Introduction: First branchial cleft anomalies are a rare group of congenital lesions of the head and neck area. Their incidence is quite low, since they account less than 10% of all branchial cleft defects. A wide range of clinical symptoms may occur, but they often are associated with acute infection at the initial diagnosis.
Objective: The aim of this work is to describe and share the case of a 2-year-old patient operated successfully in our department for a first branchial cleft cyst, this by pointing out clinical, radiological features of this entity as well as the surgical approach followed.
Case presentation: This report concerns a 2-year-old patient with a first branchial cleft cyst who presented to the ENT department of the hospital of August 20 in Casablanca, for a recurrent infected right lateral cervical swelling, for whom the clinical examination found a fustulous orifice in the upper right region of the neck. Further investigations confirmed the diagnosis. The patient then underwent surgical removal respecting the facial nerve. No complications were noted in the postoperative period nor in the follow-up.
Conclusion: Because of their rarity and their nonspecific symptoms, first branchial cleft cysts are usually misdiagnosed leading to inadequate management. Thus, recurrences are common and iatrogenic lesions of the facial nerve have been reported on several cases.
Branchial cleft anomalies, First branchial cleft, Fistula, Facial nerve
Branchial cleft anomalies are one of the commonest congenital head and neck lesions following the thyroglossal duct cysts, accounting for 20% of cervical masses in children [1]. In fact, they could be bilateral in 1% of cases, with no site predilection in right or left side [2]. Among the branchial anomalies, first cleft anomalies account only 1 to 4%. The latter arise from an incomplete closure of the ventral portion of the first and second branchial arches, presenting as tracts or masses located in the auricular, periauricular, parotid, or upper neck regions. They manifest as cysts, fistulas, sinuses depending on the degree of the closure [3].
Work’s classification, established in 1972, is the most common used to categorize first branchial cleft cysts or fistulas, where two distinct types are proposed. Type 1 being superficial to the facial nerve is rare, whereas type II the most frequent contracts intimate relation with it [4].
We will be describing in this report the case of a type II first branchial cleft cyst in a 2-year-old patient and its successful excision, while emphasizing its clinical, radiological features as well as the surgical challenge faced.
A 2-year-old infant without any past particular medical records was referred to the Otolaryngology - Head and Neck Surgery department in December 2020 for repeated episodes of right lateral cervical infected swelling. These episodes began at the age of 4 to 5 months, and were treated by oral antibiotics with good clinical improvement but relapsed soon after. No particular family history was recorded. The mother denied fever and night sweats.
Physical examination at the time of initial consultation at our institution revealed normal tympanic membranes bilaterally, a disgracious subcutaneous induration with an approximate diameter of 10 mm, below the right mandibular angle giving frank pus after its pressure. No further sign was found, particularly no orifice at the level of the right external auditory canal nor a contralateral location or an associated malformation. General physical examination also revealed no pathologic findings.
The diagnosis of first branchial cleft cyst was considered. The patient benefited then from an ultrasound examination which was not 100% conclusive. Investigation was completed by a computed tomography CT cervical examination objectifying the presence beside the right mandibular angle of a subcutaneous formation, quite well limited, isodense, discreetly enhanced at the periphery after injection measuring 6.3 * 7 mm. This formation appears to communicate through a channel with the ipsilateral parotid gland. No lymphadenopathy of significant size was found. Subsequently, CT scan data concluded to a right cyst type II of the first branchial cleft (Figure 1 and Figure 2).
 Figure 1: Coronal and Sagittal CT scan cuts concluding to a right first branchial cleft communicating with the ipsilateral parotid gland.
View Figure 1
Figure 1: Coronal and Sagittal CT scan cuts concluding to a right first branchial cleft communicating with the ipsilateral parotid gland.
View Figure 1
 Figure 2: CT scan axial cuts.
View Figure 2
Figure 2: CT scan axial cuts.
