As one gets older, some changes occur in swallowing mechanisms. The non-symptomatic swallowing disorders associated with aging for no reason are called presbyphagia. Whether or not presbyphagia has any cause other than the mechanisms of aging is not clear. In our study, we investigated the association of presbyphagia with hypertension, diabetes, and obesity. Early detection of presbyphagia is important, and it is also important to reveal its association with common diseases encountered in society. Early diagnosis of the elderly presenting with presbyphagia who carry the risk for dysphagia is of big importance. For this geriatric population, we designed a study to establish the relationship among hypertension, obesity and diabetes mellitus with the prevalence of presbyphagia.
In study was conducted on elderly populations aged 65 and over who met exclusion criteria. To able to reach the number of sampling, "EAT-10 questionnaire", which also has a validation, was used to eliminate those with symptomatic swallowing disorders. The number of patients we reached was 320, but 7 dropped out the study and therefore the study was carried out with a total of 313 samplings (Reached as 97.8% (up 95% G-power)).
We used validated sEMG test in the quantitative (objective) detection of dysphagia limit and during subsequent water swallowing test of 20 ml. In this method, swallowing disorder was detected in 39 cases (12.4%) out of 313 cases. Of the 313 asymptomatic geriatric groups, (n = 39) asymptomatic swallowing disorders were detected. The population without swallowing disorder was n = 274. Of these, 71% (25.9%) was seen to be present with obesity, while (35.8%) had diabetes and 54.7% had hypertension.
Among the elderly group without symptoms, the prevalence of asymptomatic dysphagia, namely presbyphagia, was 12.4%. With a simple, non-invasive, inexpensive, yielding quantitative results in short time method, it is possible to screen the geriatric population with asymptomatic swallowing disorders. It may also be interesting to reveal its relationship with three common diseases in this group, apart from early precautions to be taken. There was no significant difference in the prevalence of diabetes between the group with and without swallowing disorder (p = 0.434). There was no significant difference in the prevalence of obesity between the groups with and without swallowing disorder (p = 0.190). Obesity and diabetes are closely related diseases and it was significant in terms of reliability that these groups gave similar results to those of asymptomatic dysphagia. We found a significant difference (p = 0.044) in terms of HT between the group detected to have asymptomatic swallowing disorder and the group which was not detected to have. The risk of dysphagia in elderly people with hypertension was 2.104 times higher compared to those without hypertension (OR = 2.104, p = 0.048, 95% GA = 1.007-4.397).
There could be a significant relationship between hypertension and dysphagia. It could be assumed that the presence of hypertension in the elderly may be associated with the swallowing disorder accompanied by asymptomatic dysphagia. We are also convinced that 2.1 times more hypertension encountered in those with asymptomatic dysphagia compared to those without could form the basis for further research on the subject.
Geriatrics, Asymptomatic dysphagia, Superficial EMG, Hypertension, Diabetes mellitus type 2 obesity, Presbyphagia
EAT: Eating Assesment Test; GERD: Gastroesophageal Reflux Disease; SEMG: Surface Electromyography; DL: Dysphagia Limit; CI: Confidence Interval; COPD: Chronic Obstructive Pulmonary Disease; HT: Hypertension; DM: Diabetes Mellitus
The elderly are at higher risk for swallowing disorder development. With aging, there can also be some changes in the swallowing mechanisms without organic disturbances. This is thought to be only due to the decreasing reserve in the aging organism. Frequently, this condition is defined as "presbyphagia" (decreased swallowing function). The person is asymptomatic at this stage and his/her presbyphagia or susceptibility to this condition could only be determined by special methods. However, these functional changes may not cause any swallowing problem in the healthy elderly at the beginning. However, increasing swallowing functions may lead to morbid complications such as aspiration, malnutrition, dehydration, etc. These situations in the elderly are already expected complications in the cases with swallowing disorder whose etiology is clear and the symptoms are evident. What is important at this stage is to detect the swallowing disorder which the sufferers are not aware of at an early stage. Swallowing is a complex sensorimotor. It involves both voluntary and involuntary movements within a defined time frame and on a regular basis.
