The purpose of this project was to conduct pharmacotherapeutic management of patients in the outpatient setting in a standardized manner. A CMR program was implemented at select ambulatory care sites within our healthcare system. This review identified and addressed medication-related concerns in order to optimize disease state management and attain positive patient outcomes.
This prospective review included patients 80 years or older with polypharmacy concerns, categorized as having greater than 10 medications. Evaluation assessed for therapeutic duplications, potential interactions, side effects, inappropriate medications in the elderly, pharmacoeconomic issues and adherence concerns. All data was collected through the outpatient electronic health record. The primary outcome was the number and type of interventions identified through CMR. Secondary outcomes included percent of recommendations accepted, reasons for rejection, types of recommendations, and disease states intervened on.
Out of a total of 222 patients, 52 patients did not require any interventions and 250 recommendations were made to the providers on the 170 remaining patients. Currently 82% of recommendations were accepted by providers, with 17% still pending provider acknowledgement, and 1% being rejected. A large majority, 141 recommendations, were made in regards to high risk medications.
CMR was shown to be highly effective in identifying appropriate medication interventions in order to optimize patient care. This study provided the framework to move pharmacists into other outpatient sites in the healthcare setting to assist in targeting inappropriate prescribing in the elderly.
CMR, Ambulatory care, Comprehensive medication management review, Beer's criteria, Polypharmacy
CMR: Comprehensive Medication Management Review
Polypharmacy is an increasingly important issue facing the healthcare system as the baby boomer generation begins to age [1]. While polypharmacy is not universally defined by a specific number of concurrent medications, in order to make the definition operational for research and possible interventions by pharmacists a variety of totals have been proposed based on practice setting. In a clinical setting polypharmacy can be defined as patients taking any medications that are not medically necessary. This can include medications not being used effectively or those that are therapeutic duplications among others [2]. The problem is more pronounced in the elderly due to multiple comorbidities which the patient needs to take several concomitant medicationsin order to treat it effectively. Kantor and colleagues demonstrated that through NHANES (the National Health and Nutrition Examination Survey) 39% of adults aged greater than 65 reported polypharmacy, defined as using greater than 5 medications, which was a 15% increase from 2000 to 2012 data [3]. Polypharmacy is a global issue that has led to the creation of different forms of interventions in order to provide a possible solution.
The Beers criteria and STOPP/START screening tool are available to assess the current medications for the elderly. The former focuses on drugs inappropriate for the treatment of medical conditions in the elderly [4]. STOPP/START criteria first looks at medications that should be potentially stopped in elderly patients and then subsequently medications that could be beneficial for the patient but are missing from their profile due to the fear of polypharmacy [5]. Comprehensive medication review (CMR) is a service offered to patients in order to optimize their medication regimens to help prevent potential adverse drug reactions and improve their overall disease management [5]. Several studies have been published looking at the perception of CMR for both patients and providers alike which indicate an overall positive reaction to the services when available [5-7]. While CMR services are well received, there have only been a handful of studies looking at the effectiveness of the programs on elderly patient outcomes [8-12]. There is still a need for more focused studies evaluating a standardized CMR and how they affect the overall health goals particularly in the elderly population.
This was a non-randomized prospective study. Data was collected through the outpatient electronic health record and through pharmacist direct documentation on a data collection sheet for further analysis. Data was collected from October 2018 through December 2018. The study was approved by the investigation review board. The study site is a community health system with 31 affiliate outpatient practices with integrated pharmacy service present at 11 of these sites. Patients were included in the study if they were 80 years of age or older and were taking greater than or equal to 10 medications. Patients were excluded from the study if they were deceased before interventions could be recommended or if the patient was on hospice. CMR was performed for each patient and assessed several different categories including: Therapeutic duplications, potential interactions, side effects, inappropriate medications in the elderly, pharmacoeconomic issues, and adherence. Pharmacists documented on a provided template whether an intervention was required and the outcome of this intervention if applicable. Additionally, patient demographics such as age, gender and renal function were collected. The primary endpoint was thenumber of interventions identified through the CMR service. Secondary endpoints included the percentage of recommendations accepted, the reason for rejection of recommendations when applicable, the types of recommendations made based on previously stated categories, and the disease states in which medication interventions were made.
