Frailty is considered often as a physical impairment in the elderly and its characteristics are weakness, weight loss, exhaustion, a decrease of the physical activity accumulating also comorbidity. It is considered the geriatric syndrome related to the aging process, declining of biological reserve that results in an increase of vulnerability for negative results including disability, hospitalization, and death. Frailty was defined as "a state of increased vulnerability on the stress factors due to the decline of the neuromuscular, metabolic, physiologic reserve and immune systems.
To evaluate the role of physical activity and nutrition in the frail older adults, early interventions to slow down the process of fragility and disability in everyday life.
Comprehensive research was performed in literature Medline, Pubmed, Researchgate, The Journal of frailty & aging to realize the aim of this study. The selected criteria of the literature were the published articles during 2007-2018 containing specific keywords such as elderly, fragility, nutrition, physical activity, comorbidity. Included were the studies where the fragility syndrome in the elderly is defined.
Regular studies came to the same conclusion that physical activity has preventive effects in frail elderly even though uncertainty exists in optimal exercise programs regarding the frequency, kind of nutrition and duration. To prevent the fragility, necessary measurements need to be taken with nutrition e proteins, vitamin D and other alimentary, but this information is not yet public domain. The benefits of physical exercises in frailty elderly include increased movement, increased performance in activities of daily living, improved walk, elimination of falls, improvement of mineral bone density and the increase of overall health. However, systems of health care actually are not organized to offer integrated care on daily life, but to identify and treat acute diseases.
Physical activity, Frailty, Elder, Prevention, Nutrition
Frailty is often considered as a physical disability in the elderly. This state is characterized by weakness, weight loss, exhaustion, a decrease of the daily activity as well as the accumulation of comorbidities [1-4]. Frailty syndrome is a medical state characterized by an increased vulnerability, which usually occurs after 65 years and is accompanied by the need for help to perform activities of daily living [5,6]. Worldwide, the number of people over 65 is expected to increase from approximately 900 million in 2015 to over a trillion in 2030 [7]. Increased age is associated with gradual molecular and cellular damage, impairment of bodily functions, decreased muscle mass and strength, loss of bone density, multimorbidity, declining or loss of hearing, vision and recognition, and frailty [8]. Frailty prevalence is higher in older adults that is often wrongly mistaken by many of us as part of the normal aging process. In our daily life we often find difficult to diagnose frailty, to identify the difference between frailty syndrome and normality that is common in the aging vulnerability [5]. For this reason, in 2011 Linda Fried came to an important conclusion defining exactly the frailty syndrome. According to it, a person suffers from the frailty syndrome if he/she has three or five of the following criteria: Weight loss, exhaustion, weakness, slowness and low physical activity [9]. The most well-known way to measure vulnerability are 1) Accumulation of deficit model and 2) Phenotype of vulnerability [9,10]. The first seevulnerability as a vulnerable state in relation to the accumulation of health deficits defined by an index of vulnerability. The phenotype of vulnerability sees it as a syndrome characterized by loss of strength, walking speed, weight, energy and physical activity. Although many tools for measuring vulnerability have been developed, common concepts have emerged over the past 20 years that have informed and facilitated the development of additional assessment tools [11]. Regardless of which vulnerability measure is used, researchers have consistently shown that vulnerability has a detrimental effect on the elderly’s health, as it posed a greater risk of falls, hospitalizations, institutionalization, and premature death [12-14]. As such, identifying its frailty and severity can play an important role in both developing and adapting treatment strategies and preventing them from managing vulnerabilities. Regular participation in physical activity reduces the risk of developing a variety of chronic conditions such as cardiovascular disease, diabetes and certain types of cancer and reduces the risk of falling [15-18]. However, levels of physical activity decline with old age, and older people tend to decrease more and move less in leisure time [19,20]. Due to the potential and weight of medicine and economics, interest in clinics, surgical and medical specialties is increasing. This is mainly related to the follow-up and treatment procedures of these people as well as to medical interventions [10]. In addition to the high prevalence, the clinical relevance of the frailty syndrome lies in the increased morbidity, disability, and even mortality of these patients [21]. Apparently, sarcopenia, loss of muscle mass, is a major factor involved in the development of frailty [22]. Some authors refer to this syndrome as a physical frailty [23]. Therapeutic approaches have focused on behavioral interventions to avoid loss of muscle mass, such as nutritional and physical activity programs (Figure 1).