Terminologically, dysphagia is a Greek-originated term referring to the difficulty in swallowing, which consists of the words "dys" (difficulty) and "phagia" (food). Dysphagia is a symptom which occurs when the passage of the food to stomach is mechanically blocked and is also the loss of coordination or strength in the muscles enabling swallowing movement. Dysphagia occurs in the oropharyngeal or esophageal phases of swallowing. All organic and physiological reasons affecting these two phases lead to dysphagia. Almost all of the symptomatic dysphagia etiologies can be revealed by specific test and imaging methods.
As for presbyphagia, this condition differs from dysphagia in that it involves a terminology where the findings of difficulty in swallowing are not obvious. It is a condition which remains often unrecognized until it becomes symptomatic, though it is common among the elderly. We designed this study with the assumption that revealing this condition would only be possible by screening all of the population aged 65 years and more, or by screening the elderly with some unrelated but often prevalent diseases encountered widely in the community. In general, these screening tools are heterogeneous and there is no common consensus around the world on which method provides the best or most accurate result. Important factors to consider when choosing a screening tool can be counted as the quality of the study, the validity of the tool and the reliability, cost-effectiveness, and feasibility of the management of the tool [1-4]. Various scanning and diagnostic tools were compared in Table 1.
Table 1: Approved screening tools. View Table 1
Along with age-related diseases, age-related changes in swallowing physiology are predisposing factors for dysphagia in the elderly. Dysphagia affects 300,000-600,000 people per year [5]. Conservative estimates suggest that an average of 15% of the elderly population is affected by dysphagia, though the exact prevalence of dysphagia is unclear in different publications, as previously reported [6]. The impact of the condition on morbidity, length of hospital stay and healthcare costs among hospitalized elderly is higher than 51%. In some studies, this ratio varies between 15% and 22% [6-8]. When we look at the other etiologies in relation to advanced age and dysphagia, the symptoms and signs of dysphagia can be seen among the elderly patients who have anatomical or physiological defects in their mouth, pharynx, and larynx [9,10]. On-going studies on swallowing in healthy elderly individuals in relation to dysphagia and advanced age are still emphasizing the lack of studies on the effects of aging on swallowing mechanism and function. With the increasing neurophysiological studies in recent years, research in this area has gained momentum and it has been understood that dysphagia is an important health problem among the elderly [11]. However, investigating the likelihood that this condition might be more frequent in some patients may bring an advantage in primary screening these groups. In fact, it is important to investigate the relationship of this disease (or these diseases) with swallowing disorder and thus with susceptibility to dysphagia.
This is a method used as eating (swallowing) assessment questionnaire that gives symptom-specific results. The normative data lead us to think that the scores found like 3 or higher following EAT-10 test are abnormal, suggesting the person has a swallowing problem. In short, this test can be used to document the severity of dysphagia and monitor the response to the treatment in those with a wide spectrum of swallowing disorders. The EAT-10 swallowing questionnaire, which has been proven to have excellent internal consistency, test reproducibility and criteria-based validity in overt dysphagia screening, can be used as a preliminary tool to screen swallowing disorder [3,12-14].
The dysphagia assessment method according to submental muscle group in swallowing assessment is called submental electromyography (smEMG) or surface electromyography (sEMG) with reference to the muscle group where superficial electrodes are affixed [15-21]. It would be reasonable to assess the role of submental muscles in swallowing in this way when we think of the decreasing reserves of all functions with aging in presbyphagia (Figure 1).
 Figure 1: Measurement locations and application method of electrodes for dysphagia evaluation (Adapted from; [49]).
View Figure 1
Figure 1: Measurement locations and application method of electrodes for dysphagia evaluation (Adapted from; [49]).
View Figure 1
Another criterion that supports and recognizes practically a patient suspected of dysphagia is Dysphagia Limit (DL) 22-29]. Dysphagia Limit defines the "swallowing action" known as "piecemeal deglutition". One can determine the amount of water that makes swallowing harder during swallowing event. However, while a healthy person is expected to swallow a quantity of water around 20 mL at once, it is pathological that a person with impaired swallowing needs to swallow the same water in two or more portions dividing. The asymptomatic swallowing which the person cannot recognize by him/herself can be detected and recorded as an EMG in an objectively (Figure 2).
