Long term care facilities are the homes of elderly people worldwide; due to vulnerability and rapid spread of infection (droplets or fomites) the risk of severe outcomes from outbreaks of COVID-19 is of concern.
Evaluation of COVID-19 pandemic impact in a closed setting including the clinical features of the infection in an elderly population and the role of nasopharyngeal swab testing.
We analyzed data of cases from the beginning of the epidemic, confronting clinically suspected patients (absence of nasopharyngeal testing -T0) with symptomatic COVID-19 patients (availability of rRT-PCR testing - T1); all data were censored after complete nasopharyngeal swab SARS-CoV-2 negativity (T2). Containment procedures and contact tracing are reported.
48 COVID-19 linked residents were identified. They were divided into four groups: Symptomatic pre - COVID-19 testing, symptomatic COVID-19, pre-symptomatic COVID-19 and asymptomatic COVID-19. The mean (± SD) age was 85 ± 6 years (range 73-100 years); among the symptomatic patients cohort 21 patients died (56%): fatality rate 48%. Mortality rate in this series was 31% (sex specific: 37% for men and 25% for women), mean (± SD) age 85 ± 7 years (range 64-100 years), 31% men.
The main risk factor for death was encefalopaties (either vascular or degenerative) with cognitive impairment. Respiratory symptoms were uncommon and fever below 38 ℃ - 100.4 ℉ was the most frequent sign. Clinical deterioration, without gradual worsening, led to death with a median length of survival 2 days (interquantile range 1 to 2 days).
During COVID-19 outbreak mortality among elderly is high in long-term care facilities. Cases in this series had atypical symptoms and signs compared with younger populations; rapid and unexpected clinical deterioration occurred; these characteristics may help understand and define adequate approach to elderly patients cared for outside hospital (i.e. at home or non-traditional settings) in the future.
According to report from the World Health Organization (WHO) [1] older patients have increased risk of severe disease and mortality in case of infection with SARS-CoV-2; poor outcomes [2-4] have been confirmed by the fatality rates for patients over 80-years-old in China and in Italy [5] (approximately 21.9% and 20.2% respectively). Data from Italy's Official Health Care Institution- IstitutoSuperiore di Sanità- updated to may 21, 2020 reported 31096 deaths with a mean age of patients dying for SARS-CoV-2 infection 80 years (median 81, range 0-100, IOR 74-87) [6]. Worldwide the elderly population often resides in long term care facilities (LTCFs) where infectious diseases have always been a significant burden.
Frailty due to multiple chronic diseases and sharing common spaces (dining rooms, areas for group activities) foster possible outbreaks of COVID-19 in the ongoing pandemic.
Presently there is no effective weapon against COVID-19 and WHO stresses the importance of appropriate measures of infection prevention and control (IPC) [1] in all clinical settings and in particular in LTCFs.
Reports describing patients in LTCFs in this COVID-19 pandemic are limited [7,8].
Italy has 2399 long-term care facilities (44457 beds on February the 1st, 2020); 8% do not have any on site medical assistance while the rest have a mean of 2.6 physicians; on the survey dated April 6th 2020, 3859 LTCF residents had died and the highest percentage (47.2%) was concentrated in Lombardia region, the epicentre of COVID pandemic in Italy [9].
An outbreak of COVID-19 in an LTCF in the Seattle, Washington area, in March 2020 was associated with several deaths reporting a fatality rate for residents 33.7% [10].
We report the experience of a COVID-19 outbreak in LTCF of northern Italy; the aim of this study of COVID-19 pandemic impact in a closed setting is the evaluation of the clinical features of the infection in an elderly long-stay population and the role of nasopharyngeal swab testing.
Management was person-centered and tailored in the facility, due to the local unique and dramatic circumstances of emergency departments and acute care facilities overwhelmed by severe symptomatic patients with limited number of intensive care unit beds and respirators.
First nasopharyngeal swab testing for SARS-CoV-2 was performed between April 4-April 7 and it was repeated every 2 weeks.
