Background: Spontaneous pneumomediastinum (SPM) is rare complication of labor that has been associated with the Valsalva maneuver. While the available literature has elucidated the appropriate diagnosis and management, no reports have commented on patient position as a risk factor for the development of SPM.
Case: Herein we present the case of a healthy 29-year-old primigravida who had a spontaneous term vaginal delivery complicated by postpartum development of pneumomediastinum with mild pneumothorax, after pushing in an inverted hands-and-knees position for 3 hours. She was managed conservatively and experienced complete resolution of symptoms without intervention.
Conclusions: We argue that the inverted hands-and-knees position alters intrathoracic pressure dynamics in a similar manner to the effect of Trendelenburg position on ventilation. We suggest that performing the Valsalva maneuver in this position could increase risk of pulmonary barotrauma, and propose that this is a topic on which further research is indicated.
Spontaneous pneumomediastinum (SPM) is phenomenon characterized by alveolar rupture and accumulation of air in the mediastinum and subcutaneous tissue without precipitating event. A rare presentation of SPM, sometimes referred to as Hamman’s syndrome, is specifically associated with labor, particularly with the Valsalva maneuver commonly used in the second stage of labor. Case literature cites an incidence of 1/30,000 - 1/100,000, with reports of SPM arising both during and after labor. Recurrence rates are currently unknown. Patient presentation commonly includes subcutaneous emphysema, swelling of the soft tissue of the head and neck, and chest pain or discomfort. SPM can be associated with pneumothorax, but this is usually mild and does not require invasive intervention. Management of SPM is conservative in nature consisting of supportive care, although uses of supplemental oxygen and bronchodilators have been reported [1-8].
While the available case literature on this rare condition has elucidated the classic presentation, differential diagnosis, evaluation, and management of SPM, to our knowledge no case reports have discussed the role of patient position as part of pathogenesis. In this paper, we present the case of a healthy 29-year-old primigravida who had a spontaneous vaginal delivery at term that was complicated by postpartum development of pneumomediastinum with mild pneumothorax. The second stage of her labor was remarkable for pushing exclusively on hands-and-knees with her head in a steep dependent position for several hours; we suggest that this inverted hands-and-knees position may have contributed to the development of SPM. We argue that further research into the role of patient position of SPM is warranted and that patient position should be considered as a possible risk factor.
A gravida 1 para 0-0-0-0 in her 20s presented to Labor and Delivery at 39 weeks 3 days gestation with pre-labor rupture of membranes and was admitted for expectant management, with plan to await spontaneous labor. Her pregnancy was uncomplicated, and she had no significant past medical history with no history of asthma, other pulmonary disease, or connective tissue disease. She reported no history of tobacco or other inhalant use. After several hours from admission without onset of labor, induction was initiated with oral misoprostol. She was expectantly managed thereon after demonstrating adequate cervical change without additional induction agent and progressed to fully dilated. She requested no labor analgesia and received none throughout labor. She desired to push in an inverted position throughout the second stage of labor and pushed utilizing a Valsalva maneuver exclusively on hands and knees in a steep head-down position. The duration of the second stage of her labor was approximately 3 hours, after which time she achieved an uncomplicated vaginal delivery of a viable male infant weighing 3380 grams with APGARs of 9 and 9 at 1 and 5 minutes, respectively.
On postpartum day 1, she reported chest, head, and neck discomfort and swelling, as well as a hoarse voice and difficulty swallowing. Her chest pain was pleuritic in nature. Vital signs were stable with > 96% oxygen saturation and normal heart rate. On physical exam, she had normal work of breathing but significant edema with palpable crepitus was noted from the lower face, jaw, neck, down to the chest mid-sternum. There was also audible crepitus on auscultation of the heart, a finding also known as Hamman’s sign, with otherwise normal heart sounds with no evidence of murmur or additional heart sounds. Lungs were clear to auscultation in all lung zones.
With exam findings concerning for air leakage into the subcutaneous tissue, CT and radiographic imaging was sought to evaluate pulmonary structures including the trachea for defects and for other possible sources of chest pain.
