Neurodevelopmental Disorders (also known as Intellectual and Developmental Disabilities-ID/DD) are associated with multiple-complex-health-conditions that, in contrast to children, are often not evaluated and/or managed properly as adults. The specialty of Developmental and Behavioral Pediatrics exists for children with ID/DD, but there is no equivalent specialty for the adults. Since Family Medicine has taken the lead in providing primary care for adults with ID/DD, we propose that Family Medicine follow the example of Pediatrics by organizing multisite University-based Quality Improvement (QI) programs in Family Medicine Departments (with Residents, Students, and Fellows). To begin the process and create focus, the specific problem of obesity (and its complications) could be addressed in the adults utilizing Quality Improvement methods designed to promote teaching, research, and improved health outcomes. Participating University sites could then organize to create a new academic professional organization focused on all health-issues of adults with ID/DD, as occurred in Pediatrics for children.
"Neurodevelopmental disorders" (NDD), also known as Intellectual and Developmental Disabilities (ID/DD), are genetic or acquired chronic health conditions that interfere with various functions of the brain (Figure 1). These conditions persist into adulthood and are responsible for 4 categories of "disabilities"; namely, mild, moderate, or severe 1) Cognitive dysfunction, 2) Motor dysfunction, 3) Seizures, and/or 4) Maladaptive behavior (Figure 2). These four categories of health conditions, or "complications", can occur singly or in various combinations and may also lead to numerous secondary health "consequences" (e.g., obesity, osteoporosis, drug toxicity, etc.). In addition, there may also be complications specific for a syndrome, unrelated to brain dysfunction [1,2].
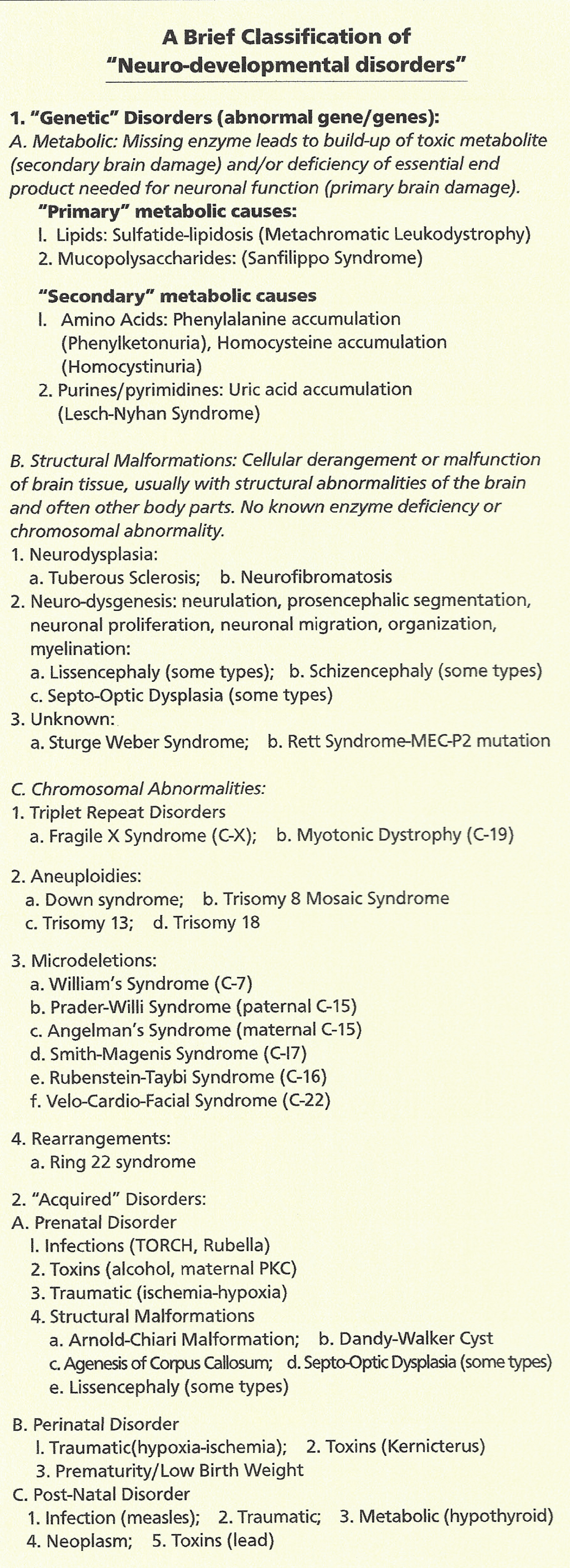 Figure 1: A brief classification of neuro-developmental disorders.
View Figure 1
Figure 1: A brief classification of neuro-developmental disorders.