A total of 222 patients met inclusion criteria and were evaluated through the CMR process. The average age of the study population was 89.3 ± 3.44 years. There were 152 females who participated in the study. The patients were taking on average 14.97 ± 5.3 medications. Interventions were not required on 52 of the patients. Of the remaining patients, a total of 250 interventions were communicated to providers. A total of 82% of recommendations were accepted by providers, with 17% still pending provider response, and 1% being rejected by the provider. Reasons for rejection included "intractable insomnia", "side effect not believed to be caused by medication", and "only medication that has been helpful for patient after failure of other recommended therapies". The distribution of the types of interventions recommended to providers can be seen in Figure 1. Additionally, the specific disease states that were involved in the interventions can be observed in Figure 2.
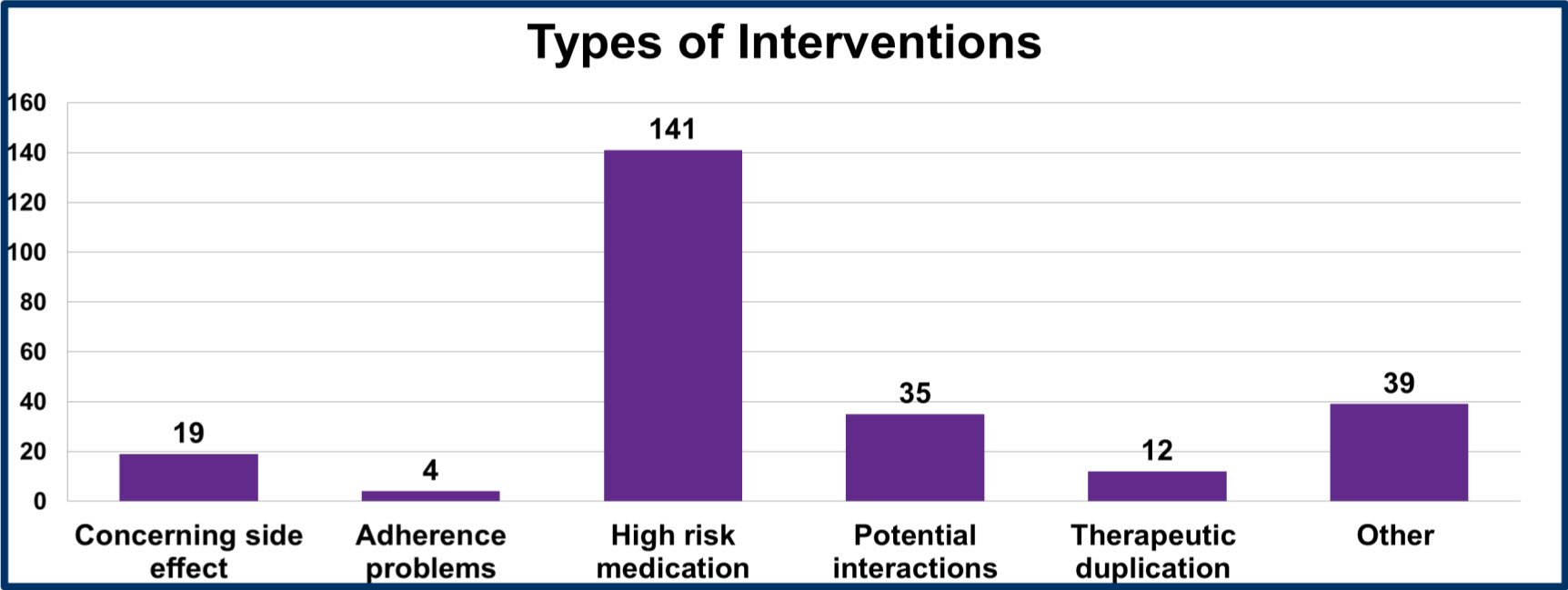 Figure 1: Types of Interventions.
View Figure 1
Figure 1: Types of Interventions.
