Introduction: Cocaine is an addictive stimulant drug. In 2014, about 913,000 Americans met the Diagnostic and Statistical Manual of Mental Disorders criteria for dependence or abuse of cocaine. Approximately 69% of Cocaine has been contaminated with Levamisole. Levamisole has been found to be immunogenic causing anti-neutrophil cyto-plasmic antibody (ANCA)-associated cutaneous vasculitis in 88-100% patients.
Case presentation: 24-year-old male with a history of polysubstance abuse including IV drug abuse presented with complaints of bilateral lower limb weakness associated with burning pain and numbness in the right leg since the past 10 hours. His vitals were in the normal range. He had used cocaine one week prior to admission. Lab evaluation showed Na - 135 mmol/L, K - 5.6 mmol/L, creatinine - 2.85 mg/dl, elevated SGOT of 1351 U/L and SGPT 460 U/L, elevated WBC. Urine analysis showed pH 6.0, specific gravity 1.016, Hb 3+, RBC 14 and Protein 100. Urine toxicology was negative. Renal ultrasound was unremarkable. CPK levels (17,000) continued to trend downwards. Urine microscopy showed muddy brown cast. Serologies were negative for Hep B, Hep C, HIV. Immunology was negative including ANCA. C3, C4 were normal. Renal biopsy revealed vasculitis, patchy interstitial edema along with focal collections of interstitial eosinophils. He required hemodialysis and steroids.
Conclusion: Vasculitis in Cocaine abusers has often been attributed to Levamisole, an anti-helminthic added to cocaine to help enhance its euphoric effects. Levamisole induced ANCA positive vasculitis is well known. Our case is one of the few ANCA negative renal vasculitis responding to steroids.
Cocaine, Levamisole, Glomerulonephritis, Vasculitis, ANCA
ANCA: Anti-Neutrophil Cytoplasmic Antibody
Cocaine is a powerfully addictive stimulant drug. The purified chemical, cocaine hydrochloride was isolated from plants more than 100 years ago. Cocaine has been abused in many forms: The water-soluble hydrochloride salt and water-insoluble cocaine base. Users inject or snort the hydrochloride salt, which is a powder. According to the national institute of drug abuse, there were estimated 1.5 million current cocaine users aged 12 or older (0.6 percent of the population). In 2014, according to the NSDUH, about 913,000 Americans met the Diagnostic and Statistical Manual of Mental Disorders criteria for dependence or abuse of cocaine (in any form) [1]. Cocaine has been known to cause systemic effects like myocardial infarction; dissection, vascular thrombosis, rhabdomyolysis and renal complications include acute kidney injury, chronic kidney injury, malignant hypertension. Levamisole is an antiparasitic, which has been discontinued due to various side effects. Approximately 69% of Cocaine has been contaminated with Levamisole [2]. Clinical syndromes associated with Levimasole adulterated cocaine include agranulocytosis, leukocytoclastic vasculitis, and cocaine-induced vasculitis with pauci immune necrotizing glomerulonephritis. Levamisole has been found to be immunogenic causing anti-neutrophil cytoplasmic antibody (ANCA)-associated cutaneous vasculitis (AAV) in 88-100% patients [3]. However, here we present a case of ANCA-negative Levamisole adulterated cocaine induced isolated renal vasculitis.
A 24-year-old male with a history of polysubstance abuse including IV drug abuse presented with complaints of bilateral lower limb weakness associated with burning pain and numbness in the right leg making him unable to walk since the past 10 hours. He was asymptomatic up until the previous night and experienced sudden onset of the above symptoms, waking him up from sleep. On further inquiry he also endorsed difficulty in passing urine. On physical examination, his vitals were in the normal range with a Pulse of 74 beats/min, Blood pressure - 120/87 mm Hg and RR of 12/min. A blanching erythematous rash was noted in the area of the 9th left rib. Neurological examination was significant for weakness around the right hip and knee joints. He smoked 0.5 packs a day and consumed 3.0 oz of alcohol per week. He reported to having used Heroin, Cocaine, LSD, and Methamphetamines in the past with the most recent ingestion being cocaine one week prior to admission. There was no significant renal history in the family. He was on sublingual Buprenorphine until one month prior to presentation.