View Figure 2
Total resection of the fistula was suggested with a potential risk of facial nerve palsy explained to the family. After, they consented to the surgery; the patient underwent a surgical excision under general anesthesia.
A parotidectomy incision by Modified Blair’s incision was made. The skin flaps were lifted. The first step was to identify the main trunk of the facial nerve and to dissect and identify its branches. Through a careful dissection by staying close to the fistula tract and following it with the facial nerve visualised throughout the procedure, the fistula tract was followed till its end where we tied it up (Figure 3).
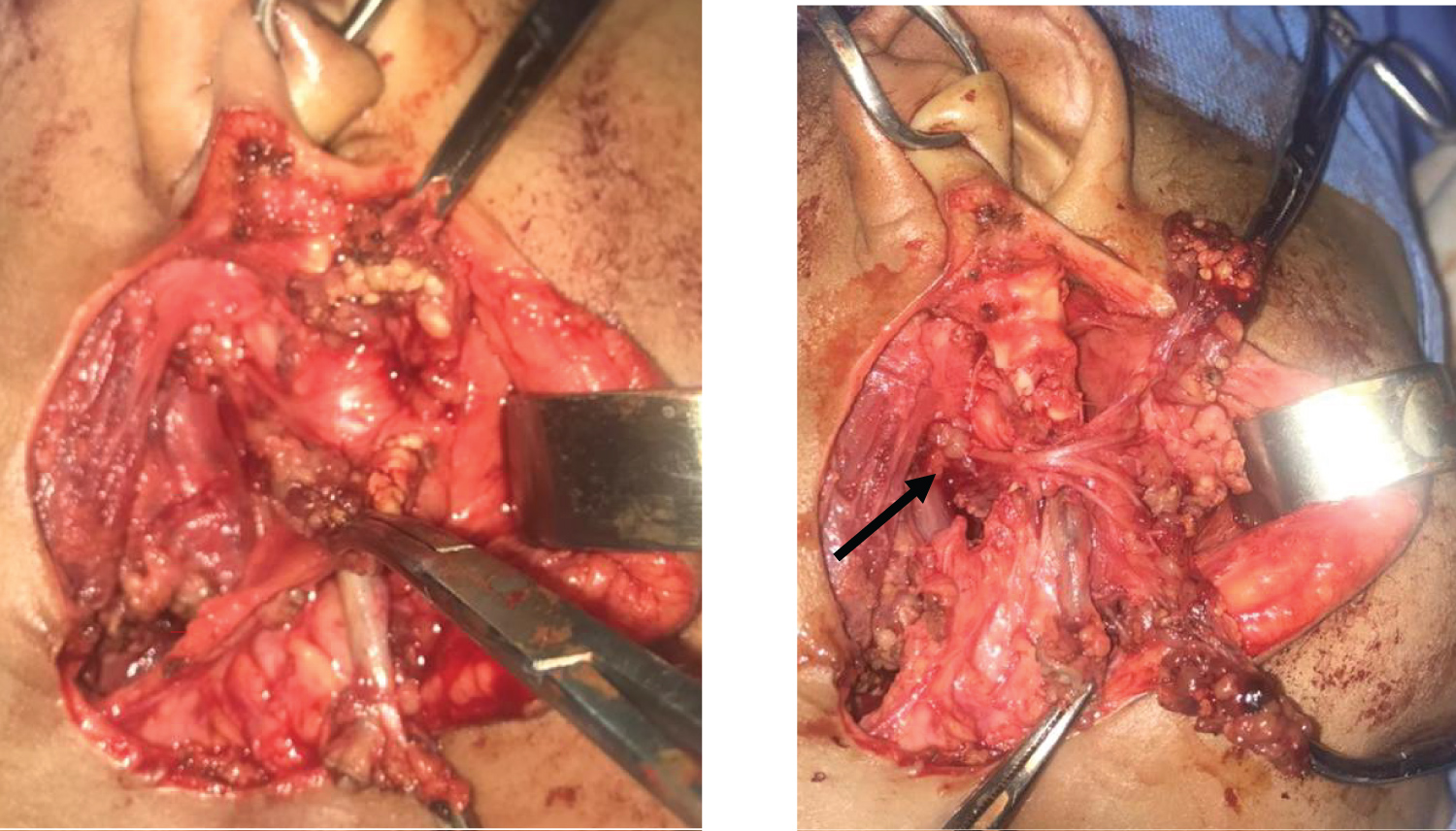 Figure 3: After a modified Blair incision, the facial nerve and its branches are identified; then dissection (Black arrow: Facial nerve trunk and its branches) follows the fistula's tract till its end.
