Total extrusion of the talus with disruption of all the ligaments is called "missing talus". It is a rare injury, associated with severe soft tissue damage and/or fracture. It is a tri-articular dislocation involving talotibial dislocation from above, subtalar joint below and talonavicular joint anteriorly. We present a report of a patient treated with immediate reimplantation and K-wire stabilisation leading to a successful outcome.
A 57-year-old tourist had a closed anterolateral extrusion of the talus with a displaced medial malleolar fracture. There was no associated talar fractures. Initial attempts at closed reduction failed. He underwent immediate reimplantation surgery and K wire stabilisation across the talo-calcaneal (sub-talar) and talo-navicular joints. There was a soft tissue interposition preventing initial reduction by the extensor digitorum tendon. This had to be released to secure accurate anatomical reduction. He had a good outcome with full function of the ankle joint.
The preferred surgical approach in the management of total extrusion of the talus is immediate reimplantation to ensure minimal disruption to the blood supply. However, it must be emphasised that soft tissue interposition prevents timely reimplantation and is likely to delay definitive treatment.
Talus, Total extrusion, Reimplantation, Soft tissue interposition, Osteonecrosis
Total talar extrusion is a rare injury. These are mostly associated with open fractures, talar fractures, foot and ankle fractures. A recent systematic review reported only13 cases of closed talar dislocation to date [1]. Open talar extrusions occur in 0.06% of all dislocations and only 2% of talar injuries [2]. Talar dislocation could be mono, bi or tri articular; whereas a total talar extrusion is tri-articular i.e. the dislocation of the talus from the talocrural, talocalcaneal and talonavicular joints - total talar dislocation (TTD) [3,4]. It is a result of high-energy impact on foot [5] either in supination or pronation, coupled with a plantar flexion force [1]. This causes either an anterolateral or posteromedial dislocation [6]. This requires immediate reduction, (open or closed) to prevent further damage. Avascular necrosis and infection of the talus are the significant complications in this type of injury [7]. We report on a closed anterolateral total extrusion of talus and medial malleolar fracture with discussion on management of the soft tissue interposition blocking prompt reduction. There are favourable reports with closed reduction of TTD without associated talar fractures [8,9].
57-year gentleman, visitor from USA, fell off a 3 feet height while climbing onto a post. He sustained an isolated, eversion injury of his left foot and ankle and presented with a grossly deformed ankle. On physical examination, the foot was in eversion and planter flexion. The skin over the lateral aspect was stretched with 5 mm puncture wound. The talus head and body was palpable laterally but not visible through the wound (Figure 1). There was no neurological deficit. Dorsalis pedis and posterior tibial pulses were felt adequately.
 Figure 1: Lateral dislocation of talus; foot in equinus and supination, puncture wound on the skin.
View Figure 1
Figure 1: Lateral dislocation of talus; foot in equinus and supination, puncture wound on the skin.
View Figure 1
Plain radiographs showed a posterolateral dislocation of talus with a medial malleolus fracture (Figure 2). CT scans showed a tri-articular dislocation with total extrusion of the intact talus from the tibio-talar, talo-calcaneal and talo-navicular joints (Figure 3). There was an associated displaced medial malleolar fracture but no other occult fractures or intra-articular fragments (Figure 4).
 Figure 2: Antero-posterior and lateral radiographs of total lateral talar dislocation.
View Figure 2
Figure 2: Antero-posterior and lateral radiographs of total lateral talar dislocation.
View Figure 2
 Figure 3: CT sagittal view: Total talar dislocation (TTD) with dislocation of sub-talar, talonavicular, and tibiotalar joints.
View Figure 3
Figure 3: CT sagittal view: Total talar dislocation (TTD) with dislocation of sub-talar, talonavicular, and tibiotalar joints.
View Figure 3
 Figure 4: CT coronal view of the foot showing an associated medial malleolar fracture.
View Figure 4
Figure 4: CT coronal view of the foot showing an associated medial malleolar fracture.
View Figure 4
Closed reduction was attempted in the resus room under propofol sedation by the on-call trauma team. This was unsuccessful. The circulation was intact. According to the British Orthopaedic Association Standards for Treatment of Open fractures (BOAST) guidelines [10] for management of open fractures and joint injuries, the open wound was debrided under general anaesthesia, with prophylactic antibiotic and tetanus toxoid booster cover (BOAST). An attempted initial closed reduction under general anaesthesia was unsuccessful. A Steinman pin was inserted into the calcaneum to enable traction during open reduction. Through an anterolateral skin incision over the ankle joint, the talus was exposed (Figure 5).
 Figure 5: Anterolateral skin incision over the ankle with the extruded talus.
View Figure 5
Figure 5: Anterolateral skin incision over the ankle with the extruded talus.