Laboratory evaluation revealed that complete blood count and comprehensive metabolic panel were within normal limits. An EKG showed normal sinus rhythm with no rhythm or other abnormalities. CT chest without contrast showed extensive large volume pneumomediastinum that tracked to the bilateral extra-pleural spaces, neck base, and anterior and posterior chest wall, as well as the left greater than right axillae and left upper extremity (Figure 1). Pulmonary interstitial emphysema was identified in the left lower lobe. No cardiovascular abnormalities were noted.
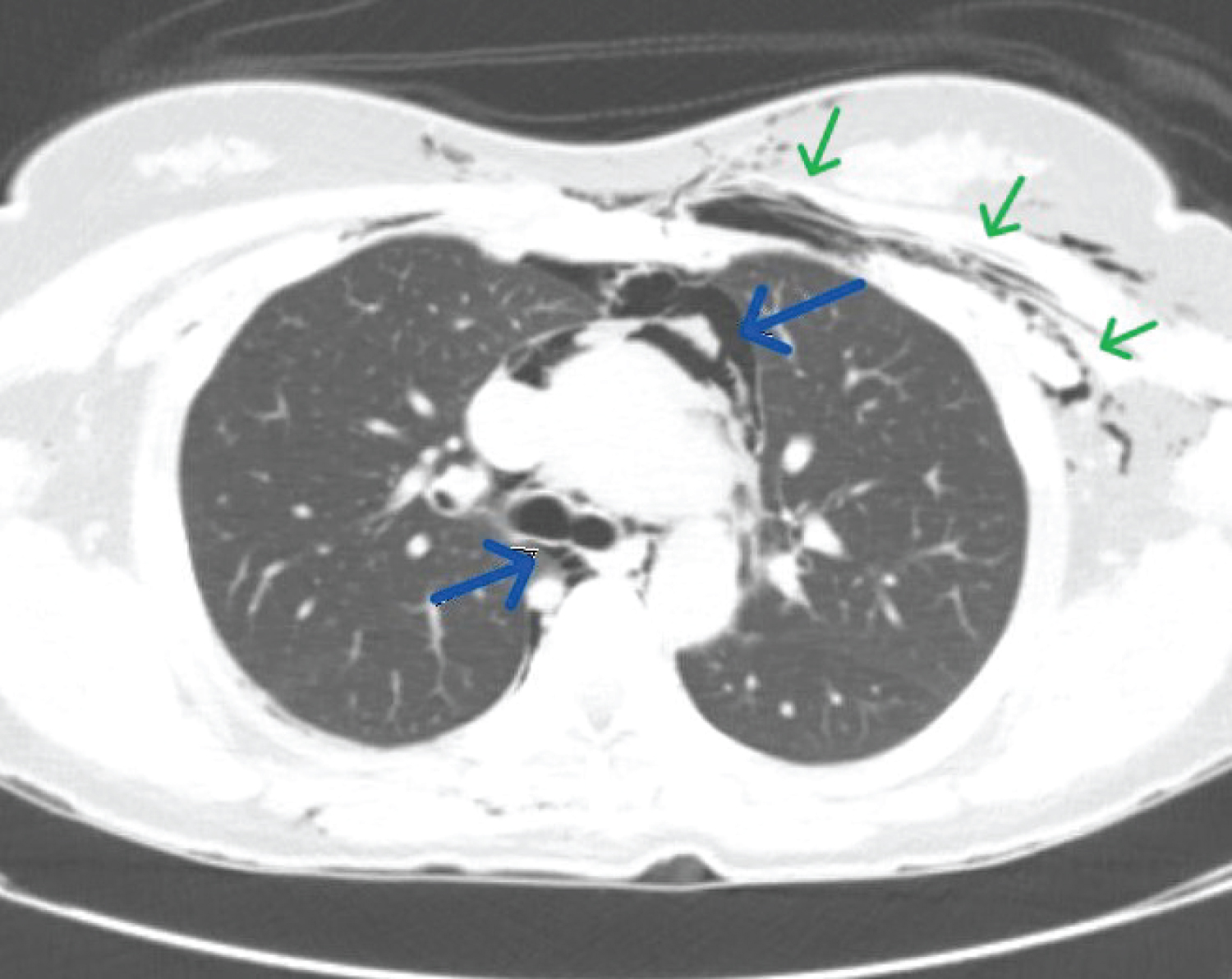 Figure 1: CT chest without contrast, axial slice. Blue arrows indicate large volume pneumomediastinum. Green arrows indicate subcutaneous air along the left chest wall extending into the left axilla.
