Objective: This study is to analyse the fall in haemoglobin concentration following various commonly used surgical procedures to repair hip fractures, analysing its relationship with pre-existing co-morbidities, post-operative complications, length of stay and 30 day mortality.
Material and methods: A retrospective analysis of neck of femur fracture patients looking at their pre-operative and pre-discharge haemoglobin levels taking into consideration co-morbid conditions and possible adverse effects including 30 day mortality occurring during the perioperative period.
Results: Two hundred and thirty one patients (160 females 69.3%) with fracture neck of femur and anaemia were identified. The mean age was 84.2 years. Pre-operatively 31.6% had moderate/severe anaemia compared to 71% post-operatively. The drop in Hb was most significant in patients who had arthroplasty procedures. The 30 day mortality in pre and post-operative anaemia patients was 18.6% (43 patients), of which 21 patients (48.8%) and 22 patients (51.1%) were in the moderate/severe anaemia group respectively (p = 0.01).
Conclusion: Identification of anaemia at the time of admission and discharge is important in improving patient outcomes and mortality in hip fracture patients with potential opportunities to proactively managing prior to surgery, as well as in the post-operative period.
Anaemia, Hip fractures, Post-operative, Mortality
The outcomes of proximal femoral fractures in the elderly generally are poor. The poor results are usually associated with pre-existing medical co-morbidities such as anaemia [1,2]. The post-operative drop in haemoglobin in this cohort of patients is often further exacerbated by oral anticoagulants, further loss of blood during surgery, malnutrition and general frailty [3,4]. Even though anaemia can be corrected with allogenic blood transfusion [5] and oral or parenteral iron supplementation [6], anaemia at the time of discharge is still a major risk factor for an increase in 30 day mortality.
Anaemia is defined by the World Health Organization (WHO) as a haemoglobin (Hb) level of < 13 g/dL in men and < 12 g/dL in women [7]. The causes of anaemia in elderly age group is multifactorial, commonly due to iron, folate, vitamin B12 deficiency [8], chronic liver or kidney disease [9] and inflammation [10]. However, in one third of the patients it can be idiopathic [11]. The drop in haemoglobin concentration in patients with hip fractures is attributed to pre-existing anaemia before sustaining the hip fracture [12] or due to bleeding before, during and after surgery [4]. Previous studies has demonstrated that the haemoglobin level before and after surgery is an independent factor associated with increased 30 day mortality in elective general surgical and non-cardiac surgery [13,14].
We aimed to analyse the fall in haemoglobin concentration following various commonly used surgical procedures to repair hip fractures, analysing its relationship with pre-existing co-morbidities, post-operative complications, length of stay and 30 day mortality.
A retrospective study of all the patients admitted with a neck of femur fracture between March 2019 to December 2019 was carried out. The data was obtained from NHFD (National Hip Fracture Database) and internal hospital computer systems (Medway, ICE, Clinic letters). After screening a total of 231 patients above the age of 65 admitted with fractured neck of femur were identified and included in analysis. Patients with bleeding disorders and pathological fractures were excluded from the study.
Patient demographics including age, sex, fracture pattern and pre-existing anaemia were recorded. The co-morbidities including oral anticoagulants at the time of admission were noted, along with the type of procedure which the patient underwent. All the patients received intra-operative tranexamic acid injections.
Female patients with haemoglobin (Hb) concentration ≥ 12 g/L were classified as normal, between 11 to 12 g/L as mild anaemia and those with Hb level ≤ 11 g/L as having severe anaemia. These Hb levels were based on WHO definitions of anaemia at sea level [7]. The drop in Hb at the time of discharge was calculated for individual sex, procedures done for hip fractures, those received post-operative blood transfusions, complications, readmissions, length of stay and 30 day mortality.
Demographic continuous data is presented as means, with standard deviations (SD). Categorical data is presented as the number of subjects in the category, along with proportional percentages. Chi-square test and Fisher's exact test were used for comparing groups of categorical data. Differences between the means of continuous data were compared using unpaired t-tests or one-way ANOVA. The strength of relationships between variables was estimated using Spearman's rank correlation. A P value < 0.05 was taken as the threshold of statistical significance. The data were analyzed using IBM SPSS Statistics version 26.