Patient data were censored at the time of date cut off, which occurred on May 11, 2020, when the results of all nasopharyngeal swabs were again negative.
This LTCF is a 74-bed facility of dependent long-stay residents located near the city of Brescia in Lombardia, northern Italy.
Data of vital signs and clinical status are analysed retrospectively from the beginning of the epidemic in March 2020 (availability of testing limited due to overt nasopharyngeal swabs lacking) through April 2020, when first testing was performed, to May 11, 2020, when the results of nasopharyngeal swabs were all negative (Figure 1).
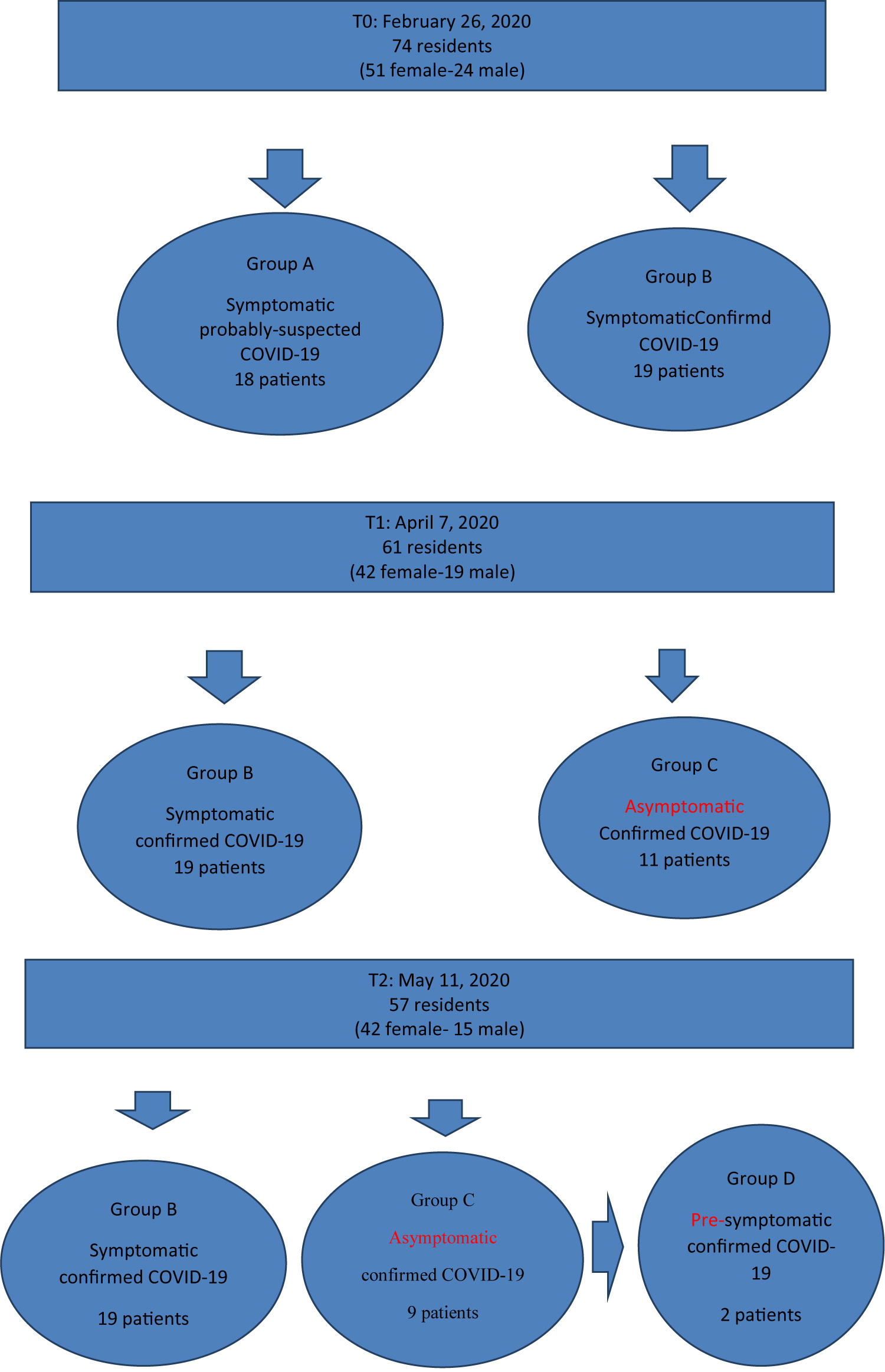 Figure 1: Results of nasopharyngeal swabs test.
