneration, atrophy, and dysfunction. In addition, there is overwhelming local inflammation with excessive production of cytokines namely tumor necrosis factor alpha (TNF alpha) and Interleukin 1 beta (IL-1beta). Next in pathophysiology, the cytokine driven elevation of the receptor activator of nuclear factor kappa B ligand (RANKL) is expressed, which in turn, enhances the synthesis of nuclear factor kB (NF-kB). This promotes osteoclast maturation and osteoclastic activity, leading to osteoporosis in the affected bones making them susceptible to fracture with minimal trauma [23].
Diabetic polyneuropathy is the most acquired diffuse disorder of peripheral nervous system. It is generally assumed that insulin benefits humans and experimental diabetic neuropathy indirectly by lowering glucose levels. In addition, insulin also provides potent direct support to neurons and axons, and there is a possibility that abnormalities in direct insulin signaling on peripheral neurons relate to the development of this disorder. Commonalities in downstream tyrosine kinase activation may allow insulin, IGF-1, and classic neurotrophins (NGF, NT-3, and CNTF), and non-neurotrophic growth factors (VEGF) to support in similar ways. Nonetheless, intensive insulin therapy prevents the development of diabetic neuropathy. In type 2 diabetes, many patients develop insulin resistance such that intermittent elevated circulating insulin levels fail to transduce intracellular signals. Lack of insulin access to peripheral neurons may represent one additional failed support mechanism that contributes to neuropathy in the face of metabolic, structural, and ischemic insults [13]. Moreover, any insulin producing pancreatic beta cells also release equivalent amount of C-peptide. This peptide is found to have biologic effects on neurons and neuronal microvasculature preventing diabetic neuropathy [24,25]. This has been confirmed clinically by human trials [25].
The present management of Diabetic Charcot Neuroarthropathy (DCN) centers around offloading orthosis, immobilization, and surgical interventions. There has been very little progress being made in medical management to alter the course of neuroarthropathy, vasculopathy, and inflammation. It has been observed that long uncontrolled hyperglycemia is the primary cause, and its associated metabolic abnormalities are the contributing factors for developing DCN. So, it makes intuitive sense to focus on diabetic control as early as possible to forestall progression of this disease.
Several features of metabolic syndrome have been linked to neuropathy, particularly obesity and dyslipidemia, independent of hyperglycemia [22,26,27].
Diabetes Control and Complications Trial (DCCT) has demonstrated that intensive glycemic control delayed the onset and progression of neuropathy in Type I diabetics. Despite this achievement, twenty-five percent of DCCT subjects receiving intensive glucose control still progressed to clinical neuropathy [28]. Apart from glycemic control alone, lifestyle interventions have shown some promising results. The Steno-2 study, multifactorial intervention and cardiovascular disease in patients with type 2 diabetes, in the intensive treatment arm, reductions in the risk of nephropathy, retinopathy, and autonomic neuropathy were observed after four years of observation and maintained at eight years [29].
In experimental mice model, hyperglycemia and dyslipidemia have been found to contribute to the pathogenesis of neuropathy [12]. In this model, changing mice from an SFA-rich diet to a MUFA-rich diet restored both nerve and mitochondrial function [14].
Balducci, et al., 2006 with lifestyle intervention of diet and exercise has observed preventing the onset of neuropathy in those with prediabetes and diabetes [30,31].
In our patient a high-fiber, low-fat plant-based diet consisting of vegetables, legumes, fruits, whole grains, limited quantity of seeds and nuts have provided an optimal dietary treatment achieving diabetes remission [7] and in improving metabolic abnormalities (improving lipids and controlling blood pressure), and likely improved (autonomic) neuropathy [29,31]. A plant-based diet has been seen to have reversed diabetic macular edema, a complex neurovascular abnormality [32]. In this case, diabetes control along with control of its associated metabolic abnormalities, permitted in arresting the progression of arthropathy and allowed healing to occur. Likely, this prevented further complications including amputation, and even threat to life [33,34].
Early diagnosis of Charcot’s Foot is indispensable. In a patient with history of diabetes having neuropathic symptoms of pain and numbness in the feet should trigger prompt and accurate diagnosis. The plain-film X-ray will miss the early pathology of Charcot’s foot, which was the case in our patient. An MRI scan could have provided a definite diagnosis at this early stage by identifying microfractures, bone marrow edema to direct prompt treatment of offloading, immobilization [5]. It has been known that hindfoot and ankle are the most common sites to require surgical treatment, due to joint instability [3]. However, the forefoot and midfoot CN can generally be successfully managed with conservative treatment of offloading and immobilization, without need for surgery [3]. This could have prevented the progressive and damaging complications of skeletal breakdown requiring multiple surgeries and long-term disability [35,36].
At present, there is no effective medical treatment for diabetic neuropathy, except for tight blood glucose control. Therefore, maintaining optimal glucose homeostasis carries a high priority. But clinically this remains a challenge. With this constraint, early detection of neuropathy is important to implement prompt treatment. In addition, restoring optimal pancreatic beta cell function, in combination with adequate secretion of neurotrophic growth factors, is of primary importance to repair neuronal damages and to maintain their integrity. To date, lifestyle changes with plant-based diet provide the best chance for achieving this goal. This will help in preventing progression of diabetic neuropathy, vasculopathy, inflammation, arthropathy; and as a result, in preventing the devastating complications of Charcot’s neuroarthropathy. This case exemplifies the effectiveness of achieving diabetic remission with plant-based diet, even in its advanced stage of neuro-vascular-arthropathy, by facilitating in healing by the way of controlling inflammation, preventing bone and joint destruction, thereby avoiding amputation, and restoring the foot to a useful level of function.
None.
The author acknowledges the contribution of Lecretia R. McCollum for making the statistical analysis, preparing the tables, and curating the images.