A total of 231 patients with neck of femur fractures and anaemia were identified. The mean age was 84.2 years (range 60-100). The male female ratio was 71:160. The pre-operative co-morbidities recorded included cardiac diseases (53.23%), COPD (55.24%), kidney disease (42.18%) and malignancies (28.12%). 63(27.4%) patients were taking oral anticoagulants on admission. There were 138 (60%) patients with intracapsular fractures and 93(40%) with extracapsular fractures.
The procedures performed were hemiarthroplasty 119, Dynamic hip screw fixation (DHS) 52, Intramedullary nail (IM) 41 and Total hip replacements (THR) 19 patients. Post op blood transfusions were given to 32(13.9%) patients, Table 1.
Table 1: Baseline patient demographics. View Table 1
There was no significant difference in drop of Hb between males and females, Table 2. There were 57 (24.7%) patients had borderline anaemia and 73 (31.6%) patients had severe pre-operative anaemia respectively. But in the post-operative group there was a significant rise in the number of patients with severe anaemia 164 (71%), Table 3. The fall in Hb was assessed against the surgical procedure performed using one way ANOVA tests which showed a significant mean fall in Hb in patients who had arthroplasty (THR-2.94 g/L and hemiarthroplasty-2.07 g/L), Table 4. Multiple comparisons using Bonferroni correction test showed that total hip replacement procedure had significant fall in Hb levels compared to other procedures, Table 5.
Table 2: No significant difference for drop in haemoglobin for gender. View Table 2
Table 3: Pre and post-op anaemia details. View Table 3
Table 4: One way ANOVA test to calculate mean drop in Hb for indivudual procedures for hip fracture treatment. View Table 4
Table 5: The THR group has significant drop in Hb than Hemiarthroplasty, DHS and IM nail (p value < 0.05). View Table 5
The correlations between the kind of operation and postoperative blood transfusion shows a significant correlation, most of the transfusion were in patients who had THR and IM nail, Table 6.
Table 6: Post-operative blood transfusion for the operations performed. View Table 6
No significant differences for fall in Hb and incidence of postoperative stroke, postoperative cardiac event, and respiratory infections, postoperative wound infections and anticoagulant therapy was demonstrated. The average length of stay was 17.14 days. Both regression and ANOVA analysis did not show any relation between length of stay and post-operative drop in Hb in all three groups (p = 0.469), Table 7.
Table 7: The length of stay in all three anaemia groups. View Table 7
The 30 day mortality in pre and post-operative anaemia patients was 18.6% (43 patients), of which 21 patients (48.8%) and 22 patients (51.1%) were in the severe anaemia group on admission and post-operatively respectively (p = 0.01), Table 8a and Table 8b. The 30 day mortality with 95% CI for all three groups of pre and post–operative anaemia are shown in Figure 1 and Figure 2. The statistical analysis shows that the 30 day mortality in severe anaemia group is higher in patients with pre and post-operative anaemia.
