Background: Adult Hirschsprung's disease (HD) is a rare motor disorder of the gut that is frequently misdiagnosed as refractory constipation and treated with laxatives. The primary pathology of adult HD is the total absence of intramural ganglion cells of the submucosal and myenteric neural plexuses in the affected segment of the bowel. 94% of HD cases are diagnosed before the patient reaches 5-years of age, however, on rare occasion, mild cases of HD may go undiagnosed until they reach adulthood and present with chronic constipation.
Case history: A 60-years male presented with a history of long-standing recurrent constipation for last 10-years intermittently relieved by laxatives with abdominal distention. A sigmoidoscopy was performed which revealed grossly distended proximal colon with fecal retention (mega colon) without evidence of ulcer or growth. A transanal rectal biopsy was performed and sent for pathological examination. Histopathology showed absence of ganglion cells in the submucosa as well as in muscularis propria. Immunohistochemistry (IHC) using calretinin was performed which confirmed the findings and hence a diagnosis of Adult Hirschprung's disease was made.
Discussion: In view of the case history of chronic constipation and mega colon as well as history of laparotomy 15-years back for? intestinal obstruction, a possibility of adult HD was considered and transanal biopsy was taken. H and E section showed mucosa, submucosa with mild chronic inflammation and part of muscularis propria. Ganglion cells were absent in the submucosa as well as in muscularis propria. IHC with calretinin was performed which confirmed the absence of the ganglion cells and nerve innervations in the mucosa. Hence a diagnosis of HD was given. Adult HD should be considered in the differential diagnosis of cases where adult patients present with chronic constipation or even acute intestinal obstruction as curative surgical intervention can be performed to relieve symptoms and reduce further complications.
Adult Hirschsprung's disease (HD) is a rare motor disorder of the gut that is frequently misdiagnosed as refractory constipation and treated with laxatives [1]. The incidence rate of adult HD at present is not known, primarily because this disease is frequently overlooked in the adult population [2]. The primary pathology of adult HD is the total absence of intramural ganglion cells of the submucosal and myenteric neural plexuses in the affected segment of the bowel. 