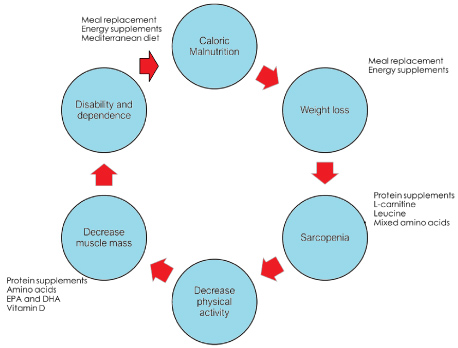 Figure 1: Frailty development cycle, adapted from Fried, et al. [9].EPA: Eicosapentaenoic acid; DHA: Docosahexaenoic acid.
View Figure 1
Figure 1: Frailty development cycle, adapted from Fried, et al. [9].EPA: Eicosapentaenoic acid; DHA: Docosahexaenoic acid.
View Figure 1
Taking in consideration the progressive aging of the population worldwide as well as the consequent overthrow of the population pyramid [5,24], it is tempting to speculate that in the not too distant future, health care providers will need to cope with the growing needs of supportive health workers who will assist people in need with their daily activities. This will be accompanied by an increased financial cost for countries most likely to face this syndrome [5,25,26]. We have therefore undertaken this study to evaluate the role of physical activity and nutrition in older frail persons, early interventions that slow the frailty process, and disabilities in daily life.
To accomplish the goals of this study, comprehensive literature searches were conducted at: Medline, Pubmed, Researchgate, The Journal of frailty & aging. The literature selection criteria were articles published during 2007-2019 with specific keywords such as (elderly, frailty, food, physical activity, comorbidity). These included studies where the frailty syndrome in the elderly was defined. The literature search was restricted to English language publications. Reports or editorials on these issues have been excluded from the research. Additional studies were searched which were searched through lists of research references, citations, and other publications by first authors from relevant materials obtained in the first search (Table 1).
Table 1: Inclusive criteria during papers selection. View Table 1
The criteria for inclusion in this paper were:
1) Randomized research, systematic review, almost experimental studies, or prospective/retrospective cohort studies;
2) Testing, managing and intervening in patients ≥ 60 years of age to prevent or treat frailty. An intervention was defined as an intervention that intervenes in at least two different areas, including exercise therapy, nutritional intervention (protein supplement, vitamin and mineral supplement, or nutritional advice;
3) Classification in terms of (pre)frailty status according to an operationalized definition; and
4) Primary outcomes including one or more of the following: A state of weakness or outcome, muscle mass, strength or power, physical functioning, and cognitive or social outcomes.
The materials were selected based on the title and abstract. After that, the full materials were analyzed for suitability for the purpose of the paper. In the absence of specific requirements of this paper, unnecessary materials are disqualified.
The main outcomes that were included in the final analysis materials were age over 60, weakness, muscle mass, muscle strength, and strength and functional outcomes. Secondary outcomes were quality of life, nutrition, physical activity, comorbidity, social inclusion, and psychosocial well-being. The following flowchart shows how to select the materials analyzed in this paper (Figure 2).
 Figure 2: Flowchart of materials selected in this paper.
View Figure 2
Figure 2: Flowchart of materials selected in this paper.
View Figure 2
From 27 selected papers on frailty over 60-years-old, only 6 of them were analyzed for this paper. These papers are from January 2013 to May 2018. These papers are based on the role of physical activity and nutrition in preventing fractures. The search strategy and selection of papers is as follows (Table 2, Table 3 and Table 4).
Table 2: Research strategy(based on the index of the journals). View Table 2
Table 3: Selection of papers according to authors references. View Table 3
Table 4: Studies characteristics and their findings. View Table 4
The PEDro scale is an instrument for the methodological quality assessment of RCTs in physical therapy and exercise studies
According to Fried (2016), with aging, a new phenotype emerges over 70-years-old, which is distinguished from any other chronic disease. This phenotype of "frailty" is an independent predictor of mortality in short-term (3 years) and medium-term (7 years) [30] and fulfills the criteria for a medical syndrome [1,31,32]. 90% of those that become frailed, frailty is chronic and progressive in its development [33]. Those who have a subclinical presentation with only one or two of the components of the frailty are at 2.5 times at high risk for progression of the syndrome (which will include three to five components present in 3 years of manifestation) the complete phenotype of frailty) [1]. The prevalence of frailty increases with age over 65 and is twice as prevalent in women as men [1,34]. 25% of the older adults over 85 years in the community have these phenotypes; meaning that they have three, four or five frailty components [1].
The impact of the many accompanying physical components and nutrition programs on frailty characteristics has been described by many researchers. In this systematic review, 7 papers by different authors were analyzed, which had as their subject of study prospective cohort studies (article), randomized control studies (2 articles) or systematic reviews (4 articles), mainly in older adults over 60 years. The distribution of these papers by continent is as follows: 1 article from America - 2 articles from the Asia - 3 articles from Europe (England, Spain, and Belgium) and we do not have data for 1 article.
