Recurrent viral shedding (RVS) in COVID-19, between four and 31 days following a test of cure, has been noted in the medical literature [1-4]. Here we describe a case of recurrent and protracted viral shedding in a nursing home patient admitted to the hospital. Following symptomatic COVID-19 and viral shedding for 36 days with subsequent test of cure, a further positive RT-PCR was obtained 45 days later when the formerly symptomatic patient was readmitted for urgent urinary tract surgery. The total time between the first and most recent positive test was 104 days. Simultaneous virus-specific antibody testing was negative. Prolonged viral shedding (PVS) as an index of serious acute COVID-19 in nursing home residents and RVS with negative antibodies are explored.
COVID-19, Prolonged viral shedding, Recurrent viral shedding, Immunity, Nursing home residents
Recurrent [1-4] and very prolonged [5] COVID-19 upper respiratory tract viral shedding in predominantly young and middle-age patients have been described in the literature. The clinical and prognostic implications of these phenomena have yet to be fully elucidated. There is consensus viral shedding does not equate with infectivity, and transmission is limited to days rather than months following infection [6,7]. Unfortunately, little attention has been paid to the study of nursing home residents with COVID-19. There remains a dearth of published information on the clinical course, viral load and shedding in this population. Studies utilizing multivariate analyses of demographic and clinical attributes associated with PVS include younger patients (median age 42 to 52) with fewer underlying health conditions. They found the time from symptom onset to admission, highest temperature at admission, and need for mechanical ventilation are independently associated with prolonged shedding. The definition of prolonged shedding varies in these studies and ranges from greater than 11 to greater than 17 days from symptom onset to negative RT-PCR testing [8-10]. The implications of these risk factors for PVS are best demonstrated by larger studies identifying predictors of serious infection. In a study of 138 hospitalized patients with COVID-19 pneumonia, there was a significant and positive association between time to admission after onset of infection and severity of disease [11]. There is also evidence that the highest temperature during hospitalization is significantly correlated with case fatality rates. For every 0.5-degree centigrade increase in body temperature above 37 degrees, there was a significant increase in case fatalities [12]. In a study of 41 severe cases of COVID-19 (median age 41), a direct connection between disease severity and PVS was described; median viral shedding was prolonged at 31 days [12]. Weiss, et al. (2020) published a meta-analysis examining 650 patients among 22 studies and found an average duration of viral shedding in the upper respiratory tract of 12 days in mild and 16 days in moderate to severe disease [14]. Taken together, these findings strongly suggest that PVS is a lagging indicator of prior serious infection.
In two studies of nursing home outbreaks in Washington State, the median age of residents is typically in the seventh and eighth decades and comorbidities are numerous and in double digit percentages [15,16]. Insofar as the greatest mortality from COVID-19 occurs among residents of nursing homes [17], and the recent report of very prolonged viral shedding in this population (median 29 days, maximum 71 days) [18], it is important to explore the phenomena of prolonged shedding among infected residents and the protracted and recurrent viral shedding in the case presented here. This may offer further insight into the triage, care and treatment of COVID-19 in this population. Elderly patients pose additional challenges to timely recognition of serious infection owing to their blunted temperature response to infection [19] and atypical presentation [20]. Delay or failure to recognize serious illness and provide commensurate medical care in these patients may meaningfully contribute to the devastating mortality from this disease. A case of recurrent and protracted COVID-19 viral shedding in a nursing home resident with simultaneous negative virus-specific antibodies is described and implications discussed. In this report, protracted viral shedding is defined as documented positive COVID-19 by RT-PCR over 70 days.
A 70-year-old skilled nursing home (SNH) resident was initially admitted to the hospital for isolation and care three days after testing positive for COVID-19 by RT-PCR. He experienced intermittent cough only (mild disease) during hospitalization and was discharged to isolation at the nursing home feeling well but still testing positive at 36 days. Discharge criteria included a minimum period of 30 days since a first positive test, or two negative RT-PCR tests at least 24 hours apart. The resident returned to the nursing home to isolation and subsequently tested negative by serial RT-PCR but was readmitted 53 days after discharge for treatment of urinary tract infection and fever with subsequent removal of a renal stone and resolution of symptoms. Per preoperative protocol, the patient was retested by RT-PCR prior to surgery and was positive, 104 days after his initial positive test. Importantly, anti-nucleocapsid antibody testing (Abbott SARS-CoV-2 IgG assay™) was negative three days later on the day of discharge (Figure 1). During this hospitalization, he remained asymptomatic for COVID-19. The patient's past medical history is remarkable for hypertension, chronic urinary retention with indwelling catheter, and obesity.