His initial labs were as in Table 1. Transaminases were elevated with SGOT of 1351 U/L and SGPT 460 U/L. CBC showed hemoglobin - 14.8 g/dl, WBC - 16.94-10 × 103/uL, PLT - 213 × 103/uL. Urine analysis showed a red colored urine with a pH 6.0, specific gravity 1.016, Hemoglobin 3+, WBC 0, RBC 14 and Protein 100. Urine toxicology screen was negative. Renal ultrasound was unremarkable with both kidneys measuring approximately 12.8 cm without any hydronephrosis. MRI of his spine was suggestive of mass effect suspicious for epidural abscess for which he underwent T8-10 laminectomy. However, epidural abscess was not found during surgery. He was started on IV fluids for AKI. He later developed swelling of the right lower extremity. Doppler studies did not show any vascular pathology. On day 3, he was tested for and found to have elevated CPK levels of 17,000 which continue to trend downwards. Urine microscopy done by nephrologist was suggestive of few muddy brown cast and occasional calcium oxalate crystals. In spite of the interventions his creatinine continued to trend upwards. Serologies were negative for Hepatitis B, Hepatitis C, HIV, ANA, ANCA, Centromere Ab, Ds-DNA Ab, Histone Ab, JO-1 Ab, RA factor, RNP auto antibody, SCL - 70, Smith, SSA, SSB auto antibody, PR3, MPO. C3, C4 were normal. Renal biopsy revealed singlebiopsy core of renal cortex and medulla containing up to 28 unremarkable glomeruli, features of renal vasculitis (focal in 1-2 arteries), mild acute tubular injury, patchy, interstitial edema along with focal collections of interstitial eosinophils. The renal biopsy however, failed to explain the severity of renal failure in the patient. His creatinine peaked to 19.0 with evidence of fluid overload after which he was started on Hemodialysis. While admitted to the hospital he required a total of 12 sessions of Hemodialysis. A provisional diagnosis of Cocaine (adulterated with Levamisole) induced vasculitis was considered and he was started on steroids for the same. He responded to steroids with improvement in renal function. 24 hour creatinine clearance test revealed a clearance of 44 ml/min done 3 days after stopping his hemodialysis. He was subsequently discharged home on oral steroids.
Table 1: Chemistry. View Table 1
There are several mechanisms by which Cocaine can cause acute kidney injury. These include Rhabdomyolysis, Vasculitis, Platelet activation, Prostaglandin pathways, Oxidative stress [4]. Rhabdomyolysis has been thought to be caused by direct toxicity of cocaine leading to acute skeletal myofibrillar degeneration, vasoconstriction leading to muscle ischemia and necrosis, seizure or hyperpyrexia [5]. In our case outlined above, the patient did admit to having used cocaine and the positive finding of elevated CPK levels which were responding to fluids showed a possible underlying rhabdomyolysis. Although his CPK levels normalized his creatinine continued to trend upwards triggering the need for a renal biopsy. The biopsy did not show any myoglobin deposits but did show some focal vasculitis (Figure 1). Vasculitis in Cocaine abusers has often been attributed to Levamisole. Levamisole was introduced as an anti-helminthic agent which was later withdrawn due to its side effects of liver toxicity, gastrointestinal distress, vasculitic purpura, necrosis of the ears, agranulocytosis and vasculitis. However incidences of Levamisole induced toxicity have been on the rise in cocaine users in the recent past. Levamisole has been added to cocaine to help enhance its euphoric effects. Levamisole increases the Dopamine D1 receptors and has a cholinergic action thus enhancing the effect of cocaine. With a half-life about 5.6 hours, testing for levamisole is quite challenging. Also, specific testing is not readily available at all centers [6]. This may explain a negative urine toxicology screen in our case. We believe that due to lack of any other precipitating factor and negative serologic testing, his renal disease was most likely caused by Levamisole adulterated cocaine (Figure 2).