View Figure 1
Figure 1: CT chest without contrast, axial slice. Blue arrows indicate large volume pneumomediastinum. Green arrows indicate subcutaneous air along the left chest wall extending into the left axilla.
View Figure 1
CT head and neck soft tissue without contrast showed extensive pneumomediastinum with lateral extension into bilateral extra-pleural spaces and extensive subcutaneous emphysema involving the chest wall, neck, face, right temporal, and bilateral occipital scalp. The neck subcutaneous emphysema extended medially to involve the right C5-C6 to C7-T1 neural foramen and right epidural space (Figure 2). No obvious airway or cervical esophageal injury was identified.
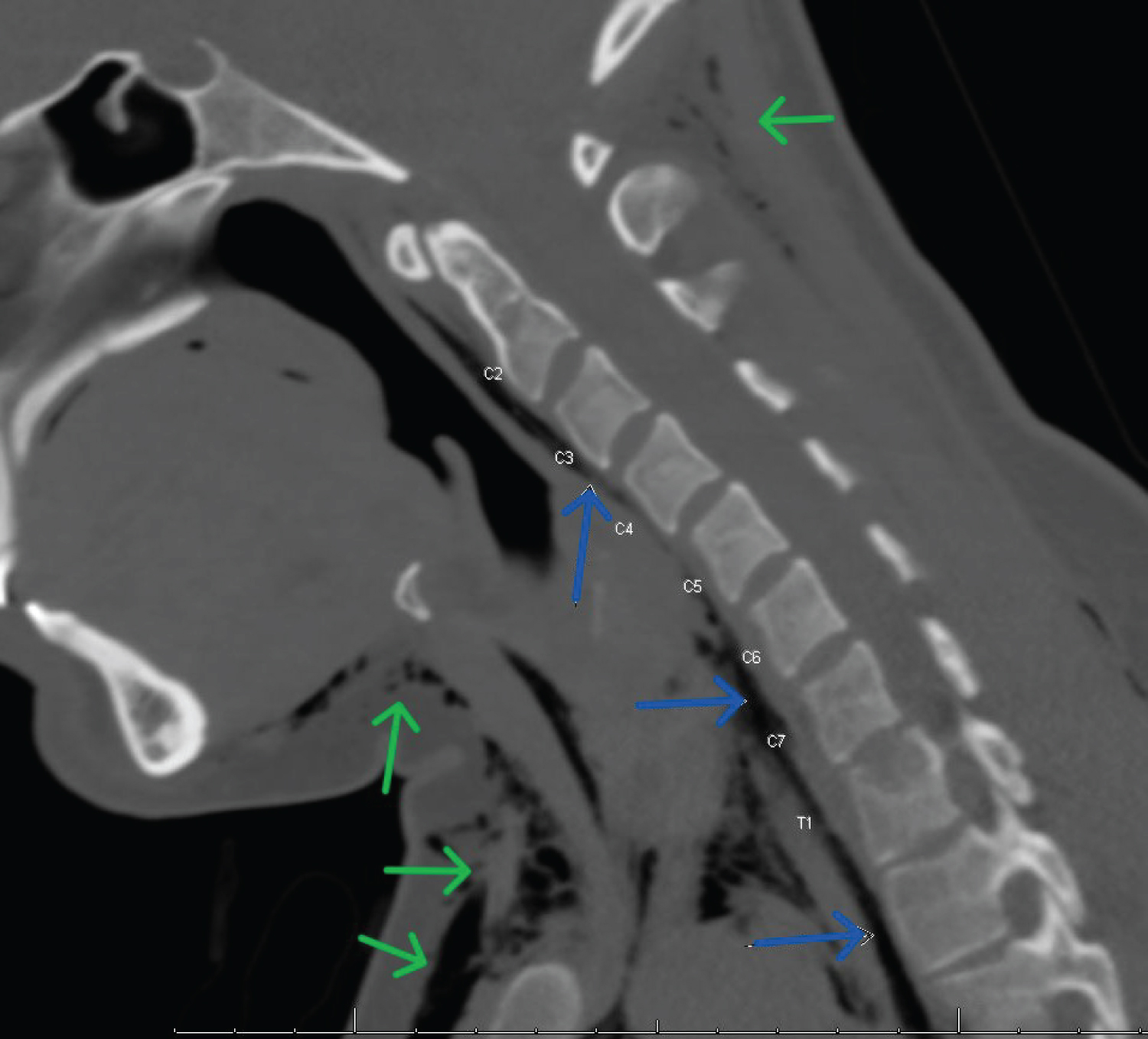 Figure 2: CT neck without contrast, sagittal slice. Blue arrows indicate extensive pneumomediastinum intimate with vertebral bodies and neural foramina. Green arrows indicate subcutaneous emphysema along the anterior chest wall and occiput.
View Figure 2
Figure 2: CT neck without contrast, sagittal slice. Blue arrows indicate extensive pneumomediastinum intimate with vertebral bodies and neural foramina. Green arrows indicate subcutaneous emphysema along the anterior chest wall and occiput.
View Figure 2
A chest radiograph performed on postpartum day 1 showed a trace right apical pneumothorax (Figure 3).