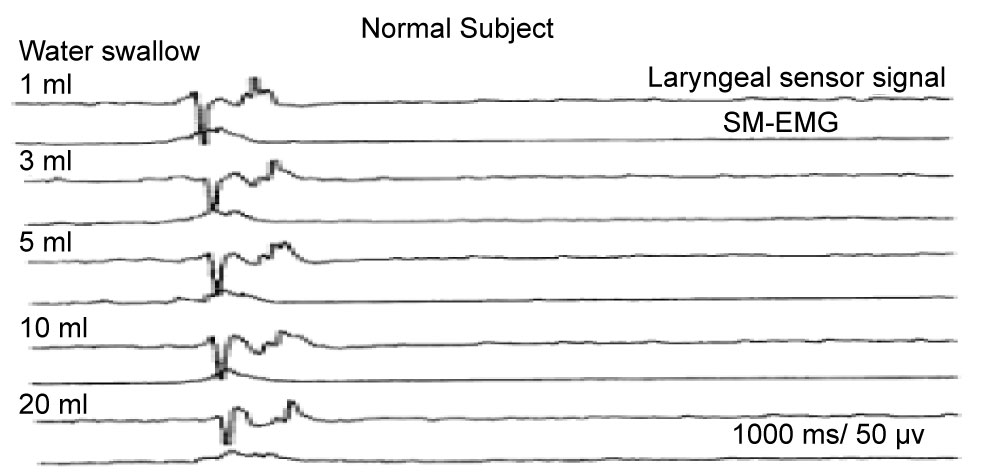 Figure 2: Normal water swallowing model in semg [20].
View Figure 2
Figure 2: Normal water swallowing model in semg [20].
View Figure 2
The research, was conducted with the voluntary participation of the elderly patients at the age of 65 and over who had applied to our hospital as well as with the voluntary patient companions of the patients hospitalized in internal medicine clinic who were at the age of 65 or more. Our preliminary study found that the smallest sample size to be reached at the 95% confidence interval (CI) with a 5% error was 320 (G-power).
It was proven that the volunteers aged 65 or more who were found to be eligible for the study criteria of being without any swallowing complain were seen to be asymptomatic through the EAT-10 test, thus we reached 313 cases, showing that we were close to the previously intended number of cases in our preliminary study with 97.6% at our disposal (313/320). In order to detect the presbyphagia rate of this population (those with asymptomatic dysphagia), water at amounts of 3,5,10,15 and 20 ml were made to be swallowed by each of these patients and sEMG recordings were taken. The osmyographic recordings of swallowing activity were quantitatively recorded in sEMG as 3, 5, 10, 15, 20 ml of water were respectively swallowed by each case in a total of N = 313 cases. The volume of water at the time of oscillographic recording when piecemeal deglutition was observed was recorded as the patient's DL (Dysphagia Limit) and the case was enlisted in asymptomatic dysphagia group. Water at amounts of 3, 5, 10, 15, 20 ml was prepared in advance for each patient separately.
In the study, Nihon Kohden Neuropack S1 model 2 channel EMG device was used for swallowing and respiration recording. One channel was used to record muscle activity related to swallowing, and the other channel was used to intranasally record the respiratory function of swallowing.
To get EMG recording from submental muscle, a cup electrode with two touch-proof connectors, having a recorder with silver/silver chloride metal end, about 1.5 meters long was placed to the first channel. The active (-pole) electrode was mounted on right submental muscle, while the reference (+pole) was placed on left submental muscle using paste. A breath sensor branded as Sleep Sense (Item = 14830 SN = 1247394013) was fitted to the second channel. A systematic disposable nasal cannula was mounted to the air inlet of the respiratory sensor. The nasal cannula was placed in both nostrils of patients and controls and was instructed to breathe only through the nose during the examination. We took great care to make the observations at normal room temperature. To record superficial muscle activity in the sEMG device, the device settings of the first channel were made as follows: High pass filter - 5 kHz, low pass filter - 10 Hz, display sensitivity 50 microvolts. The settings of the second channel for breathing sensor recording were as follows: High pass filter-50 Hz, low pass filter-0.2 Hz, display sensitivity 500 microvolts. Due to the technical nature and limitations of the EMG device, the screening recording time was set to 1 second. Apart from this, the patient's earthing was done using a cup electrode with a touch-proof connection, about 1.5 meters in length, having a recorder with an end made of silver/silver chloride metal.