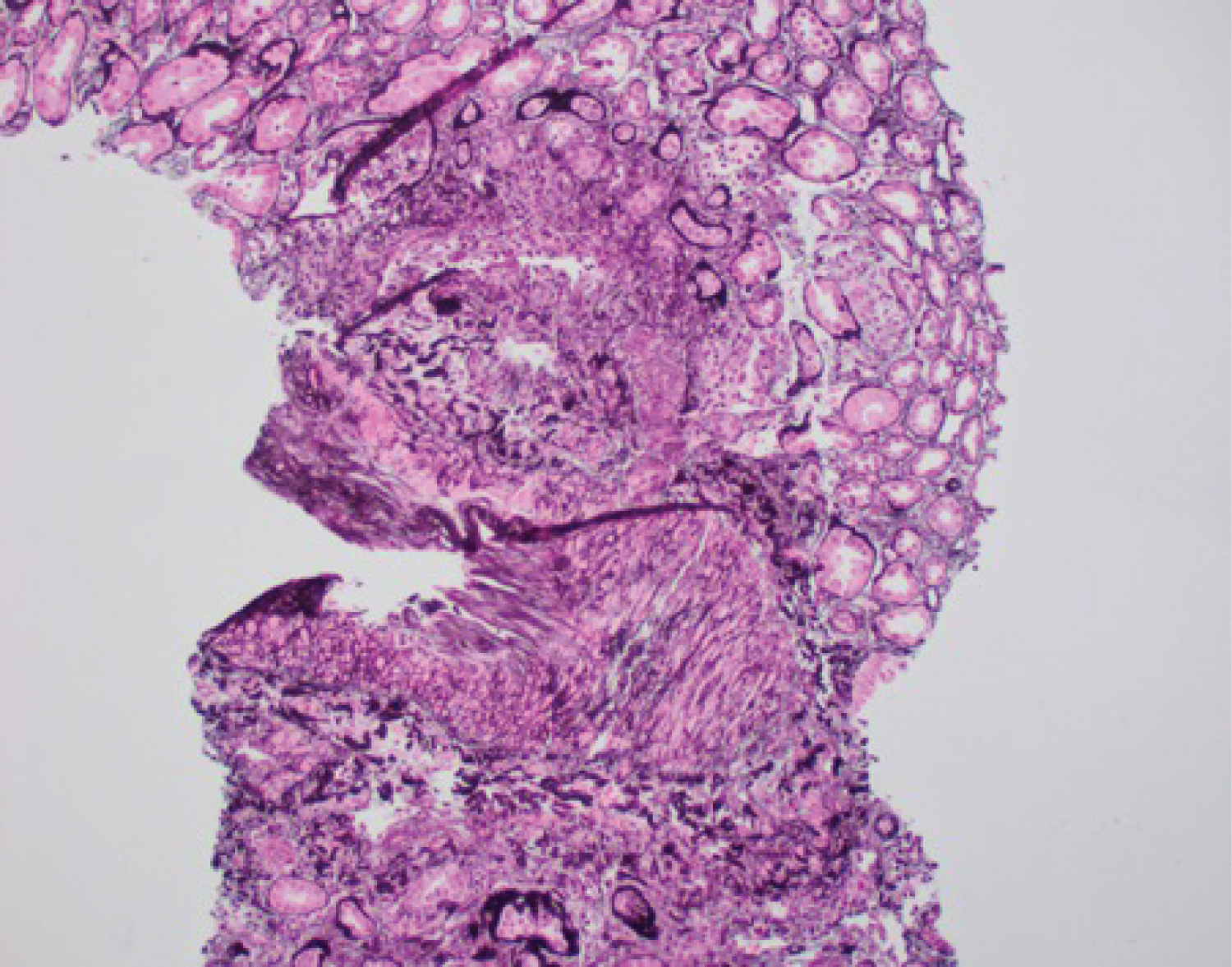 Figure 1: Renal Biopsy: Low-power view of a medium-sized artery, itself a branch of a nearby larger artery, showing inflammatory cells along its intima (Jones silver stain X 100).
View Figure 1
Figure 1: Renal Biopsy: Low-power view of a medium-sized artery, itself a branch of a nearby larger artery, showing inflammatory cells along its intima (Jones silver stain X 100).