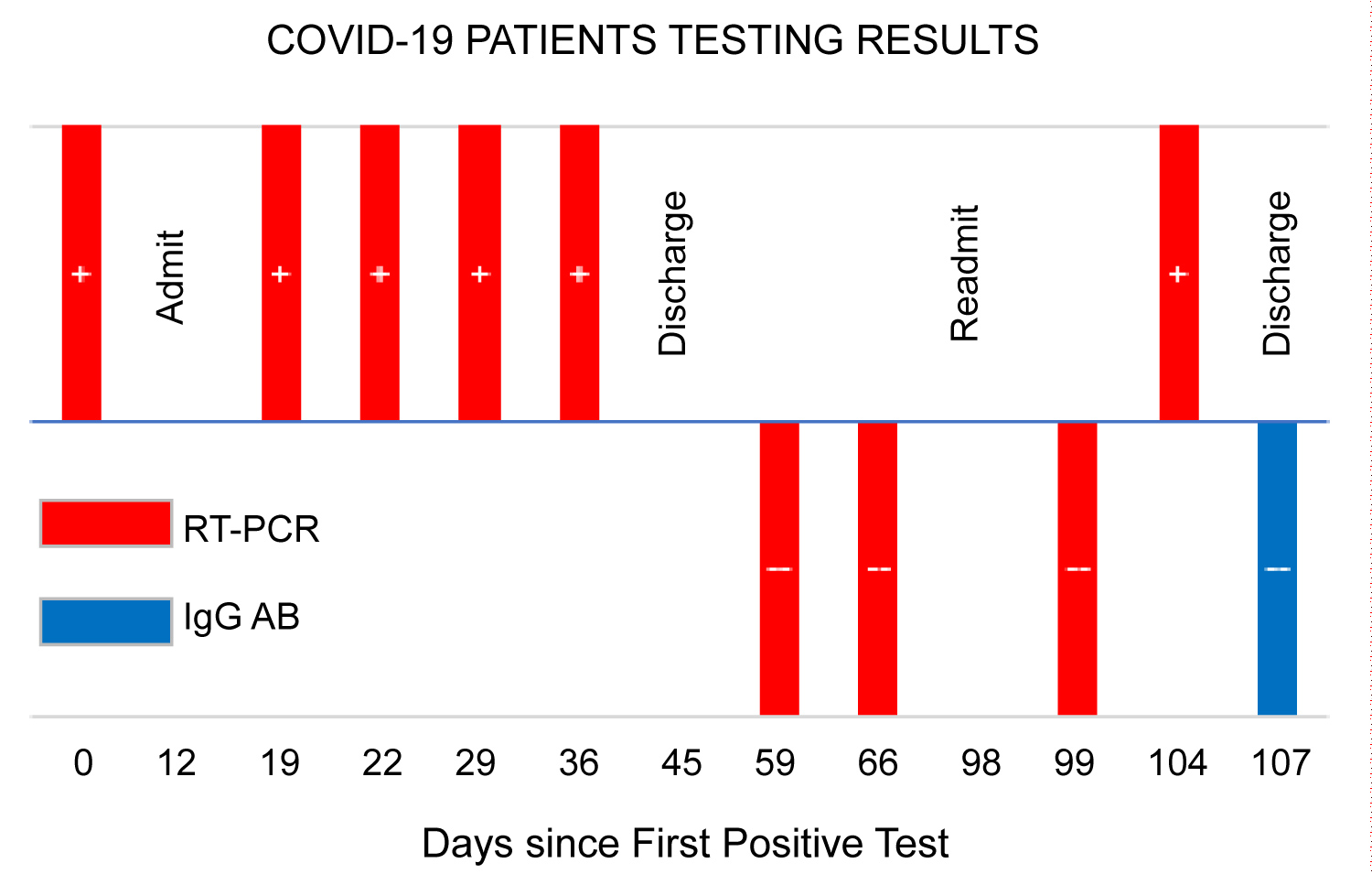 Figure 1: COVID-19 patients testing results.
Figure 1: COVID-19 patients testing results.
RT-PCR (red bars) and IgG anti-nucleocapsid protein antibodies (blue bar); (+) positive test results; (--) negative test results. Day 0 represents initial RT-PCR patient test.
