Infective endocarditis (IE) is a potentially life-threatening disease process that may result in several long-term sequelae. Transthoracic echocardiography (TTE) may be inadequate to diagnose IE in up to 20% of patients secondary to poor image quality or the inability to identify all lesions present [1]. TTE has shown to be less sensitive concerning identification of abnormalities of left heart structures, whereas the sensitivity for detection of vegetations on native valves is close to 100% with transesophageal echocardiography (TEE) [1]. Additionally, intraoperative TEE (IOTEE) has been shown to identify undiagnosed pathology and residual defects after surgical intervention which allows for immediate correction. For example, in retrospective reviews, both pre- and post-cardiopulmonary bypass (CPB) IOTEE led to changes in the planned surgical procedure; the incidence of the former ranging from 6% to 29%, whereas the latter ranged from 0% to 7% [2].
In cases of IE, TEE is vital for detecting other cardiac abnormalities such as septal defects. It has been demonstrated that atrial septal defects may allow transmission of left sided IE to the right side of the heart and lungs [3].
A 42-year-old male presents to the ED with an episode of chest pain and orthopnea. He reports a 1-month history of fever, night sweats, fatigue, and 30 lb weight loss. His physical exam is positive for diffuse rales, a 3/6 systolic murmur, and painful evolving erythematous lesions on the palms of his hands.