The study was completed in 11 months with the preparation of such conditions and equipment as non-allergic adhesive tapes, preparation of 2-way sEMG silver electrodes with sterilization liquid for every patient, hydrophilic cotton, laptop computer for recordings, sEMG device (NIHON KOHDEN), 2-way electrode and silver probes, providing examination table to allow the patient sit upright position comfortably, printers, the gloves for the sEMG practitioner and providing the person who assisted in redesigning these conditions (me) for each case group within a scheduled calendar time (I). Our elderly subject was instructed to place his head in a way that his body would be neutral and in an upright position on the examination table. For SEMG activity, bipolar silver chloride consisting of a piezoelectric aperture was banned under the jaw in the direction of the submental muscle complex with the EMG electrodes (in the direction of the submental muscle contracted during swallowing through palpation). The signal was passed from the tape, filtered and made ready for operation. Individuals were asked to swallow the water in increasing volumes each time as 3-5-10-15-20 ml with the command "swallow". The elderly were asked to swallow the whole liquid in one single pass, and the curves at the time of swallowing were seen on the screen and recorded and printed out. This was done by taking the methods in the literature as an example (60). Those who were observed to exhibit more than one-divided-swallows, namely piecemeal deglutition, and/or coughing reflexes were considered dysphagia. The water volume where piecemeal deglutition was observed more than once formed the dysphagia Limit (DL) of the person. Swallowing time and synchronized apnea times in the dysphagia limit (piecemeal deglutition sample) were recorded. Using a nasal cannula, the respiratory sensor connected to the 2-channel EMG (Nihon Kohden) device with an electrode cable simultaneously measured and recorded respiratory function (duration of apnea) and swallowing time during the swallowing activity (Figure 3).
 Figure 3: sEMG recording device.
View Figure 3
Figure 3: sEMG recording device.
View Figure 3
As a result, the data were obtained from 313 patients who were reached with the help of a specialist neurologist in a total of 11 months. The data were evaluated instantaneously through sEMG and 39 patients were diagnosed with asymptomatic swallowing disorder (presbyphagia).
1) Criteria for inclusion in the study:
• Those over 65 years of age
• 65 or over people who meet their mental and physical needs themselves
• To become volunteer
• Not having the exclusion criteria
• Those with negative dysphagia test score less than 3 in EAT 10 questionnaire.
2) Criteria for the exclusion in the study:
• To be bedridden or dependent on others
• To have pulmonary disease including COPD
• To be mentally and physically dependent
• To be previously diagnosed with dysphagia
• Those with a disease that can cause oropharyngeal dysphagia (those undergoing head and neck surgery).
• To have any causes of esophageal dysphagia
• To have Infection conditions, including upper and lower respiratory tract infections, which may affect swallowing functions during work
• To have cerebrovascular and neurological diseases (Parkinson, stroke, all types of stroke, myasthenia gravis, dementia,)
• To have At least one diagnosis (gastritis, ulcer, reflux, polyp, hemorrhage, malignancy, achalasia) from the stomach and foodborne diseases by invasive or non-invasive methods by a gastroenterologist
• To have uninvestigated dry eye syndrome and/or sjögren diagnosis
• To have applicants to oral and dental health policlinics within the last 6 months
• Patients with dysphagia at the end of the questionnaire, the validated dysphagia screening tool EAT 10 (EAT 10 score 3 and higher than 3)
• Exposure to one or more of the above exclusion criteria when participating in the study
• Lymphoma disease, Hepatitis C Viral infection
• Smokers
• Those under 65 were considered as ineligible for the study.
Definitions for examining the effects of some demographic records of those enrolled in the study are as follows:
• Age: Those 65 and over assessed according to inclusion and exclusion criteria. The birth date of the individual on his/her ID was recorded.
• Gender: All elderly volunteers who presented irrespective of sex.
• Diabetes Mellitus type 2 presence: The cases diagnosed by a physician and followed continuously by a physician were also enrolled in the study.
• Presence of hypertension : The cases diagnosed by a physician and presenting tension values within the desired limits of Turkish Hypertension Guideline with or without medication under continuous physician follow-up were also enrolled in the study.
• Body mass index: The BMI of the subjects was obtained by dividing the weight (kg) to the neck (m2). The relationship between dysphagia and malnutrition was evaluated under the heading of General Information. BMI < 18.5 kg/m2 was evaluated as severe malnutrition, 18.5-19.9 kg/m2 moderate malnutrition, 20-22 kg/m2 at malnutrition risk, 22-27 kg/m2 normal weight, 27-30 kg/m2 was evaluated as overweight and obese. Those over 30 kg/m2 also participated in the study and recorded in demographic information.