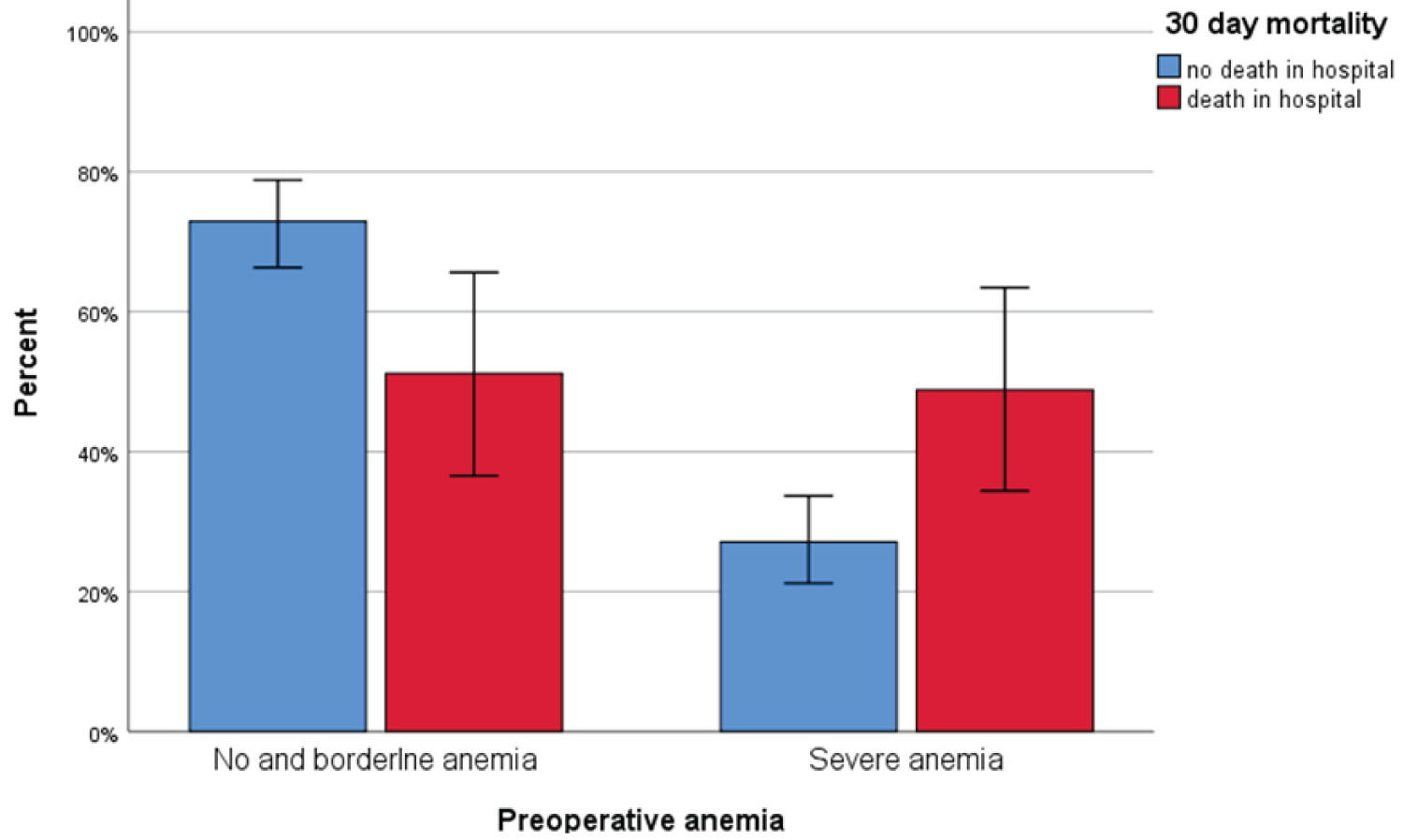 Figure 1: 30 day mortality for all three groups of pre-operative anaemia (Error bars 95% CI).
View Figure 1
Figure 1: 30 day mortality for all three groups of pre-operative anaemia (Error bars 95% CI).