Study protocols are highly heterogeneous. Different populations were studied that varied according to age, gender, the environment of the study and health status of the study participants. In these papers, different types of physical activity, different categories of different supplements, different dietary supplements have been applied, which are reflected in additional doses, and duration of study that varies throughout these papers.
4 of the 7 selected papers present only physical activity accompanied by nutrition programs, while the other 3 present only physical activity programs in frequency.
Il-Young Jang, et al. in 2018, presented a retrospective cohort study in which they applied a 24-week multi-component program to 187 patients located in three different regions in Korea. Although located in different geographical regions, this multi-component program was performed at the same time. During the intervention period, they received group exercise training, nutritional supplements, management for depression, and increased risk of falls. A 60-minute group exercise session was held twice weekly. Each session focused on resistance, balance, and aerobic capacity for ~20 minutes each. Also, participants were provided with a written guide on the exercises they were supposed to do and were encouraged to practice for 60 minutes each day. In addition, all participants received two 125 mL nutritional supplement packs (ready to drink) per day. At the end of this 24-week intervention program, it resulted in the clinical meaningful improvement in terms of physical function, frailty, and sarcopenia. So timely and alternate application of physical activity coupled with nutrient supplements achieves positive results in treating cases with fractures and sarcopenia. According to Il-Young Jang, et al. this outcome benefit was seen even 6 months after the intervention for most participating individuals [35].
Beaudart, et al. in 2017 has presented both nutrient and physical activity as a measure taken in the prevention and treatment of high-frequency sarcopenia (effect on muscle mass and muscular function). In the study by Beadart, et al. a total of 993 references were identified from which only 37 of them have been selected. The number of participants in this systematic review of the papers varies from 17 to 222 individuals and the study time varies from 4 weeks to 18 months. Most of these papers cover both genders and their mean age ranges from 59.5 ± 4.5 years to 87.1 ± 0.6 years.
Among the 37 systematic reviews conducted by Beadart, et al. the impact of interventions (nutrients and physical activity) on muscle mass in frail elderly was evaluated. In nearly 80% of the papers, muscle mass was increased by exercise training. The effect of increasing muscle mass after intervention with dietary supplements was found in only 23.5% of the papers, which were all of the high quality. The additives used were creatine, protein, vitamin D, amino acids, β-hydroxy-β-methylbutyrate supplement, etc. Most studies that have used a dietary creatine supplement have shown a higher effect on increasing muscle mass. This was mostly observed in the case of a combination of creatine supplementation and increased physical activity. So the combination of creatine and resistance training seems to work synergistically. Also, some of these studies showed the positive effect of Vitamin D3 and protein used on muscle mass and muscular strength [36]. At the conclusion of this paper, Beadart, et al. have stated that physical activity has a beneficial effect on muscle mass, muscle strength, or physical performance in healthy individuals aged ≥ 60 years. However, the additional effect of dietary supplementation has only been reported in a limited number of studies [36].
Kwon, et al. in 2017 conducted a randomized control study in women aged ≥ 70 years. They have intervened combined physical training and nutritional intervention for 12 weeks in order to improve physical performance and health-related quality of life (HRQOL) among unregistered women living in the community [37].
A total of 89 women were divided into two groups. The first group participated in a training program accompanied by a once-weekly nutrition program, while the second group only participated in the training program. Results were seen at the end of the 12-week intervention and 6 months after the end of the intervention program. At the end of the 12-week intervention, significant improvements in physical resistance and frailty were generally observed in the first group, whereas the second group saw a smaller change. Positive effects after 6 months were significantly reduced. The combined physical exercise training and nutritional intervention program have beneficial effects in some areas of quality of life and frailty in older women living in the community. However, Kwon, et al. suggest further studies as quite necessary to explore approaches that facilitate the retention of improved outcomes from combined exercise training and nutritional intervention [37].
Dedeyne, et al. in 2017, carried out a detailed study on the effects of the multi-domain intervention on pre-frailty and elderly fragrance. According to these authors, in general, multi-domain interventions tend to be more effective than single-domain interventions in the condition of individuals diagnosed with frailty or to obtain a good result in muscle mass and strength (Sarcopenia) and physical functioning. Physical exercise seems to play an essential role in the intervention which is associated in many areas, where additional interventions can lead to further improvements (eg. interventions with different nutrients) [38].
The combination of physical exercise and nutritional intervention yielded a more positive outcome on frailty status. According to these authors, this effect was not consistently found and is thought to depend in part on variables such as the type and frequency of intervention and the target group. It is of particular interest to note the added value of combining an exercise and nutritional intervention, underlining the contribution of nutritional intervention to deficiency improvements. Moreover, this positive effect on vulnerability appears to be more prolonged in multi-domain compared to single domain interference. These observations support the inherent characteristics of the frailty syndrome: A broad syndrome that requires broader access to entire systems together [38].