View Figure 5
It was noted to be extruded anterolaterally with the extensor tendons tenting over the head of the talus. There was total disruption of the tibio-talar, talo-calcaneal (sub-talar) and talo-navicular joints. There was an associated displaced medial malleolar fracture. After careful dissection of the soft tissues, a capsulotomy was performed and it was noted that the extensor digitorum brevis was blocking the reduction. This had to be divided to enable reimplantation under traction (Figure 6).
 Figure 6: Soft tissue interposition (extensor digitorum brevis) blocking reduction.
View Figure 6
Figure 6: Soft tissue interposition (extensor digitorum brevis) blocking reduction.
View Figure 6
A K-wire each was inserted through the talo-calcaneal and talo-navicular joints under fluoroscopy to ensure stability. The medial malleolar fracture was stabilised with 2 partially threaded cancellous screws (Figure 7).
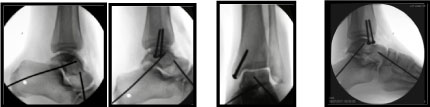 Figure 7: Intra-operative radiographs of K-wire stabilisation and Medial malleolar fixation.
View Figure 7
Figure 7: Intra-operative radiographs of K-wire stabilisation and Medial malleolar fixation.
View Figure 7
Post-operative CT scans showed good reduction and alignment of the talus and medial malleolar fracture (Figure 8). Patient was followed up in clinic a week after discharge. Sutures were removed and wound healing was satisfactory. The cast was removed and patient was mobilised in air cast boot and crutches and he flew back to the USA after 2 weeks.
 Figure 8: Post op CT scan showing anatomical reduction of the talus and internal fixation of medial malleolus.
View Figure 8
Figure 8: Post op CT scan showing anatomical reduction of the talus and internal fixation of medial malleolus.
View Figure 8
Isolated closed talar extrusions are rare, and the injury is often associated with malleoli fractures [11]. It is suggested that medial malleolar hypoplasia, peroneal muscle weakness, ligamentous laxity, previous sprains and lack of coverage of the talus puts the ankle at risk for a dislocation [12]. Fahey and Murphy described talar dislocations in relation to anterior, posterior, medial, lateral, and upward direction of the displacement as well as the combined forms [13]. Leitner, et al. [14] described a 3-stage mechanism; stage one: Dislocation of subtalar joint, followed by talonavicular and total talar extrusion [14]. In our report, the patient had his foot in supination on landing resulting in a closed anterolateral total talar dislocation (TTD). Most of these patients are treated by immediate closed reduction [15], however in our case this could not be achieved due to extensor digitorum brevis blocking the reduction.
This required open reduction after an unsuccessful closed reduction attempt. The totally extruded talus was managed by immediate reimplantation and stabilisation by 2 retrograde K-wires across the talo-calcaneal and talo-navicular joints [16]. We used Steimann pins through the calcaneum to assist joint distraction to facilitate reduction [17].
Open reduction has resulted in frequent complications like avascular necrosis and osteomyelitis affecting 38-85.7% of cases [4,18,19]. Delayed intervention leads to skin necrosis requiring sural fasciocutaneous island flap [20]. There is no evidence-based strategy in the management of TTD. However, immediate reimplantation is the first-line of treatment. The goal is to achieve anatomical reduction and stability. This must be achieved in a time bound manner to prevent infection, osteonecrosis [21] and osteoarthritis at a later stage [19,22]. Many authors have reported soft tissue interpositions like joint capsule [23,24], tibialis posterior tendon [16], extensor retinaculum [25], Flexor hallucis and digitorum longus tendon [18], dorsalis pedis [26]. This may cause delay in the definitive treatment and must be anticipated. Careful consideration of soft tissues, minimal osteosynthesis with K-wires, initial immobilisation does improves blood flow to the soft tissues due to reduced post-operative odema [27]. In the past, immediate tibiocalcaneal arthrodesis was usually favored over reimplantation [4,28]. However, subsequent sporadic reports of favorable outcomes with reimplantation led to the exploration of reimplantation as a first-line treatment [7]. Gerken, et al. had suggested that with immediate reimplantation and follow up care, AVN should be delayed as long as possible [29]. Kwak, et al. reported revascularisation of a completely extruded talus with serial MRI scans after prompt reimplantation. They did not report any soft tissue problems in achieving the desired outcome [30]. A systemic review in 2015 reporting on 39 articles with 86 cases showed that 84% had open injuries and 12% had associated fractures other than talus. 25% underwent secondary arthrodesis. Good outcomes were reported in a third, 25% developed AVN, and 16% progressed to clinically significant secondary osteoarthritis [7].
The current trend in the management of this injury is immediate reduction, re-implantation and stabilisation of the total talar dislocation (TTD). Soft tissue interposition must be considered for prompt and accurate anatomical re-implantation to prevent or delay AVN. Our report supports this view and this approach will achieve a good to fair result than primary talectomy [31]. The rates for infection and need for secondary procedures are identical. Salvage procedures like talectomy and tibiocalcaneal arthrodesis are reserved for late complications.