TTE reveals left ventricular and atrial dilatation with LVEF 60-64% and a 2cm x 0.7 cm echodensity on the base of the anterior leaflet of the mitral valve (A2) with perforation and severe mitral regurgitation (MR) with concern for IE. His aortic valve is tricuspid with mild aortic insufficiency (AI). Cardiothoracic surgery is consulted for mitral valve replacement.
After an uneventful induction of anesthesia and placement of lines, a pre-bypass TEE confirms the presence of the A2 vegetation (Figure 1) and perforation with severe MR (Figure 2). The patient is also found to have moderate AI (Figure 3) and a patent foramen ovale (PFO) with left to right shunting (Figure 4). The surgeons are informed of the new findings and plans are made to close the PFO and to inspect the aortic valve. Aortotomy is made, and the aortic valve is found to have redundant tissue. Both the aortic and mitral valves are replaced with mechanical St. Jude's valves. The PFO is closed with a single suture, followed by de-airing of the heart under TEE guidance and weaning from CPB.
The case is completed without further complications. The patient is transported to the ICU and extubated the following morning.
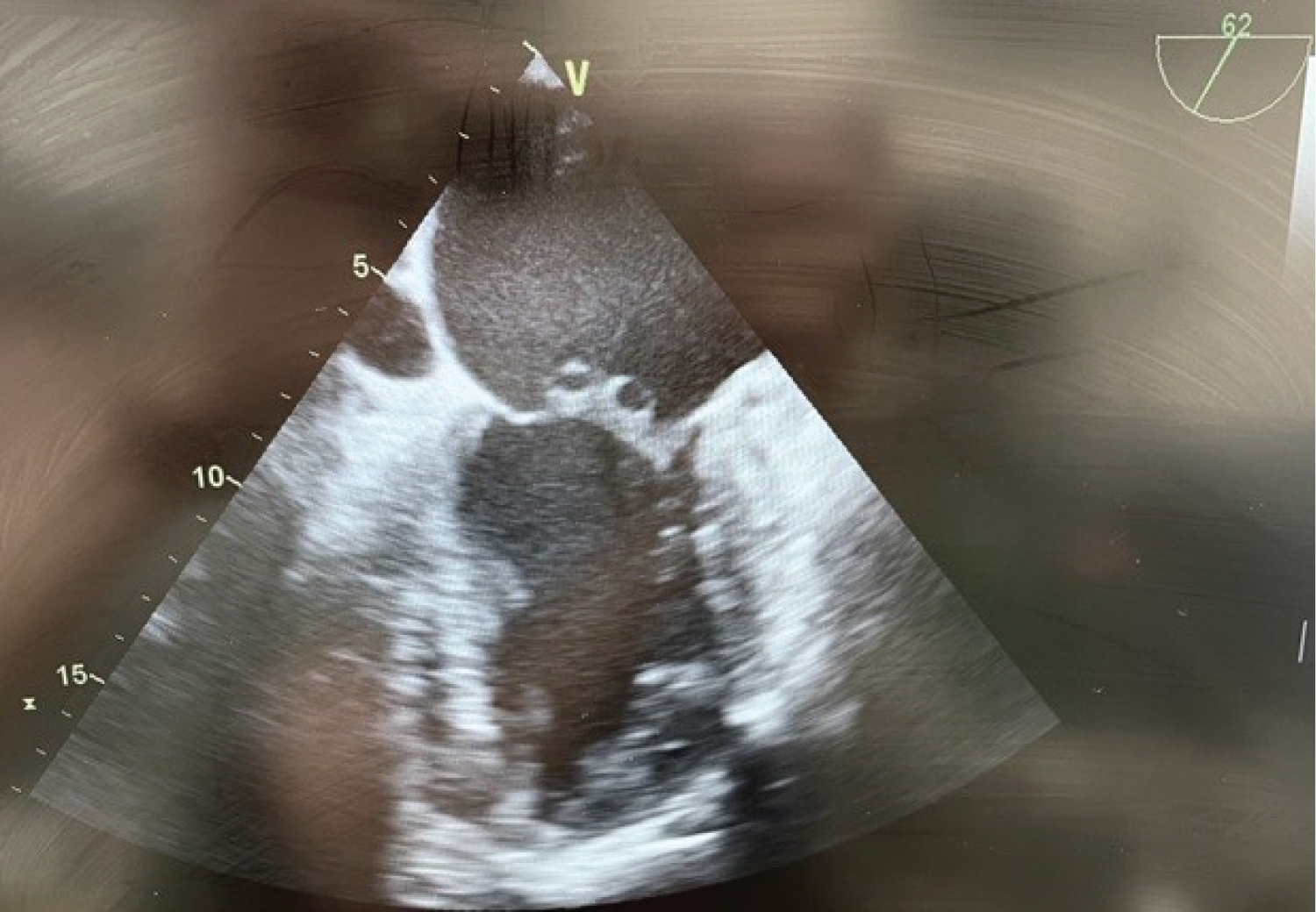 Figure 1: Pre-bypass TEE midesophageal bicaval view illustrating the PFO.
View Figure 1
Figure 1: Pre-bypass TEE midesophageal bicaval view illustrating the PFO.
View Figure 1
 Figure 2: Pre-bypass TEE midesophageal mid commissural view illustrating MV vegitations.
View Figure 2
Figure 2: Pre-bypass TEE midesophageal mid commissural view illustrating MV vegitations.