94% of HD cases are diagnosed before the patient reaches 5-years of age. However, the expression ‘adult Hirschsprung's disease’ is used when the diagnosis is made after ten years of age [2]. It is a recto sigmoid lesion in 80% of cases [3]. The first documented case of adult HD was described by Rosin, et al. in 1950 [4].
A 60-years-old male presented with a history of chronic constipation with abdominal distention, intermittently relieved by laxatives. A sigmoidoscopy was performed which revealed grossly distended proximal colon with fecal retention (mega colon) without evidence of any ulcer or growth. In view of history a possibility of adult HD was considered and a transanal partial thickness rectal biopsy was taken. H and E stained section of the biopsy showed unremarkable mucosa, submucosa with mild chronic inflammation and part of muscularis propria. Ganglion cells were absent in the submucosa (Meissner’s) as well as in muscularis propria (Myenteric plexus). Few submucosal and myenteric nerves were hypertrophic (Figure 1A and Figure 1B).
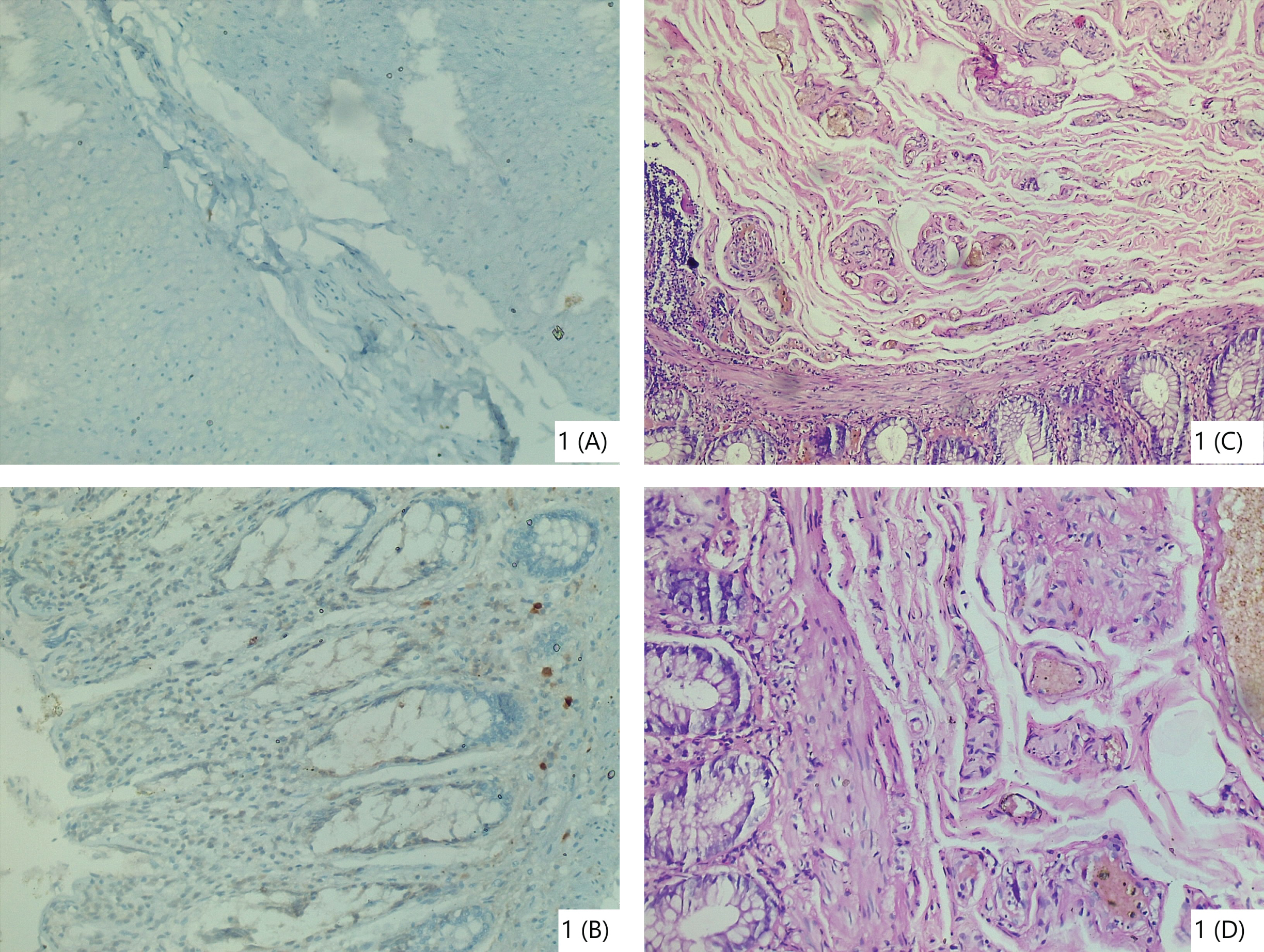 Figure 1: Stenosed segment biopsy shows few hypertrphic nerve fibres and absence of ganglion cells in the submucosa (C,D H&E stain,40x)
Figure 1: Stenosed segment biopsy shows few hypertrphic nerve fibres and absence of ganglion cells in the submucosa (C,D H&E stain,40x)
Absence of ganglion cells in submucosa and muscularis propria confirmed on IHC (A,B Calretinin stain 40x).
View Figure 1
IHC with Calretinin was performed and negative staining for Calretinin confirmed the absence of Ganglion cells. (Figure 1C and Figure 1D). Hence a diagnosis of Adult Hirschsprung's disease was given.
Deloyer’s procedure (Creation of anastomosis between the right or transverse colon and the rectum) was done to remove the affected part and sent for frozen section diagnosis. Proximal and distal margins of the specimen were examined for the presence of ganglion cells. Proximal resection margin showed hypoganglionosis. Hence it was revised (5 cm) and the revised margin showed normal histology. This finding was confirmed on IHC with Calretinin (Figure 2A, Figure 2B, Figure 2C, Figure 2D, Figure 2E and Figure 2F). On permanent sections stenosed segment revealed aganglionosis consistent with the primary diagnosis of adult HD. Postoperative recovery was satisfactory.