View Figure 1
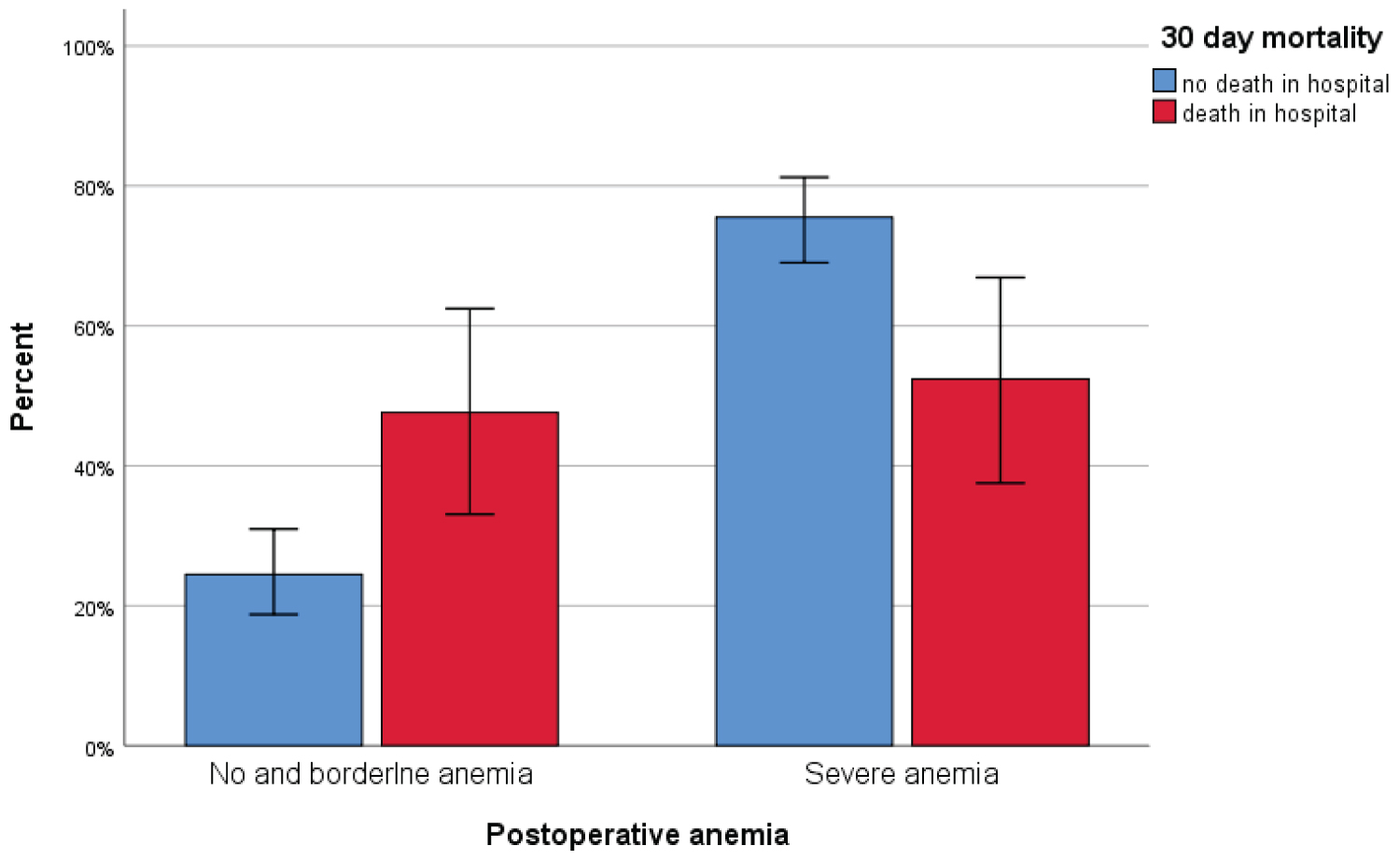 Figure 2: 30 day mortality for all three groups of post-operative anaemia (Error bars 95% CI).
View Figure 2
Figure 2: 30 day mortality for all three groups of post-operative anaemia (Error bars 95% CI).
View Figure 2
Table 8a: Significant 30 day mortality in patients with severe pre-operative anaemia (p = 0.01). View Table 8a
Table 8b: Significant 30 day mortality in patients with severe post-operative anaemia (p = 0.01). View Table 8b
In our study 56.3% of patients had pre-operative anaemia which is slightly higher than the other studies [15,16]. The advancing age in our group (mean = 84.2 years) of hip fracture patients may be a contributing factor for the high incidence of pre-operative anaemia [3]. In elderly patients there is abnormal regulation of proinflammatory cytokines, which inhibits haemopoesis either by reducing erythropoietin production or impaired erythropoietin receptor function [17]. The prevalence of pre-operative anaemia was independent of gender and fracture pattern in our study.