View Figure 1
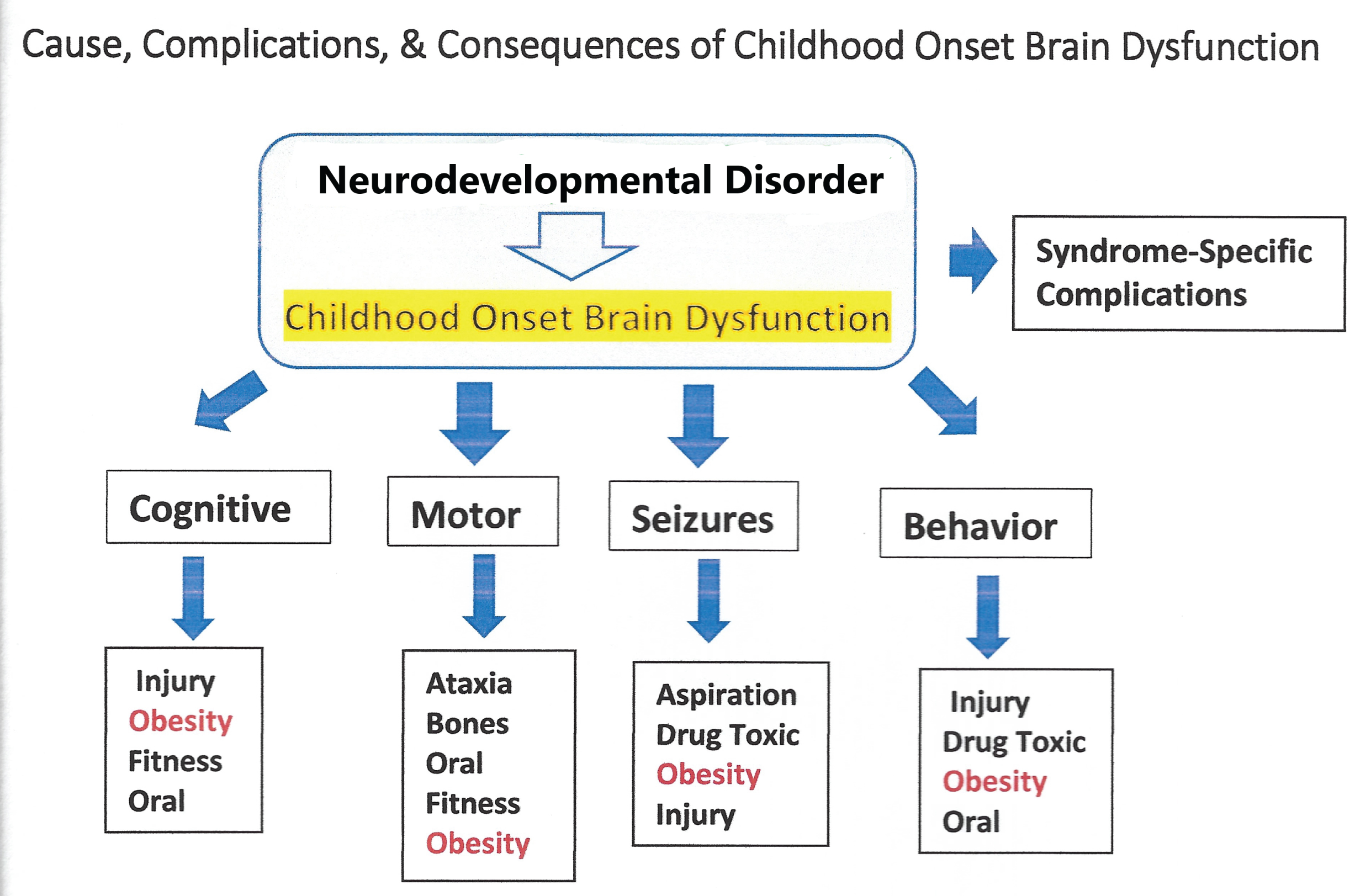 Figure 2: Cause, complications and consequences of childhood onset brain dysfunction.
View Figure 2
Figure 2: Cause, complications and consequences of childhood onset brain dysfunction.
View Figure 2
At least since the 1800's [3], physicians have recognized the complexity of health conditions experienced by adults with NDD. In the United States, an Accreditation Council for Graduate Medical Education (ACGME) approved medical specialty (Developmental and Behavioral Pediatrics) which addresses these health conditions in children has existed in the United States since 1999 [4]. Unfortunately, there are no analogous programs designed to train specialist physicians in the research, teaching, and service of health-conditions of adults with neurodevelopmental disorders [5-9]. Thus, in the United States, when children with neurodevelopmental disorders are transitioned into adult services, there are no ACGME approved "Board Certified" specialists in adult Neurodevelopmental Medicine to continue the same high-quality health services they received as children. A similar situation appears to exist internationally.