View Figure 1
Figure 1: Results of nasopharyngeal swabs test.
View Figure 1
Three serial point prevalence surveys were conducted: At the beginning of the pandemic (time T0 February 26:74 residents - 51 female and 24 male); on April 7 (time T1 with availability nasopharyngeal swab testing: 61 residents - 42 female and 19 male) and at the end of the FU (T2 May 11: 57 residents- 42 female and 15 male).
A cohort of 48 COVID-19 linked residents was identified and 4 clinical groups were categorized: Group A (18 probable or suspected COVID-19 patients) - group B (19 symptomatic patients confirmed COVID-19) - group C (9 asymptomatic COVID-19 patients) - group D (2 presympotmatic COVID-19 patients). Dividing COVID-19 patients in sub-groups, including the presymptomatic, has been validated in some recent reports in literature [11-16].
Probable or suspected COVID-19 patients were identified based on the assumption that unexplained illness with clinical symptoms and signs of infection either of the airways or of the gastrointestinal gut (Table 1) was otherwise due to the infection agent circulating around in the community and in hospitals; main comorbidities ascertained by medical charts were considered in the differential diagnosis (Table 1).
Table 1: Clinical characteristics of patients in the long-term care facility. View Table 1
Confirmed COVID-19 patients were defined by a positive result on a reverse-transcriptase-polymerase-chain-reaction (RT-PCR) assay of a naso-pharyngeal swab.
Descriptive statistics were used to summarize the data; results are reported as medians; categorical variables were summarized as count and percentages.
During the period from February 26 (time T0) through May 11 (time T2) we identified a cohort of 48 patients linked to COVID-19; 37 had clinical symptoms and signs of infection (group A, 18 patients, 23% of total population at time T0 and group B, 19 patients, 30% of remaining population at time T1); the mean (± SD) age of the patients was 85 ± 7 years (range 64 to 100); 31% were men.
Asymptomatic COVID-19 positive patients (group C + group D) were 11 (18% of the population at time T1); only 2 patients (3% of the population at time T1) during the FU as of May 11 resulted pre-symptomatic (group D).
No changes in chronic symptoms were reported; all residents had been vaccinated against circulating seasonal viruses such as common cold influenza; bacterial co-infections, such as staphylococcus or streptococcus, in a period of confounding seasonal influenza would have been controlled by the wide use of empiric antibiotics (Table 2).
Table 2: Patient count of those who underwent therapies and the outcomes of treatment. View Table 2
Chronic medical conditions were common in this elderly population (Table 1).
Fever was the most common sign in 62% of the cases (above 38 ℃ in 8 patients and below 38 ℃ in 15 patients); the most common symptom at infection manifestation was cough which occurred however in only 5 patients (13%); other symptoms such as diarrhea, malaise and sore throats were present each respectively in 2 patients (5%); oxygen saturation on room air < 90% was present in 8% (3 patients).
As of May 11, of the 37 symptomatic patients 21 (56%) had died: 3 patient of group B, affected by COVID-19, and 18 patients who belonged to group A, which did not have a COVID-19 confirmed diagnosis because death occurred before availability of testing with nasopharyngeal swabs; 2 patients asymptomatic at time T1 died 1 week before date of cut off May 11 (T2) and there for were identified as presymptomatic (group D); the fatality rate for infected residents was 48% (23 of 48) (Figure 2), mean age (± SD) 86 ± 6 years.