Data were collected from healthy elderly patients who admitted to the clinic who were eligible for the inclusion criteria of the EAT 10 questionnaire created in accordance with the variables through a face-to-face interview method. The data were collected between May 2016 and June 2017.
The study is a cohort/cross-sectional study. The data were analyzed with the SPSS 22.0 demo program. We used Chi-square in univariate analyzes in causal findings, Shapiro Whilk test in the distribution of the date between two independent groups, Mann Whitney test in determining whether or not there was the difference and Logistic Regression Analysis in multivariate analyses.In Logistic Regression Analysis model, univariate variables with a significant relationship with dysphagia were obtained.
Age: 65-75, 75-85 and 85 years or over (Reference Group 65-75 group)
Gender, Female, Male (Reference Group Male) Hypertension, Yes, No (No Reference Group)
Diabetes Mellitus Yes, No (No reference group) Significance level was accepted as p < 0.05.
The ethics committee approval of the study was obtained from the Bozyaka Training and Research Hospital Ethics Committee of Clinical Investigations of İzmir Bozyaka Education and Research Hospital of Health Sciences University in December 2016.
In terms of gender and dysphagia relationship, 151 (48.2%) of the 313 participants were female, 162 (51.8%) were male, and of the cases detected to have dysphagia in water swallowing test and sEMG (asymptomatic), 13.2% was female (n = 20), while 11.7% (n = 19) was male. The related findings are presented in Table 2. There was no significant difference between the groups with (n = 39) and without (n = 274) dysphagia (p = 0.685).
Table 2: Gender distribution of participants and gender-dysphagia relation. View Table 2
When we look at the relationship between diabetes and dysphagia; Of the 274 patients without dysphagia, 98 patients (35.8%) were present with diabetes mellitus, while 176 (64.2%) had no diabetes diagnosis. 17 (43.6%) of the group with dysphagia were detected to have diabetes, while diabetes was present in 98 patients in the group without dysphagia. There was no significant difference in the presence of diabetes between the two groups (p = 0.434). In Table 3, the results of the relationship between the group with and without dysphagia are presented.
Table 3: Relationship between dysphagia and diabetes. View Table 3
When we look at the hypertension-dysphagia relationship, there were 150 patients (54.7%) with hypertension diagnosis, while 124 patients (45.3%) with no HT diagnosis out of 274 patients without dysphagia. In the group with 39 dysphagia diagnosis, hypertension (HT) was diagnosed in 28 patients (71.8%), while 11 patients (28.2%) had no hypertension. There is a significant difference between the group which was detected to have dysphagia and the group which was not in terms of the presence of HT (p = 0.044). Table 4 presents the results of the relationship of hypertension with the group which was detected to have dysphagia and the group which was not.
Table 4: Relationship between dysphagia and hypertension. View Table 4
On the other hand, when looked in terms of obesity and dysphagia relationship, out of the 274 patients without dysphagia, obesity was found in 71 patients (25.9%) There was no obesity in 203 people (74.1%). Of the 39 patients who had dysphagia, 25 (64.1%) patients had no obesity, while 14 (35.9%) had the disorder (Table 5). There was no significant difference between the group with dysphagia and the group without dysphagia in terms of obesity (p = 0.190). The results of the relationship between the group which had dysphagia and which did not have with obesity were shown.
Table 5: Relationship between dysphagia and obesity. View Table 5
There could be a significant relationship between hypertension and dysphagia. It could be assumed that the presence of hypertension in the elderly may be associated with the swallowing disorder accompanied by asymptomatic dysphagia (Presbyphagia). We are also convinced that 2.1 times more hypertension encountered in those with asymptomatic dysphagia compared to those without could form the basis for further research on the subject (Table 6).
Table 6: Effect of sociodemographic and chronic disease variables on risk of dysphagia in all group- logistic regression analysis results. View Table 6
In our study, we utilized sEMG, which is a simple, inexpensive, reliable, non-invasive and fast-result-giving screening device in the elderly with no dysphagia complaint about screening or diagnosing for asymptomatic (latent) dysphagia together with water swallowing test. There is a study in literature conducted with 81 patients and the sensitivity of dysphagia was seen to have been determined at 96% and specificity at 69% using EMG method in that study. Most of these cases are neurogenic dysphagia cases [30]. The most comprehensive study on the subject was reported by Suiter and Leder (2008) on 3000 participants. In this study, it was also shown that EMG had a sensitivity of 96% and specificity of 46% in the diagnosis of dysphagia [31].