View Figure 1
In this case study, a preoperative positive RT-PCR test was obtained 104 days after the initial diagnosis of COVID-19 and following two negative tests at least 24 hours apart. The finding of a positive test following serial negative testing has been described in COVID-19 patients and found to represent a true positive by serial repeat analyses [21]. Furthermore, it has been shown that immunosenescence is a natural condition of aging with wide ranging defects in the innate and adaptive immune systems [22] and could, therefore, contribute to persistence of virion debris in the upper respiratory tract as well as serious infection and mortality in elderly patients. Despite recurrent viral shedding (RVS), serum antibody testing was negative in this patient, an indication that residual virion debris may not necessarily stimulate or sustain humoral antibody response in elderly COVID-19 patients.
Several recent reports address humoral and T-cell immunity to COVID-19. They attempt to distinguish factors related to the strength of acute response and sustained versus waning immunity during the early and late convalescent phases of disease [23-26]. There is agreement among these reports that strength of antibody response during the acute phase of infection correlates with severity of disease. However, there is no clear consensus regarding the duration or strength of humoral immune response during convalescence from COVID-19. Resolving this question may shed important light on improving the care and treatment of our elderly, especially those with underlying serious health conditions.
In the case reported here, recurrent and protracted viral shedding may be evidence of diminished humoral and T-cell immunity; conditions shared by the elderly and infirm in long-term care facilities [22]. RVS and PVS also may indicate a past active infection more severe than apparent on initial presentation. This case would appear to represent reactivation rather than reinfection despite the long interval between negative serial testing and a recurrent positive test (45 days). On readmission for surgery, the patient had no COVID-19 symptoms or IgG anti-N antibodies. Because of the relatively short period of infectivity (8 to 18 days) [6,7] following onset of COVID-19, there has been little impetus to conduct studies of recurrent and protracted viral shedding. Therefore, the incidence and implications of protracted and recurrent viral shedding still remain unknown.
The current literature supports a significant association between COVID-19 severity and duration of viral shedding in largely healthy young and middle-aged cohorts. However, one case series did describe a cohort of infected nursing home residents with PVS (median age 83, median viral shedding 29 days) admitted to the hospital with apparent mild or asymptomatic disease [18]. It is important to keep in mind that atypical clinical presentation during serious infection, and specifically, in COVID-19 is commonplace among residents [19,20]. This case report describes recurrent and protracted shedding in a previously infected and symptomatic nursing home patient.
Whether PVS in general, and protracted viral shedding in this case are solely related to immunosenescence and the natural tendency for diminished humoral and T-cell immunity among the elderly, or reflect a population with more severe disease than apparent when presenting with COVID-19, has yet to be determined. Both may contribute to an infection fatality rate of one in four. Since it is not possible to change inherent immunity deficits in the elderly and infirm, an approach that treats all COVID-19 nursing home patients as seriously ill may be prudent. If all nursing home residents who contract the infection suffer significant disease, as suggested by PVS, the question remains whether admission to the hospital at the time of diagnosis would reduce mortality through early enhanced medical and multidisciplinary care. This also further highlights the importance of early identification of disease through robust testing of nursing home residents and staff, and rapid isolation of infected residents to stem outbreaks.
A recent systematic meta-analysis estimated the infection fatality rate of 0.68% in COVID-19 [27]. Statistics compiled by the Centers for Medicare and Medicaid Services (CMS) show a nursing home infection fatality rate for the week ending August 23, 2020 of 25% [17]. A nursing home resident in the US is 37 times more likely to die from this disease than the general population. Nursing home residents make up only 0.4 percent of the US population but represent 27% of all deaths [17,28].
Of interest is the absence of anti-N IgG antibodies despite evidence of viral shedding in this case. Additional research is urgently needed to fully understand the ramifications of prolonged viral shedding and humoral response in nursing home residents if we are to improve the care and survival of the most vulnerable to mortality from COVID-19.
This material is the result of work supported with resources and the use of facilities at the Mann-Grandstaff Veterans Affairs Medical Center, Spokane, Washington, USA. The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. I would like to acknowledge the men and women of Mann-Grandstaff VA Medical Center for their dedication and skill in the care of community patients during the COVID-19 pandemic and in fulfilling Veterans Affairs' fourth mission. I also would like to recognize Stephen D. Fischer for his invaluable assistance in proofreading this submission.
No funding has been received for this work.