View Figure 3
Figure 3: After a modified Blair incision, the facial nerve and its branches are identified; then dissection (Black arrow: Facial nerve trunk and its branches) follows the fistula's tract till its end.
View Figure 3
Then a closure of the plans was carried out leaving a redon drain in place. No complications were recorded in the postoperative period, in particular neither hematoma nor facial paralysis. The patient was discharged 2 days after surgery after drain removal. Regular follow-up showed complete remission and satisfactory clinical outcome.
First described in 1832, by Ascherson, branchial cysts are rare [1]. In fact, by the 4 th week of the embryonic life, six branchial arches are recognizable. Five pairs of clefts and five branchial pouches separate these six arches, with a membrane located at the interface between the pouch and the cleft. Each arch is the embryological precursor of certain structures of the face, neck, and pharynx [2]. Branchial anomalies can be divided into first cleft, second cleft, third, and fourth pouch anomaly. Indeed, the embryonic origin of these lesions ultimately dictates their clinical presentation, the diagnosis as well as the correct surgical treatment.
The first branchial cleft anomalies represent a rare group of congenital anomalies accounting less than 8% of the overall incidence of branchial cleft defects [6]. They may present as cysts, fistulas, sinuses or cartilaginous remnants. Symptom occurs in the periauricular and upper lateral cervical region located above a horizontal plane passing through the hyoid bone. They manifest very often as recurrent swelling or abscess, erythema and pain around an identifiable opening [7].
Arnot in 1971, Work in 1972, defined two distinct types of anomalies involving the first branchial cleft [8]. Since then, Work’s classification is the most used based on clinical and histological features: Type I anomalies present as a cystic swelling and are purely ectodermal, while type II anomalies present as a cyst, sinus, or fistula or any combination thereof. The latter is of ectodermal and mesodermal origin [9].
Diagnosis is based on the awareness of the condition as well as a careful examination. Ultrasonography, CT and MRI scans are useful investigations to confirm the diagnosis and define the extent of the lesion. Indeed, the scan helps the surgeon to delineate the lesion. It also may be useful in evaluating its relation with the facial nerve especially with the MRI known to perform well at exploring soft tissues [10].
Surgical excision is considered the most proper treatment. It is based on the complete removal of the cyst and any associated fistulous tract, given the high rate of recurrence if partial excisions are made or any tissue is left behind [11].
According to the literature, the recommended surgical technique begins with an incision used for parotid tumors excisions, followed by a careful exposure of the facial nerve and complete mass resection while avoiding the nerve’s lesion [12]. In fact some authors recommend injecting blue of methylene to follow the fistula tract, while others recommend performing a partial or superficial parotidectomy because of the intimate relationship between the facial nerve and the lesion [13].
Facial nerve injuries temporary or permanent are the most dreadful complication, besides recurrences if the excision was incomplete, infection or hematoma as the case of any surgery [9]. In our case, neither recurrence nor facial nerve complication was found.
In a nutshell, first branchial cleft anomalies are a rare condition, manifesting as cysts or fistulas. Diagnosis is based on the interrogation and a thorough clinical examination. Indeed, imaging tools are a great help for the surgeon to confirm the diagnosis as well as to guide the surgery which is the mainstay of treatment based on the complete removal of the lesion not letting any tissue behind.