Muscle mass and strength showed a tendency to be more effectively improved by multi-domain compared to single-domain interventions. Specifically, combined physical exercise and nutrient supplementation intervention showed a tendency to improve muscle mass and muscle strength more than exercise programs and nutritional intervention if applied separately. Skeletal muscle strength is not only dependent on muscle mass, but is a function of numerous factors such as nutritional, hormonal, and neurological components. Therefore, it is likely that combining two or more of these interventions will increase the efficacy of the intervention. In addition, the duration of the intervention has an effect on these improvements [38].
Regarding physical activity intervention and its impact on frailty, there are many papers that present the benefits that frail individuals benefit during and after physical activity intervention. In this paper, we have presented studies by Carmen de Labra, Gine-Garriga, and Kehler. Carmen de Labra, et al. presented in 2015 a paper on the impact of physical activity on frail individuals. Of the 507 articles selected, only nine documents met the specific criteria they have been filtered. Six of them included multi-component training interventions (aerobics and resistance), one included comprehensive physical treatment and the other two included strength-based exercise training. All nine of these papers involved a control group receiving no treatment, maintaining their usual lifestyle, or using a home-based exercise program. Five of them saw the effects of exercises on their fall parameter and among them, three found a positive impact of exercise interventions on this parameter. Six of them reported exercise effects in some aspects such as mobility, and among them, four showed improvements in some measurements of this outcome. Three papers focused on the effects of an exercise intervention on balance performance and one showed improved balance. Four papers investigated functional ability and two showed positive results after the intervention. Seven papers investigated the effects of physical activity interference on muscle strength and five reported increases; three workouts showed the effects of exercise on body composition and condition, finding improvements for this parameter in two of these exercises. As a conclusion of this study, these authors have found that intervening physical activity in different forms in frail individuals has shown an improvement in the measurement of different outcomes, but nevertheless, large differences have been found between studies regarding the size of the fractures. the effect after the intervention of physical activity [39].
According to Gine-Garriga, physical deterioration is considered a precursor to disability and dependence on others for daily activities. Frail individuals are seen as a group of patients presenting more complex and challenging problems for healthcare professionals. In their paper, Gine-Garriga, et al. evaluated whether a 12-week functional training program can reduce self-reported fears of a decline and improvement in health status in a group of frail elderly individuals. This study included 51 female and male individuals with a mean age of 84 ± 2.9 years. Individuals underwent a functional circuit-training program. Individuals were divided into two groups in the experimental and control groups. This program focused on a combination of low power-based functional and exercise balance. The self-reported measure of fear of decline (specific activity reliability scale) and health status was assessed at weeks 0, 12 and 36. At the end of this 12-week follow-up, it was seen that the experiment group had greater improvements than those of the control group. These improvements were maintained until the 36th week following, with significant interactions [40].
Kehler, et al. in 2018 studied the lifestyle factor (physical activity) which is known to reduce the risk of frailty. They have studied six longitudinal and ten cross-sectional studies where the sample size ranges from 26 to 5871 individuals. Studies generally ranged from low to moderate risk. Most studies have used the Fried criteria to measure frailty. Five studies measured questionnaire sedentary behavior, with three studies specifically measuring television viewing time. Seven studies measured sedentary time with accelerometry. Thirteen of the sixteen studies observed a harmful association between high amounts of sedentary behaviors and a greater prevalence of frailty or higher levels of frailty. Six of the seven studies that regulate physical activity behaviors showed an independent association between sedentary behaviors and frailty. All six longitudinal studies found a negative association between sedentary behavior and frailty.
At the conclusion of their paper Kehler, et al. concluded that sedentary behaviors were associated with a higher prevalence of frailty or higher levels of frailty. They, therefore, recommend further longitudinal studies of physical activity to determine the links between sedentary life, increased physical activity, and frailty [41].
Systematic and randomized control studies came to the same conclusion that physical activity has a detrimental effect on older frail persons and why there is uncertainty in optimal exercise programs regarding frequency, type of exercise, and duration. Prevention of fractures requires proper nutrition of proteins, vitamins D and other nutrients, but this information is not yet in the public domain. Benefits of physical exercise in older adults with frailty include: Increased mobility, increased performance in activities of daily living (ADL), improved walking, elimination of radiation, improved bone mineral density and increased overall well-being. However, health care systems are not currently organized to provide integrated care over daily life, but to identify and treat acute illnesses.
Physical activity and adequate nutrition, especially with regard to vitamin D, calcium and protein are key lifestyles that simultaneously improve bone, muscle and functional outcomes in the elderly population, if they are individually adjusted and determined. Preventive methods through physical activity, in frail elderly, should be described in a progressive individualized plan just like other medical treatments.