View Figure 1
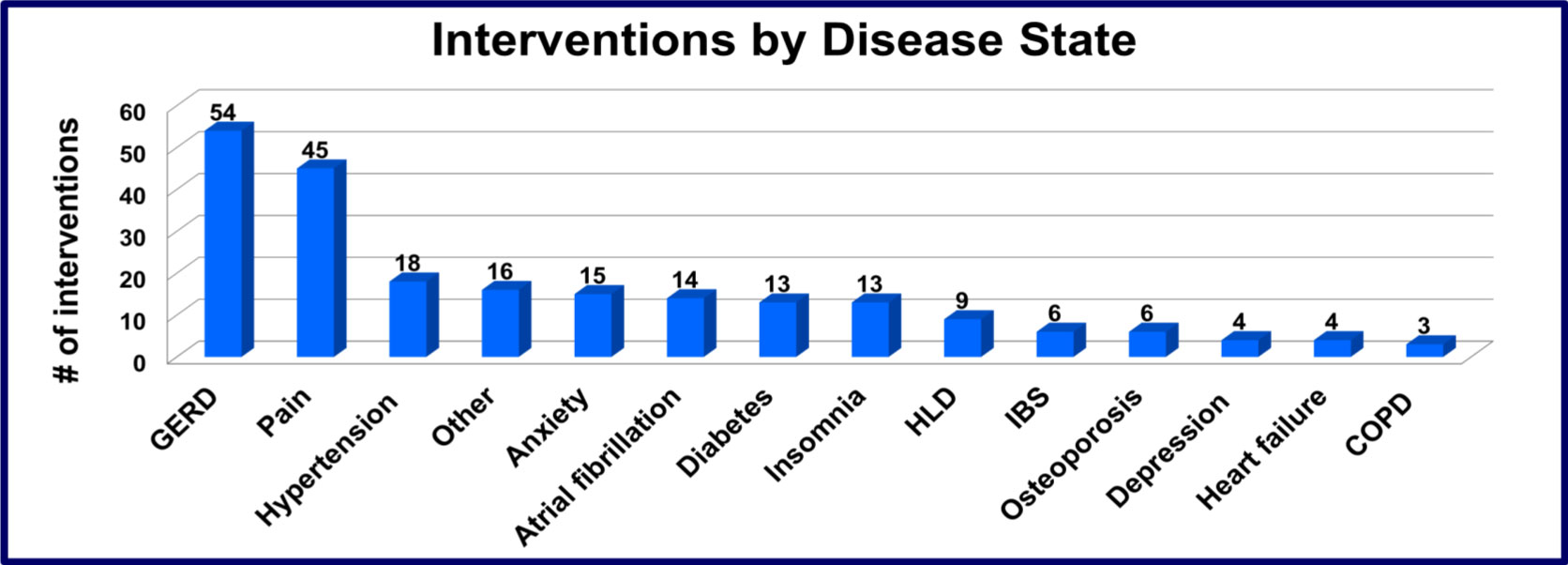 Figure 2: Interventions by Disease State.
View Figure 2
Figure 2: Interventions by Disease State.
View Figure 2
Pharmacy resident driven CMR service identified numerous medication interventions. Currently, 82% of the recommendations were addressed and accepted by providers. Only 1% of the recommendations were rejected, while 17% of the recommendations were still pending review. As shown by the acceptance versus rejection rate, providers positively took recommendations through the CMR process.
A majority of the interventions targeted high risk medications resulting in concern for falls and other adverse events in the elderly. The Beers Criteria provided a comprehensive list of medications that were inappropriate for use in our geriatric populations and set a tangible target when performing CMR. Proton Pump Inhibitors comprised the largest portion of the recommendations at 21.6%. This is further evidence of the use of continuous therapy with PPIs in patients who medically no longer require therapy. After prolonged therapy many of these patients cannot tolerate cessation due to rebound gastric reflux causing our geriatrics population to be exposed to the long term effects of PPI use. The second largest disease state intervention group was based on pain management, generally in relation to the use of opioids. Many providers did not make attempts to maximize the effects of acetaminophen by scheduling dosing rather than having patients use it on an as needed basis.
The main reasons for rejections of pharmacy interventions were based on disease states that were non-responsive to other therapies. This was evident mainly for patients who were experiencing insomnia. There are not many available geriatric safe therapies for the treatment of insomnia and behavioral changes are our gold standard of treatment. In these cases providers were recommended to provide further education to patients and continue to encourage patients to make positive behavioral changes to help with insomnia.
Some limitations of this study were that even though CMR services captured copious number of patients that met the criteria through an automated system, it did not allow for personal interaction with patients and prescribers on a consistent basis. In addition, it may not capture patients with polypharmacy outside of the defined parameters. Moving forward, the health system is considering expansion of CMR services to allow high risk patients opportunity to meet with pharmacists in the ambulatory care setting. Co-visits with providers can be utilized to provide more consistent interaction with the patient and pharmacist. Additionally, pharmacists are visiting more sites in the health care system to establish a physical presence with both providers and patients. The CMR process can be used to target other high risk populations as well, such as patients with uncontrolled diabetes. It is not restricted for use only with the geriatric population and can be utilized to evaluate any patient's medication profile.
CMR was shown to be highly effective in identifying appropriate medication interventions in order to optimize patient care. Pharmacists are a valuable resource to help target interventions in our high risk populations such as our geriatrics population or patient with uncontrolled diabetes. Utilizing the CMR process provides pharmacists with a standardized approach to evaluating patient profiles for possible inappropriate medication uses.
None.