View Figure 2
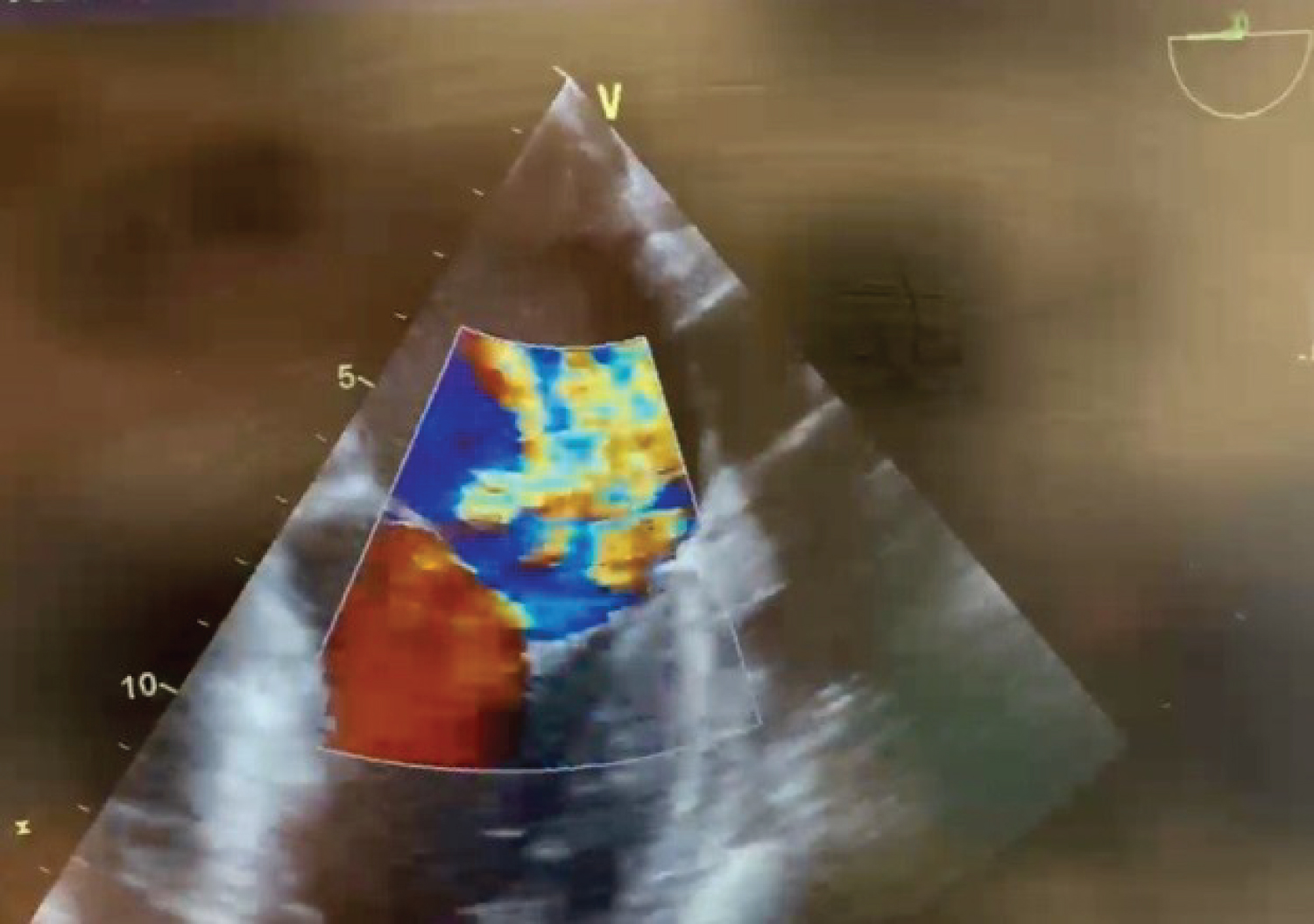 Figure 3: Pre-bypass TEE midesophageal four chamber view illustrating severe MR.
View Figure 3
Figure 3: Pre-bypass TEE midesophageal four chamber view illustrating severe MR.