View Figure 1
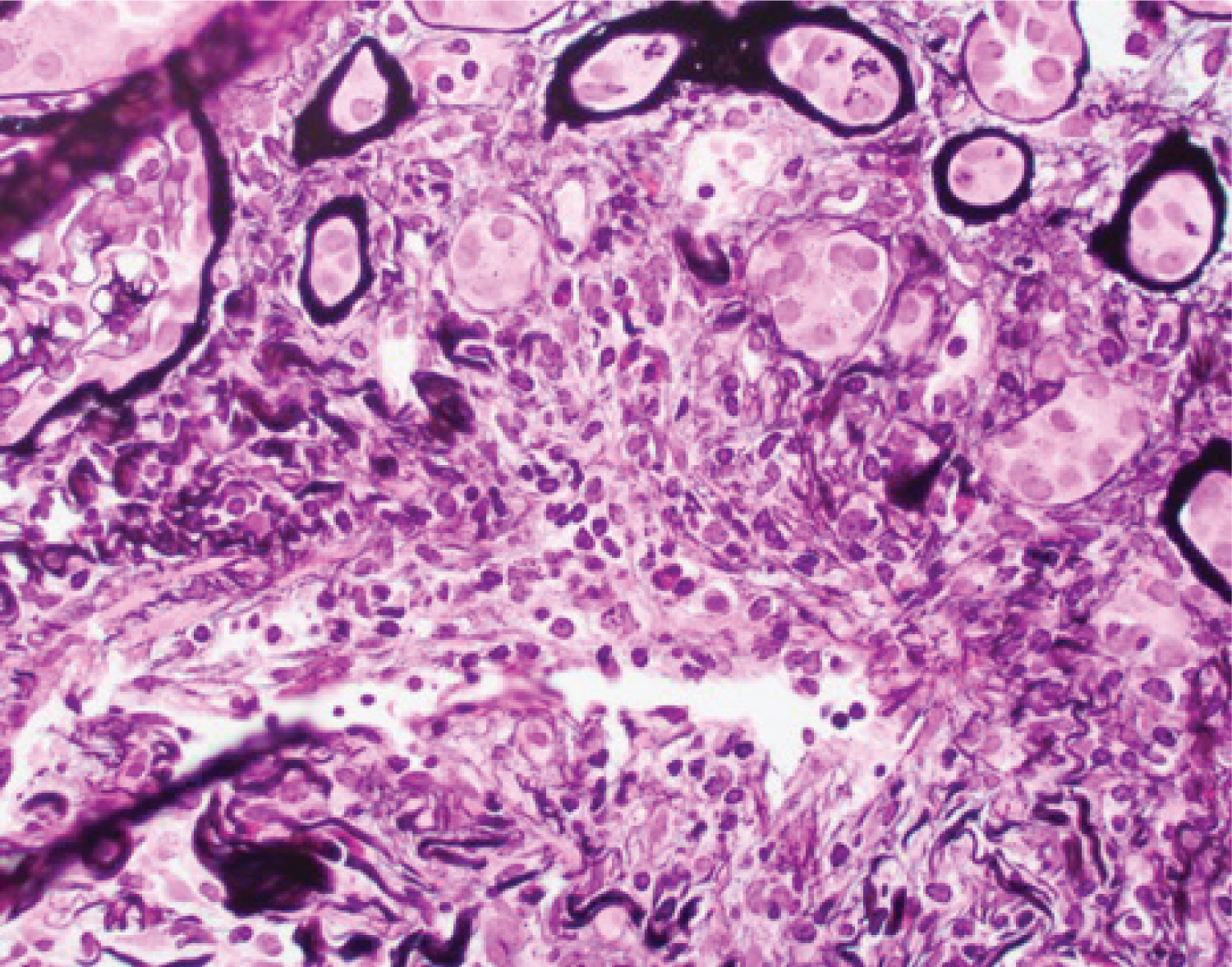 Figure 2: High-power view of the involved medium-sized artery showing lymphocytic infiltrate in its wall, which also shows partial disruption (Jones silver stain X 400).
View Figure 2
Figure 2: High-power view of the involved medium-sized artery showing lymphocytic infiltrate in its wall, which also shows partial disruption (Jones silver stain X 400).
View Figure 2
There have been several case reports of Levamisole induced ANCA positive vasculitis. However ANCA negative vasculitis has also recently been reported in the literature [7]. Our case is one of the few ANCA negative renal vasculitis responding to steroids. Our case was limited in the sense that the substance was not available for testing.
Cocaine induced kidney injury may have various different presentations and pathology and to define a particular approach to treatment is not always possible. Cocaine remains detectable in the urine up to 48 to 72 hours and while levamisole for only 5-6 hours which makes their diagnosis even more challenging. Thus a high level of suspicion with timely testing are required to detect these substances. The role of steroids in the treatment of this condition has not been established but this patient responded well to steroids likely due to presence of interstitial inflammation. Further research and studies are required to understand effective was to diagnosis and treatment this condition. Until then, the primary treatment continues to be cessation of drug use and renal replacement therapy if needed.