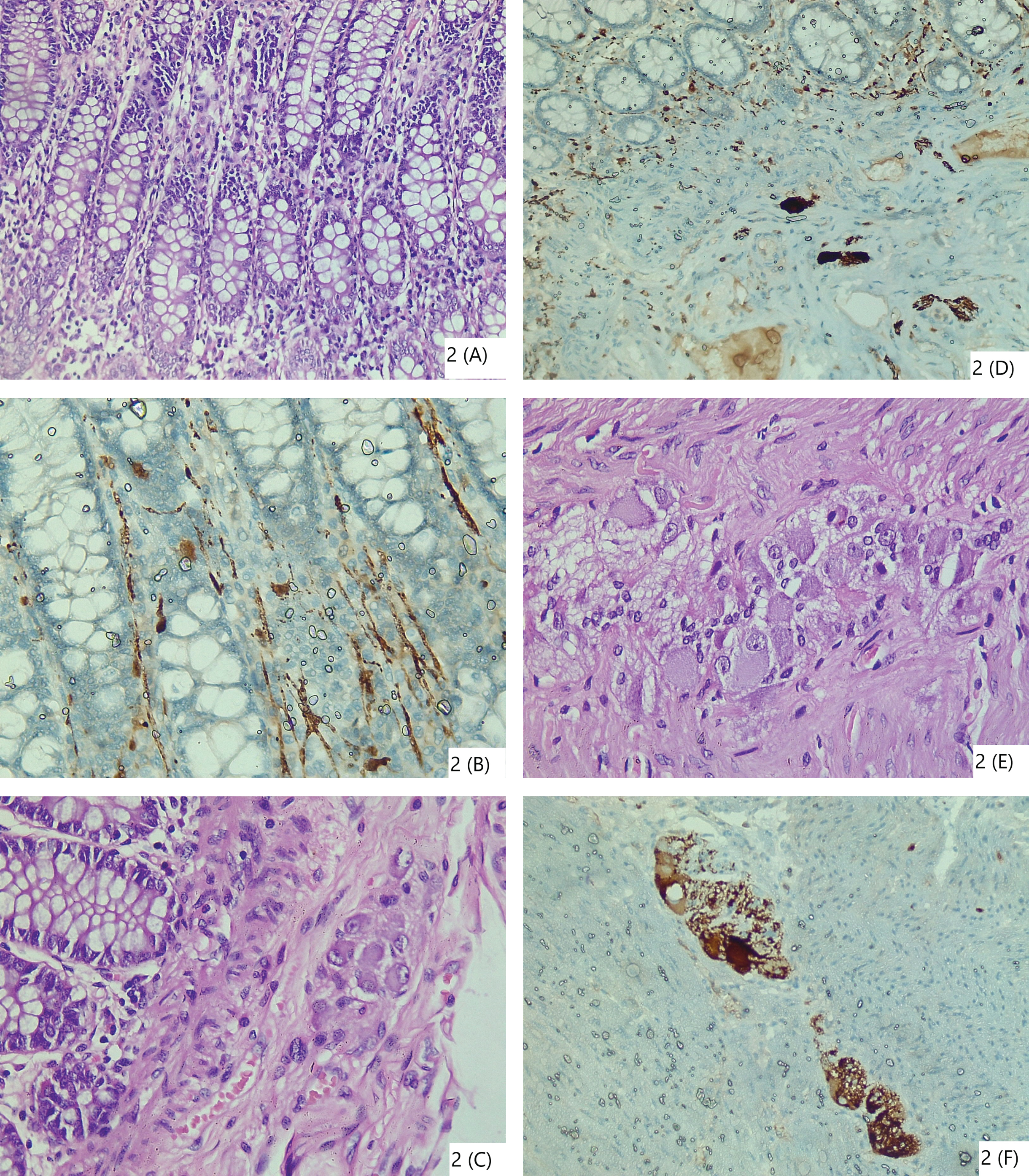 Figure 2: (Proximal resected margin): (A) Normal colonic mucosa showing nerve innervations; (B) IHC highlighting mucosal nerve innervations; (C) Submucosa showing ganglion cells [Meissner's plexus]; (D) IHC highlighting Submucosa showing ganglion cells; (E) Ganglion cells in muscularis propria [Myenteric/Aurbach plexus]; (F) IHC highlighting Ganglion cells in muscularis propria.
View Figure 2
Figure 2: (Proximal resected margin): (A) Normal colonic mucosa showing nerve innervations; (B) IHC highlighting mucosal nerve innervations; (C) Submucosa showing ganglion cells [Meissner's plexus]; (D) IHC highlighting Submucosa showing ganglion cells; (E) Ganglion cells in muscularis propria [Myenteric/Aurbach plexus]; (F) IHC highlighting Ganglion cells in muscularis propria.
View Figure 2
HD is classified according to the length of aganglionic section into short aganglionic segment (75-80%) [distal part of the sigmoid colon and rectum]; long aganglionic segment (10%) [rectum, sigmoid colon and colon up to the splenic flexure]; total colonic aganglionosis (5%) and ultra short segment HD [short in the anal canal] [2]. Hirschsprung’s disease in adults is usually a short or ultra-short aganglionic segment because it shows relatively mild symptoms. Surgical removal of the aganglionic segment of the gut is the definitive treatment for Hirschsprung’s disease [5].
Etiology of this condition shows a Complex genetic basis with at least 24 susceptibility genes; variable penetrance for most genetic alterations; combinatorial effects of low penetrance gene variants [6]. Most common symptoms of HD are chronic constipation, flatulence and emesis. Complications in undiagnosed cases of HD include acute enteritis, toxic mega colon, perforation and sepsis [7]. Parc, et al. [8]. said there is no HD that is revealed in adulthood, there is only HD ‘unknown’ until adulthood. As a definitive treatment is available, clinical suspicion of HD is of crucial importance.
Possibility of adult HD should be considered in patients presenting with chronic constipation or even acute intestinal obstruction, as curative surgical intervention is available to relieve symptoms and reduce further complications. Clinical suspicion and accurately performed biopsy with IHC are the key in the appropriate and timely diagnosis of HD.