Hallucinations are common in different clinical disorders associated with older age. The differential diagnosis of new onset complex visual hallucinations is vast. A case is reported of a 70-year-old man who presented with visual impairment attributed to retinopathy, that then developed complex visual hallucinations. Charles Bonnet syndrome (CBS) was initially diagnosed. Throughout the course if his disease, he developed rapidly progressive dementia associated with myoclonus and pyramidal signs. MRI showed cortical ribboning on T2-weighted and diffusion-weighted images. A real-time quaking-induced conversion (RT-QuIC) > 98% was reported, as well as a positive 14-3-3 protein in cerebral spinal fluid (CSF). The diagnosis of Heidenhain variant of Creutzfeldt-Jakob Disease was made. The association of complex visual hallucinations and visual impairment in the absence of cognitive decline may strongly suggest the diagnosis of CBS. Nevertheless, the differential diagnosis must be broadened as this can also be the first symptom of a fatal neurodegenerative disease.
Visual hallucinations, Charles Bonnet Syndrome, Rapidly progressive dementia, Heidenhain variant
Visual hallucinations are defined as visual perceptions that are experienced when fully conscious but in the absence of corresponding external stimulus [1]. The differential diagnosis of new onset complex hallucinations in the elderly is vast. Hallucinations can occur in different pathologies but also in otherwise healthy individuals and are believed to occur more frequently among the elderly [2]. They can present a symptom of sensory, neurological, medical, neurodegenerative, and psychological disorders [2]. Hence, diagnostic approach must be very precise and largely relays on a detailed history and clinical exam. A lot of emphasis must be given to accompanying symptoms, including confusion, cognitive decline, motor symptoms, sensory deficits, among others [3].
We present the case of a 70-year-old man, who presented to the hospital with visual hallucinations and confusion. His past medical history was relevant for poorly controlled diabetes mellitus. He began with gradual vision loss and blurred vision over the past 3 months. He consulted an ophthalmologist and a diagnosis of non-proliferative diabetic retinopathy with bilateral macular degeneration was made. Laser photocoagulation was performed. Seven days later the patient began with complex visual hallucinations described as spiders walking on the wall, geometric figures on the floor and people's faces. Symptoms lasted from few seconds to minutes and presented several times during the day. Neither behavioural changes nor disorientation were present. A diagnosis of Charles Bonnet syndrome was suspected, and patient was started on haloperidol 2.5 mg TID. Hallucinations gradually worsened causing emotional distress and agitation. Three weeks later, patient developed confusion with inability to recognize familiar faces and accentuated agitation. In the following days language problems and memory impairment became evident causing complete dependence. Family members consulted neurology department at our institution. General physical exam showed no abnormalities. On mental exam patient was awake but with profound inattention and disorientation. Language was non-fluent with affected naming and repetition. Working memory was also clearly affected. Menace reflex seemed abolished in both eyes with preserved pupillary function and normal fundoscopic exam. The rest of the neurological exam was unremarkable. Diagnostic approach began for suspected cortical blindness and encephalopathy. Blood tests and a complete autoimmune panel were unremarkable. A screening for hepatitis B, C, HIV, and syphilis were all negative. MRI showed cortical ribboning on T2-weighted images more evident on diffusion-weighted images and with clear predominance for occipital, parietal and temporal lobes bilaterally. High signal intensity in the right caudate nucleus was also apparent on DWI and FLAIR imaging (Figure 1). An electroencephalogram revealed diffuse slowing and periodic sharp wave complexes. A lumbar puncture was performed with normal cytochemical characteristics and tau protein > 4000 pg/ml. A real-time quaking-induced conversion (RT-QuIC) > 98% was reported, as well as a positive 14-3-3 protein in cerebral spinal fluid (CSF). A definite diagnosis of Heidenhain variant of Creutzfeldt-Jakob was made. During the following two weeks patients developed paratonia of all four limbs, frontal release signs and bilateral extensor plantar response. Sporadic segmental myoclonus in the upper extremities were also noted. Patient died three weeks after admission.