The significant co-morbidities recorded in our study were COPD, cardiac diseases, chronic kidney diseases and malignancies. There were 27.4% of patients taking oral anticoagulants on admission. The factors contributing to pre-operative anaemia with existing co-morbidities are multi-factorial mediated by cytokines such as interleukin-1 [IL-1], IL-6, tumour necrosis factor-a [TNF-a] [18]. These factors regulate the secretion and action of erythropoietin and median red blood cell survival [9,10]. In patients with chronic kidney disease the cause of anaemia are due to decrease in erythropoietin and glomerular filtration rate [19].
The post-operative drop in Hb in our series was quite significant demonstrated in 86.2%. Our results are similar to the study by Halm, et al. who has found that the incidence of post-operative drop in Hb was 84.6% [3]. Those patients who underwent arthroplasty procedures such as total hip replacement and hemiarthroplasty had the substantial drop in Hb levels (THR-mean drop of 2.94 g/L and hemiarthroplasty-mean drop of 2.07 g/L). This is in full agreement with previous studies on drop in Hb levels after lower limb arthroplasty [20]. The causes for the drop of post-operative Hb can be due to several factors such as duration of surgery and the type of the procedure [1]. Arthroplasty procedures take longer surgical time hence more blood loss.
In our study patients who had most post-operative blood transfusion were those who underwent total hip replacement (26.3%) and intramedullary nailing procedures (22%). Morris, et al. [21] in their study on allogenic blood transfusions for fracture neck of femur surgery concluded that the incidence of post-operative blood transfusion is 20.8% for those patients who underwent total hip replacement and 67.4% who had intramedullary nailing. But various authors have described decreased blood loss [22], increased blood loss [23] and no difference [24] in patients who had intramedullary nailing for hip fractures.In an already co-morbid population, an allogenic blood transfusion is not without significant risk and can contribute towards morbidity and mortality.
Choi, et al. [25] in their study found that a post-operative haemoglobin level between 8 g/dl and 10 g/dL did not affect the length of stay in the hospital. But Willems, et al. [26] have reported that higher postoperative haemoglobin levels predict shorter length of hospital stay after hip fracture surgery in the elderly. In our study the length of stay in the hospital did not show any statistically significant association was found between patients who had normal and low Hb levels post-operatively.
There are several studies which have also shown an association between pre admission Hb and the mortality following fracture neck of femur. Gruson, et al. [12] reported an increased mortality in patients, who were anaemic on admission. Similarly, Halm, et al. [3] showed Hb to be animportant predictor of mortality and re-admissions within 60 days. Greatorex and colleagues [27] also found low Hb on admission to be predictive of mortality at 6 months. Bhaskar, et al. reported comparable lower mortality in males and females with normal Hb (21.1% and 20.0%, respectively with p-value 0.873) compared with higher mortality rates between anaemic males and females (43.6% and 36.2%, respectively with p-value 0.258) [28]. In our study, we found that the overall 30 day mortality was 18.6%, but in severe anaemia group the mortality was 48.8% in pre-op and 51.1% in post-operative groups respectively (p = 0.01) which is highly significant.
The limitation of this study is that it is a retrospective analysis. The sample size is small and the results are calculated for 30 day mortality. However we looked at all the confounding variables that can affect the haemoglobin level both pre and post-operatively. The significance of our results has made a foundation for future studies with large sample size, one year mortality and correction of reversible factors affecting the pre and post-operative anaemia in hip fracture patients. Although there are several guidelines regarding the management of anaemia during the pre-operative assessment of elective orthopaedic surgery, in elderly hip fracture patients the guidelines are unclear regarding the treatment of pre and post-operative anaemia. Future randomised trials should be done looking at the results of treatment of pre admission and post-operative anaemia and its effects on perioperative and one year mortality in hip fracture patients as we feel this may present with potential opportunities to proactively manage anaemia prior to surgery, as well as in the post-operative period with a view to reducing the mortality risk.
Our analysis has shown a significant number of patients were discharged from the hospital with moderate/severe anaemia. The 30 day mortality in this group of patients is above 50%. We also found that there was significant drop of Hb in the post-operative period in patients undergoing arthroplasty procedures for hip fractures. We recommend that in patients undergoing hip fracture surgery both pre and post-operative anaemia should be corrected with adequate and appropriate interventions to decrease morbidity and mortality.