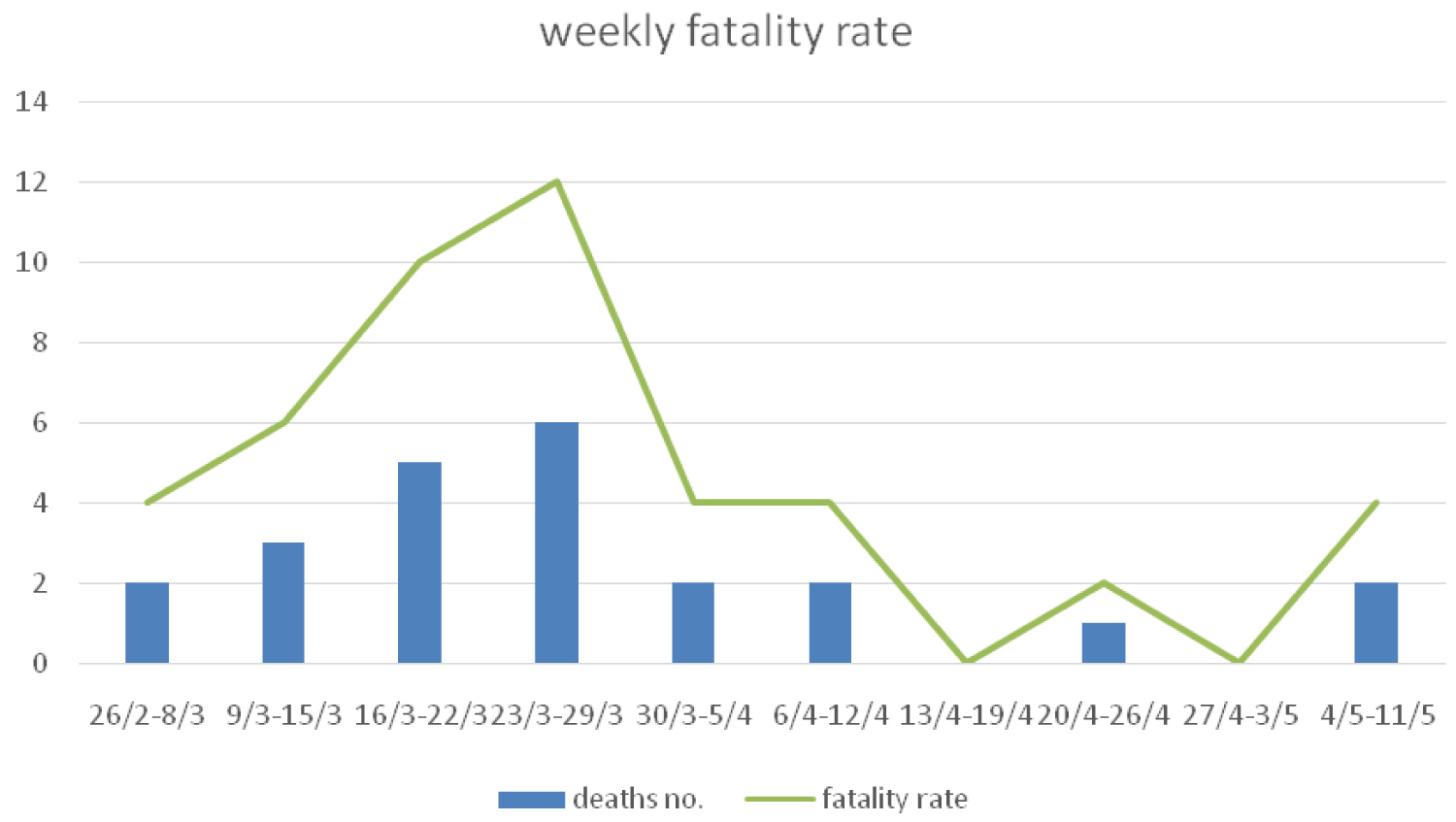 Figure 2: Weekly fatality rate (26/02/2020 - 11/05/2020).
View Figure 2
Figure 2: Weekly fatality rate (26/02/2020 - 11/05/2020).
View Figure 2
The global mortality rate among all residents was 31% (23 of 74) versus a mortality rate at the same period of the previous year (2019) equal to 1%.