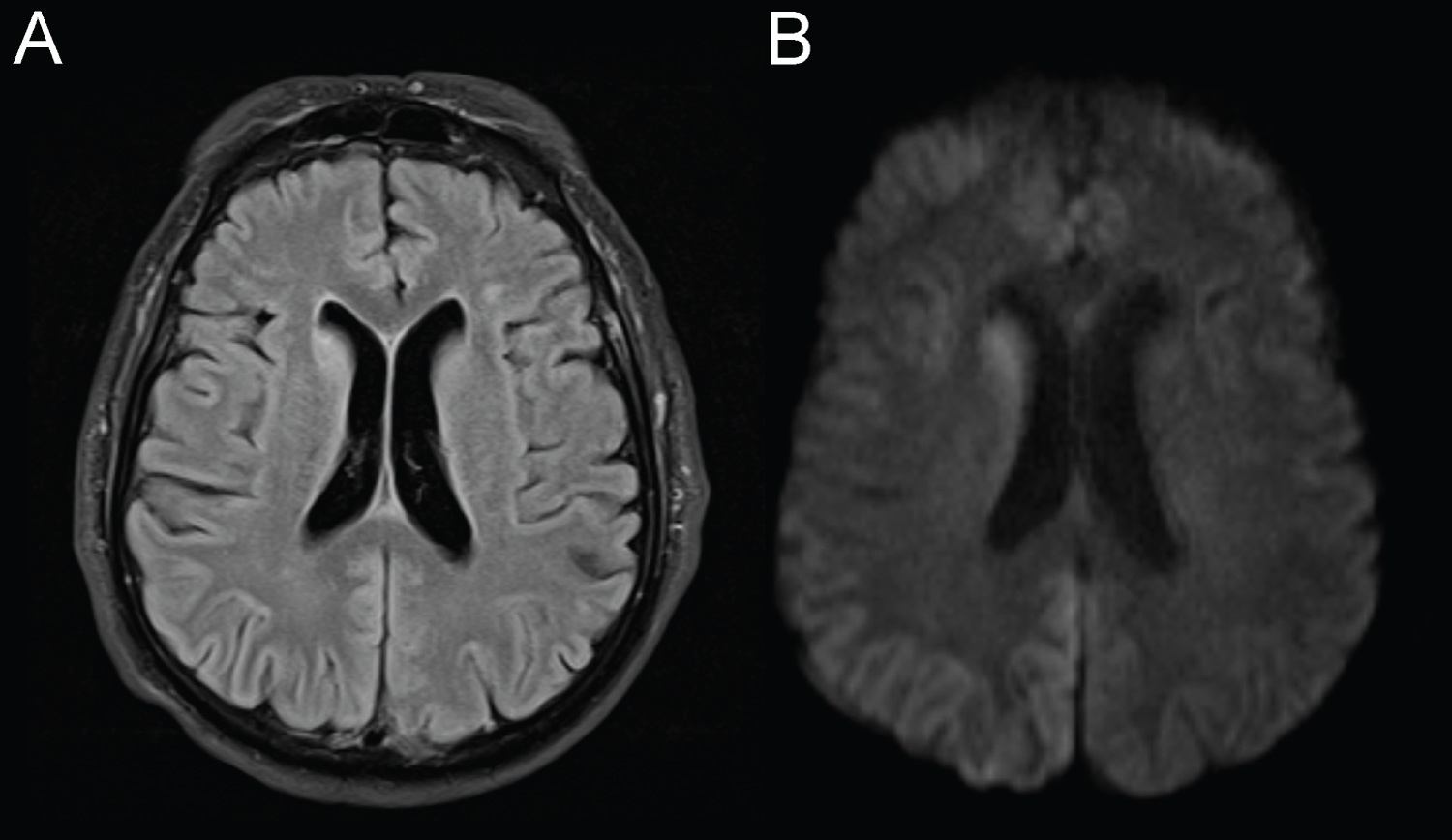 Figure 1: MRI findings. Fluid-attenuated inversion recovery (FLAIR) showing hyperintensity of the right caudate nucleus and cortical ribboning predominantly in parieto-occipital lobes (A). Changes are more apparent in diffusion weighted imaging (DWI). View Figure 1
Figure 1: MRI findings. Fluid-attenuated inversion recovery (FLAIR) showing hyperintensity of the right caudate nucleus and cortical ribboning predominantly in parieto-occipital lobes (A). Changes are more apparent in diffusion weighted imaging (DWI). View Figure 1
In our case the coexistence of visual hallucinations and visual decline initially suggested a diagnosis of Charles Bonnet syndrome. This syndrome is defined as complex visual hallucinations associated with loss of visual acuity due to different ophthalmologic conditions [4]. Hallucinations are often described as complex, stereotyped, persistent or repetitive in nature. They usually are made up of vivid images including people, faces, animals, flowers, among many other objects [5]. Although rigid diagnostic criteria are lacking, patients usually maintain insight into the unreality of their visual hallucinations, which are commonly pleasant but may sometimes cause distress [6]. The prevalence of Charles Bonnet syndrome varies greatly and has been reported between 1 and 10% [7]. The observed differences are probably due to patient selection and differences in screening tools used to detect hallucinations. Interestingly, although cognitive integrity is an often-cited characteristic of Charles Bonnet, a recent study found that up to 26%, from a large series of 77 patients, eventually developed an overt dementia syndrome [8]. In our case, the development of encephalopathy and confusion made the initial diagnostic unlikely and warranted further study.
In contrast, Creutzfeldt-Jakob Disease (CJD) is very rare and fatal neurodegenerative disease induced by the prion protein scrapie (PrPsc). This disease is characterized by rapidly progressive dementia, generalized myoclonus, ataxia, pyramidal and extrapyramidal tracts, and akinetic mutism [9]. An infrequent variant of CJD with early prominent visual symptoms is called the Heidenhain variant. This uncommon phenotype of the sporadic CJD represents 10-20% of cases [10]. The myriad of symptoms owes to the predominant occipital and posterior parietotemporal cortex neuronal loss induced by the PrPsc [11]. Visual symptoms are usually negative and include visual field restriction, visual blurring, or cortical blindness [12]. Few emphases are made into visual hallucinations which are usually mild, non-complex and often referred as metamorphopsia or visual perceptions [13]. Probable diagnosis of CJD is based on suitable clinical manifestations and at least one suggestive finding among typical MRI, typical periodic sharp waves on EEG or positive CSF 14-3-3 protein. Until recently, definitive diagnosis required neuropathological confirmation. Now a definite diagnosis can also be immunohistochemically or biochemically confirmed [14] RT-QuIC has been shown to have modest sensitivity (about 77% to 92%) but very high specificity (99% to 100%) for PrPsc detection in CSF [15].
To the best of our knowledge this is the first case to present a CJD initially diagnosed as a Charles Bonnet Syndrome. It is therefore possible that some patients with dementia manifest complex visual hallucinations in the early stages of the illness and they may be inappropriately diagnosed. In this case, striking early preservation of cognitive function and the absence of encephalopathy completely misled the initial diagnosis into a relative being condition. This highlights the importance to consider that complex visual hallucinations can be the first manifestation of a fatal neurodegenerative process.
The authors declare no conflicts of interest. No funding was received for this work.
All authors participated equally in the evaluation of the patient and the elaboration of the manuscript.