Another example that shows great specificity and sensitivity is the study with a sensitivity and specificity of 86% 32-35]. The data obtained in dysphagia diagnosis with sEMG were obtained by single or sequential water swallowing test in various volumes. Water swallowing tests are quite popular with the EMG method as they basically do not pose any major risk for patients due to their noninvasive nature. We can say that this test is comfortable enough to use in the clinical setting because it is easily applicable and reproducible. Details of the patient selection, position, sEMG device used and results, dysphagia and normal sEMG samples were detailedly shared above in the material and method section. In our study, we used sEMG method with sequential water swallowing test in the evaluation of dysphagia diagnosis and treatment results by giving reference from the studies of Ertekin C, et al. who has numerous studies on this subject. It can be seen that most studies have frequently made use of SEMG method, which directly assesses the swallowing-related function of a person performing swallowing 500 times a day and which can also objectively demonstrate oropharyngeal dysphagia [15,16,25,36-41]. It seems that sEMG method has empirical and clinical benefits in the analysis aiming towards detecting dysphagia and also has the quality to have acceptable accuracy and reliability in the determination of swallowing difficulties, at least when based on valid and reliable data. We used this method in our study to evaluate the screening and treatment results as it was methodologically quite consistent with the previous studies [42,43]. 313 elderly volunteers at the age of 65 and over were enrolled into our study irrespective of their genders At the end of the study, we found the prevalence of asymptomatic dysphagia in the elderly as 12.4%. This result was close to the ones reported by Okamoto, et al. who reported it to be 15.1% [44]. We could not find a study on asymptomatic (presbyphagic) conditions in the elderly in which we could compare this ratio with our elderly population of 65 years and over who had no overt dysphagia. Asymptomatic dysphagia may, in fact, be considered as a major geriatric syndrome associated with depressive disorders with its high prevalence in the elderly population [45]. Only a few epidemiological studies have documented dysphagia prevalence in asymptomatic elderly, with the exception of dysphagia prevalence related to pathological reasons [46]. Inui A, et al. found the prevalence of dysphagia in males as 17.8% and 21.9% in females (a total of 109 elderly without gender discrimination). Consistent with this study in which there is no difference detected between genders in terms of dysphagia prevalence, we found that 13.2% of female participants had asymptomatic dysphagia, while 11.7% of male participants had the condition and there was no significant difference between the groups (p = 0.685). Inui A, et al. cross-sectional study was designed to investigate the relationship between oral conditions and dysphagia. The dysphagia evaluation process went on with an objective assessment of dysphagia using repeated saliva swallowing test.
However, in this study, they featured the saliva swallowing test as a distinctive test for "certain impaired swallowing activities" (oral, pharyngeal residues, ruptured tears and impaired lip closure), but stressed the limitation in their study as they did not perform EAT-10 test. However, we specifically excluded symptomatic dysphagia with the EAT-10 test in our target age group (65 and older) and involved the elderly without symptomatic dysphagia into the study. In the study of Inui, et al., when the patient could not swallow his/her saliva three times consecutively with him/herself (saliva swallowing test), s/he was considered to have dysphagia and they also concluded that the risk of dysphagia-related aspiration might be higher in these persons. We came to this assumption seeing the objective and reproducible results of the sequential water swallowing test in our study, Inui, et al. detected the dysphagia prevalence as 40% for 70-75 age group and as 41.4% for the 75-79 age group. In our study, we found that the prevalence of dysphagia was similar in all age groups over 65 years old, and concluded that being at the age of 65 and over is enough to be considered at risk for dysphagia. There was no significant difference in gender distribution between dysphagia group (n = 39) and non-dysphagia group (n = 274) (p = 0.685). Gender was not a specific factor for dysphagia. We found parallel with similar values in the literature that there was no significant difference in gender distribution (17.8% male, 21.9% female) in elderly dysphagia cases. It was enough for us when the person demonstrated piecemeal deglutition more than once. Determination of the number of swallowing DL was sufficient to diagnose dysphagia, and determining the number of multiple-swallowings was not taken into account as it would not contribute to our study. The dysphagia limit (DL) is an objective measure of dysphagia. DL evaluates a precise