Of the 23 patients only 9 were men (39%); sex specific mortality rate was 37% for men (mean age 86 ± 7 years, range 77-100 years) and 25% for women (mean age 85 ± 6 years, range 73-90 years); a greater percentage of patients over age 80 had died than patients under 80 years of age (83% vs. 17%); the median length of survival after symptom/sign onset was 7 days (interquartile range 5 to 10); the median length of survival after rapid deterioration leading to death was 2 days (interquartile range 1 to 2).
Fifteen patients (71%) reported at onset of COVID-19 infection the only sign of fever (5 cases above 38 ℃ and 10 cases below 38 ℃); the remaining 8 (28%) reported atypical symptoms.
Encephalopahies (either vascular or degenerative), with various degree of cognitive impairment, were the prominent clinical condition (16/23) often in association with either ischemic heart disease or a metabolic syndrome (NIDDM- hypertension - obesity) (Table 1).
All patients were regularly monitored and received conventional supportive care interventions (Table 2) including antibiotics (18/23), oxygen therapy (18/23), steroids (14/23) and volume resuscitation (14/23); hydroxychloroquine was added according to intervening recommendations in 7 cases.
Main causes of death, on the basis of a clinical diagnosis in a non-acute setting, was either cardiac shock (refractory hypotension) or refractory respiratory failure (oxygen saturation under 90% despite supplemental oxygen) often leading to death in less than 2 hours; any attempt to transfer to acute settings was withhold due to the rapidity of clinical deterioration.
It was not possible to distinguish between deaths due directly to COVID-19 or associated with COVID-19 that could have had a prominent role in triggering the original comorbidities (Table 1).
In order to release pressure on local acute-care hospitals, overwhelmed by critical or severe COVID-19 cases necessitating advanced oxygen/ventilatory support, communication between the medical/nursing staff and the families was strengthened; a terminal palliative approach was endorsed in 65% of the cases (13 patients received palliative sedation with morphine and 2 patient terminal sedation with midazolam) (Table 2).
Mean time of nasopharyngealSARS-CoV-2 negativity was 29 days ± 7 (range 16-39).
This study describes a cluster of elderly patients who encountered COVID-19; they were all long-stay residents of a LCTF located in the northern part of Italy, where first the infection erupted in March 2020.
The findings of this study highlight some important features of the approach to the elderly; as real life photography of what happened in a chaotic moment the particular clinical manifestations and the rapidity of evolution of the infection are underlined.
In this population mild signs and symptoms involved 50% of the residents without any need of hospitalization in accordance with WHO's guidance [1]; data from China revealed mild-to moderate disease in 81% of the population with 14% cases of severe illness and 5% critical [17]; according to our experience sudden, rapid and unexpected deterioration into a severe or critical illness threatened 31% of the population, leading irreversibly to death in a little lag of time (1-2 days) and without alarming overt signs/symptoms of an intervening complicated disease.
Isolated fever under 38 ℃ of temperature was the most common sign at clinical onset in 40% of symptomatic cases; clinical signs of respiratory involvement as cough or sore throat were less common (respectively only in 14% and 2% of patients); this confirms as an atypical clinical presentation must be expected in the elderly population so delay in identification of COVID-19 infection by means of nasopharyngeal swab may occur if respiratory symptoms are attended; another possible cause of delay in diagnosis is the mental status, secondary to neurocognitive disorders, that in this study affected 68% of the fatality cases.
The findings of this study could apply to the general population. In fact many patients treated by general practitioners are often elderly who are presenting symptoms of COVID-19 in their homes who have not yet been tested. We had 64% of residents linked to COVID-19 with the threat that cannot be ignored, of the asymptomatic carriers of COVID-19 (18% of the residents with positive tests in this LTCF) who may play a major role in the transmission of SARS-CoV-2.