In the universities, there has been little interest in development of 1) University-based medical education [5] 2) "Quality Improvement" Programs [10] and/or 3) Clinical research [11] designed to improve delivery of high-quality evidence-based healthcare for adults with NDD. Therefore, as of 2002, even though remarkable improvements had been achieved for social, non-medical community services (e.g., residential, employment, educational, recreational) modern generations of physicians who provide primary healthcare to adults (Family Physicians and Internists), remain untrained regarding comprehensive evaluation of health-conditions that often present in adults with neurodevelopmental disorders (e.g., obesity, osteoporosis, lack of genetic vs. acquired etiologic diagnosis, etc.) [12].
As former US Surgeon General David Satcher MD succinctly stated in the introduction to the historic Surgeon General's Report of his Conference in 2001, "as services for people with mental retardation evolved, our attention to their health lessened". Then US Secretary of Health and Human Services, Tommy G. Thompson, concluded in the same report, "too few providers receive adequate training in treating persons with mental retardation. Even providers with appropriate training find our current service system offers few incentives to ensure appropriate health care for children and adults with special needs. American health research, the finest in the world, has too often bypassed health and health services research questions of prime importance to persons with mental retardation" [11].
While major healthcare-service deficiencies still exist for adults with neurodevelopmental disorders, healthcare-services for children with neurodevelopmental disorders, have significantly improved and how these improvements were achieved could serve as a model for improvement of healthcare quality for adults. In the United States, health issues of children with neurodevelopmental disorders greatly benefited from the work of the Society for Developmental and Behavioral Pediatrics (SDBP) (SDBP Website) [4]. Formation of the SDBP initially began in 1976 by eleven University-based Directors of Training Grants provided by the W.T. Grant Foundation of New York City. The purpose of those training grants was to train Pediatric Residents in how to better care for children with ID/DD. After meeting yearly for 5 years, from 1977-1982 (required as a condition of funding), these eleven Medical School-based training Directors (all University Professors of Pediatrics) and colleagues formally created the SDBP for the purposes of continuing to exchange ideas and to encourage research in the field by presenting research papers at its annual meeting, establishing additional training programs, and creation of a Society journal. In addition, because of the advocacy of the Society (SDBP website), since 1986 the U.S. Maternal and Child Health Bureau of HRSA has provided funding for 3-year University-based research/academic Fellowship Programs in the field of Developmental and Behavioral Pediatrics. In the United States, several hundred ACGME certified Board-Certified pediatric specialists in Developmental & Behavioral Pediatrics now exist for children (SDBP website) [4].
Recognizing the deficiency of quality primary health services for adults with ID/DD, the discipline of Family Medicine has been comprehensively addressing this problem since 2011 [12]. Family Medicine has been providing culturally competent compassionate primary care, but due to lack of quality-improvement programs and clinical research, major deficiencies in the practice of evidence-based-medicine for adults with Intellectual Disability still exist. In addition, ACGME-certified Fellowships have not been established in Family Medicine for adults with ID/DD as they have been for children.
To begin to eliminate these health-disparities, we propose that the specialty of Family Medicine follow the lead of Pediatrics. This could begin by government and/or private foundation funding of "Quality Improvement" [13,14] grants awarded to University Departments of Family Medicine, with the stipulation that Directors of these "Quality Improvement" grants meet regularly to share outcomes and to also establish training of medical students and residents and conduct "Quality Improvement" Programs which address health conditions of adults with neurodevelopmental disorders [12]. "Quality Improvement" programs are often implemented for general medical practices [14], but it is uncommon for the QI approach to be applied to the adult population of individuals with Neurodevelopmental Disorders [10]. Conditions such as obesity and osteoporosis are examples of health conditions that frequently occur in adults with neurodevelopmental disorders that could easily be addressed using QI methodology. Obesity is an especially important problem because of the associated higher risk of morbidity and mortality from cardiovascular, metabolic disorders, cancer, and many other problems [15]. In addition, there now appears to be an increased risk of poor outcome from COVID-19 infection associated with obesity [16], which may be worse in adults with ID/DD [17]. Developmental and Behavioral Specialist Pediatricians also have difficulty treating obesity in children [18]. If Obesity QI Programs were designed to include multiple University-based sites in a project which involves Medical Students, Residents, Fellows, and Faculty, valuable clinical information needed to improve health of obese adult participants with neurodevelopmental disorders could more readably be obtained. Furthermore, valuable information obtained from such QI Projects would lead to formal research projects designed to build a much-needed evidence-base to promote optimal medical practice for adults with neurodevelopmental disorders.