physiological phenomenon and can be objectively quantified for this reason. There are numerous studies in which the oropharyngeal dysphagia detected within the dysphagia limit is objectively displayed and DL is measured and dysphagia is assessed [47,48]. Detecting at which DL there was dysphagia through sequential water swallowing test in sEMG formed the basic method for us to repeat the test at this piecemeal deglutition limit. Among the 274 normal subjects without dysphagia, diabetes was present in 98 patients (35.8%) and 176 patients (64.2%) were not diabetic. There was no significant difference between dysphagia and non-dysphagia groups (p = 0.434). Based on this, it can be said that there is no direct relationship between diabetes and dysphagia. Whether DM has any direct effect on oropharyngeal swallowing has not been discussed in the literature, but there are numerous studies investigating the relationship of DM with dysphagia caused by reasons not related to swallowing, including diabetic neuropathy in esophageal dysphagia. However, we did not encounter a study on diabetic dysphagic elderly associated with oropharyngeal swallowing or oropharyngeal dysphagia. There are a number of studies on the mechanism of action. Because our study is a study on oropharyngeal swallowing, asymptomatic dysphagia, and oropharyngeal dysphagia, we did not resort to the comparison between the ones written in the literature on esophageal dysphagia or caused by other reasons and diabetes. Of the 274 patients without dysphagia, 150 patients (54.7%) had HT diagnosis, whereas 124 patients (45.3%) had no HT diagnosis. We found a significant relationship between HT and dysphagia. (When assessed in terms of the presence of hypertension, those with hypertension are 2.104 times at greater risk of dysphagia than those without, which significantly increases the risk (OR = 2.104, p = 0.048, 95% GA = 1.007-4.397)) There was a significant difference between dysphagia and non-dysphagia groups in terms of HT presence (p = 0.044). Dysphagia was detected 2.1 times more frequent in hypertensive elderly. It is known that hypertension is not a factor causing oral dysphagia. The blood pressures of the patients who participated in our study were regulated through various antihypertensives. There is a need for further study on what sort of relationship this is. Of the 274 patients without dysphagia, 71 patients (25.9%) had obesity, while 203 patients (74.1%) had no obesity. There was no significant difference between dysphagia and non-dysphagia groups in terms of obesity (p = 0.190).
In our study, we came to the conclusion that hypertension could pose a risk for in the elderly. Hypertension may be an important risk factor in elderly patients who are asymptomatic in terms of swallowing disorder. It can be suggested that asymptomatic swallowing disorder (presbyphagia) screening should be primarily considered in hypertensive elderly in the geriatric group. Screening should be initiated for early diagnosis and treatment with the age of 65. Hypertensive patients aged 65 years and over can undergo a water swallow test with direct EMG without applying a preliminary questionnaire and asymptomatic swallowing disorder screening and diagnostic modalities can be performed. Since swallowing disorder prevalence does not show distributional variations among elderly age groups, it is recommended that swallowing disorder screening explained in this study should be performed at any age starting from the age of 65 years and over. In view of these additional outcomes, it is thought that by performing cost analysis, which is referred in the literature but not constituting a part of our study, possible complications of swallowing disorder may be reduced to a minimum even before emerging with early diagnosis. It was also revealed that diabetes and obesity are not statistically related to asymptomatic swallowing disorder. However, it was found that the presence of diabetes in the elderly could 1.4 times increase the risk of swallowing disorder compared to those without swallowing disorder, this may be worth investigating in larger geriatric populations.
Ethics approval and consent to participate: The ethics committee approval of the study was obtained from the Ethics Committee of Clinical Investigations of İzmir Bozyaka Education and Research Hospital of Health Sciences University. The authors declare that they have no conflict of interest. Inform consent was obtained from all participants.
Consent for publication: Not applicable.
Availability of data and materials: All data generated or analysed during this study are included in this published article.
Competing interest: The authors declare that they have no competing interests.
Funding: Not applicable.
Authors contributions: AY contributed to the interpretation of data and to the writing of the manuscript. FA is a sinyor author. AK and YÖÜ are executive persons in the study and in the EMG laboratory process. RRB is the consultant doctor. HU analyzed the data. MNY contributed to the create the population of the study. All authors read and approved the final manuscript.