Fatality rate among the infected (48%) in this series is higher than the one of the similar outbreak of COVID-19 in an LTCF on the other side of the ocean in the city of Seattle, Washington USA, in March 2020 (33.7%) [10]. However compared with the fatality rates (50%) in intensive care units of the Seattle Region, with younger critically ill patients [18], a lower fatality rate of elderly in LTCFs poses serious questions on the pathogenesis of the disease and on the allocation of resources at a time of unprecedented crisis by health system leaders, with enormous ethical issues of appropriate approach and therapies to those at the end of life. In fact the absence of rapid on-site naso-pharyngeal swab mass testing of residents of LTCFs was the main cause of the dramatic fatalities of elder people in the first months of the pandemic in Italy (total 3859 deaths - 47.2% concentrated in Lombardia region) [9].
This study confirms how rapid and widespread the transmission of SARS-Cov-2 can be in a congregate setting, where physical distancing is not always possible considering the high percentage of residents affected by cognitive impairment as dementia. In this case after complete restriction to visitors, including relatives, to prevent further introduction of SARS-CoV-2 (closure of the LTCF on March 4, 2020) proactive steps to contain the spread were urgently adopted. The effects of these measures seen after 2 months resulted in complete negative NF testing on May, 11, 2020.
First, isolation of all suspected cases with widespread use of PPE of staff and, if possible, of the residents was made compulsory. Diffuse use of alcohol-based hand sanitizers as well as plans of regular sanitization of all surfaces and rooms was enhanced and any contact between residents was limited, according to the policy of social distancing, with all meals served in the bedrooms.
Second, once the results of nasopharyngeal swabs, (performed between April 4-April 7), were available on April 8, 2020, compartmentalization was achieved with transfer of all positive cases for surveillance and quarantine within the facility.
Contact tracing of all cases revealed that sites of spread were the points of aggregation of small groups of residents, in particular the same table for lunch or dinner or for table-games (chest or cards). Case tracing identified two possible sources of infection spread: Contacts with relatives and one suspect resident.
External contact with relatives or friends in fact continued until Italy's national lockdown on March 8; at that time Italy had a context of supply shortages of personal protective equipment. The risk of introduction of the pathogen from around the community was therefore very consistent.
The index resident was discharged on the 28th of February from a local acute-care hospital where he had been transferred for pneumonia when routine PCR testing of naso-pharyngeal swab or other specimen for SARS-CoV-2 was not performed for thorough differential diagnosis. At that time the only known risk for SARS-CoV-2 exposure, according to local hospital guidelines, was from returning travellers from China. The resident worsened clinically for 3 days after which he died from septic shock on March 11, 2020. Unfortunately it was not possible to confirm post-mortem COVID-19 infection.
First, the assumption that the 18 patients, who died before availability of testing for COVID-19, had been infected by SARS-CoV-2; however the comparison with the monthly mortality of 2019 (1% vs. 31% of this study) strengthens this assumption.
Second, all diagnosis are based on clinical ground, due to the lack of laboratory and radiologic findings consistent with either the features of a LTCF or the difficulty of access to the overcrowded acute-care facilities in March 2020 in the region of Lombardia.
Third, patients received care focused on conventional supportive care interventions and on comfort measures.
Fourth, medical and nursing staff members were tested between April and May; therefore it was not possible to document their role in the transmission of SARS-CoV-2 in this facility.
The experience described in this study is an important lesson for the forthcoming months; it indicates that outbreaks of COVID-19 in long-term care facilities have the potential to spread widely and rapidly and to increase the burden on regional health care systems if uncontrolled.
Infectious cases in elderly in this series had atypical symptoms and signs compared with younger populations; sudden, rapid and unexpected deterioration occurred; these characteristics may better help understand and define adequate approach to elderly patients cared for outside hospital (i.e. at home or non-traditional settings).
Symptom-based screening alone will fail to detect a high proportion of infectious cases in elderly and will not control transmission in enclosed populations; rapid on site naso-pharyngeal swab mass testing of all residents of LTCFs for compartmentalization of cases is highly recommended until other more effective measures will be available (vaccine o proved chemoprophylaxis).
The authors declared that they have no conflicts of interest.
The authors are all part of the medical staff working in the facility.