View Figure 3
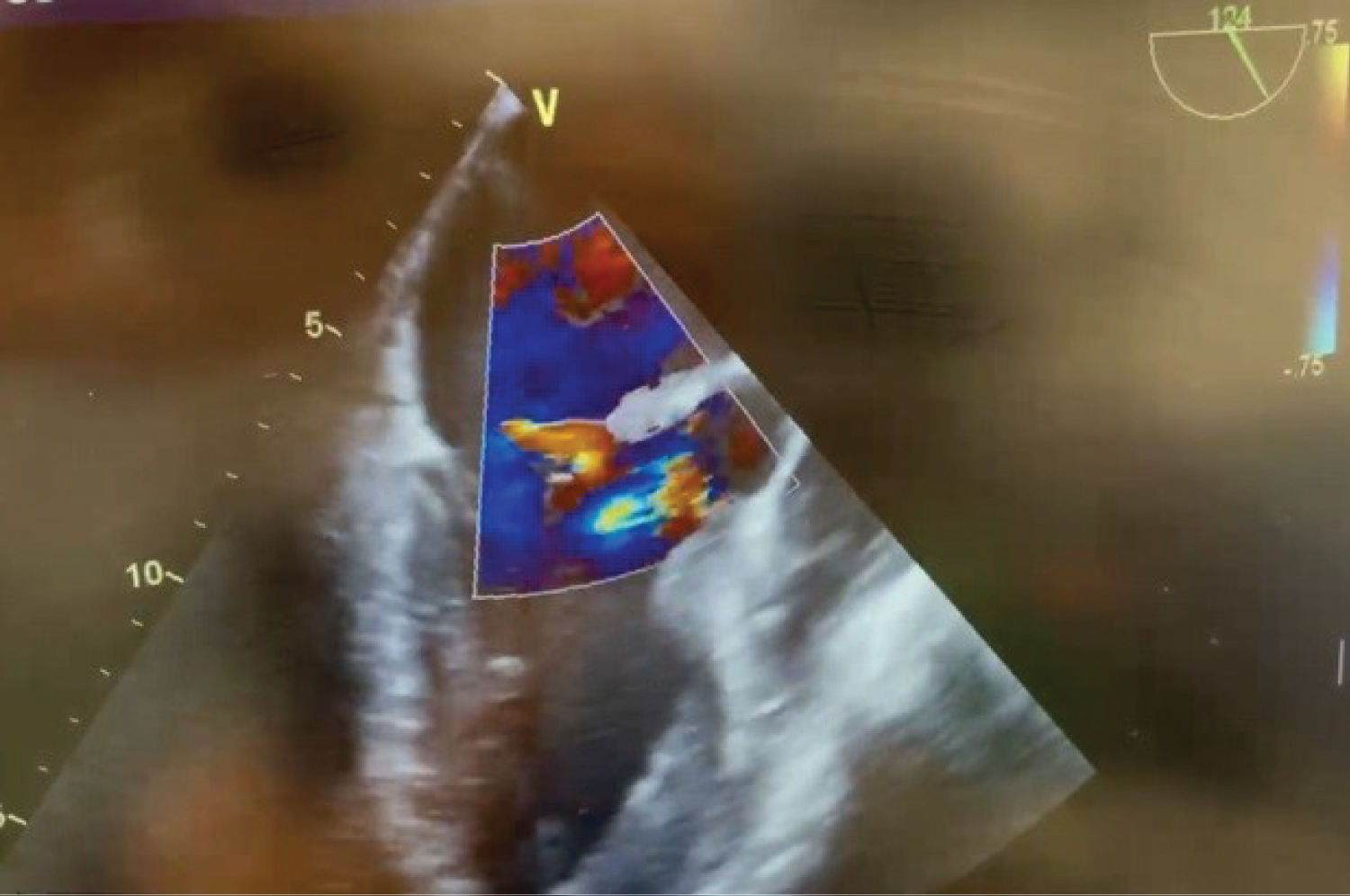 Figure 4: Pre-bypass TEE midesophageal long axis view illustrating mitral and aortic insufficiency.
View Figure 4
Figure 4: Pre-bypass TEE midesophageal long axis view illustrating mitral and aortic insufficiency.
View Figure 4
This case reinforces the importance of TEE in both the management of IE and during valvular cardiac surgery. In patients with IE, close inspection of each valve is a critical step in the perioperative evaluation. There is also a possibility of spreading the disease from one side of the heart to the other if a septal defect is present. Surgical manipulation of the vegetative valve increases this risk. Ultimately, a careful IOTEE exam was crucial for guiding surgical management during this case and may have saved our patient increased perioperative morbidity or a need for reoperation.