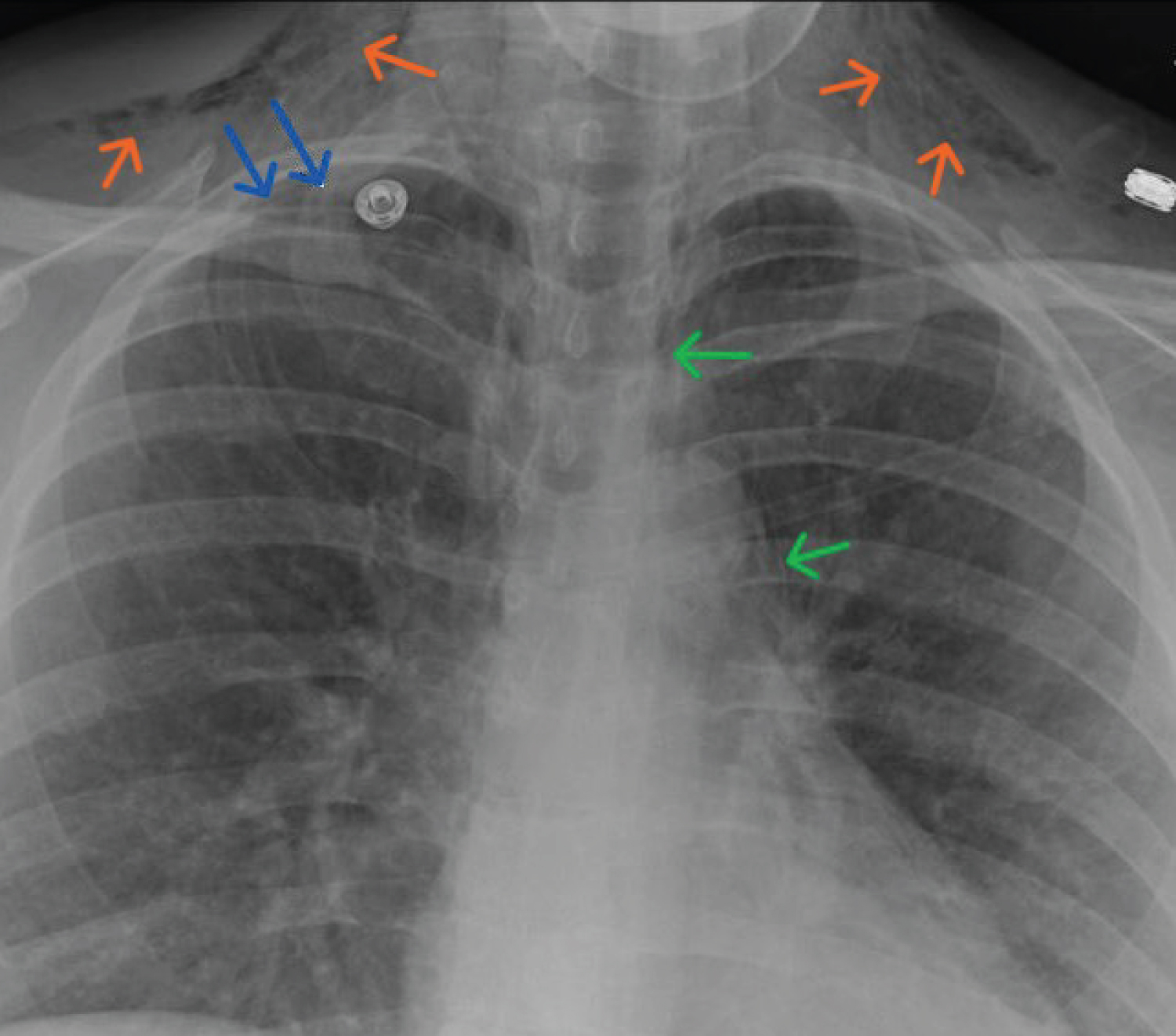 Figure 3: Chest radiograph, AP projection, postpartum day 1. Blue arrows indicate trace right apical pneumothorax. Green arrows indicate pneumomediastinum apparent along the cardiac silhouette. Orange arrows indicate bilateral subcutaneous emphysema in the chest wall extending to the neck.
View Figure 3
Figure 3: Chest radiograph, AP projection, postpartum day 1. Blue arrows indicate trace right apical pneumothorax. Green arrows indicate pneumomediastinum apparent along the cardiac silhouette. Orange arrows indicate bilateral subcutaneous emphysema in the chest wall extending to the neck.
View Figure 3
The patient was managed conservatively with modified bed-rest and administration of 2L supplemental oxygen by nasal cannula. Vital signs were monitored closely and the patient maintained > 96% oxygen saturation and normal hemodynamics throughout hospitalization. The Thoracic Surgery service was consulted and recommended daily chest radiograph while inpatient and continued observation, with no interventions anticipated. Daily chest radiographs showed progressive improvement in the right apical pneumothorax. The patient’s postpartum course was otherwise remarkable only for meeting criteria for gestational hypertension. The patient reported daily improvement in her pulmonary symptoms and she was discharged home on postpartum day 3.
The patient was seen for a check-in visit at 1 week postpartum and reported complete resolution of her symptoms. She was referred to Medical Genetics to discuss the utility of testing for alpha1-antitrypsin gene mutation, with the goal of investigating a possible inciting risk factor for her development of SPM. At the time of publication of this report, the patient has not yet been seen for Genetics consultation. She was also seen by Thoracic Surgery after discharge; she had an additional chest radiograph at 4 weeks postpartum that showed complete resolution of pneumomediastinum and subcutaneous emphysema, and she was cleared by their service with no need for additional follow-up or testing.
SPM is a rare complication of labor about which there is limited clinical information. The proposed pathogenesis of the condition is that the sudden increase in intrathoracic and intra-alveolar pressure from Valsalva leads to alveolar rupture and subsequent leakage of air into the mediastinum and subcutaneous tissue following fascial planes. Case reports have been written about the appropriate diagnosis and management of this rare condition, but to our knowledge no reports have commented on the role of patient position as a possible risk factor [1-8]. The patient presented in this report pushed in an inverted position on hands and knees with her head down for the duration of the second stage of her labor. In consideration of the effect of this inverted position on intrathoracic pressures, we propose that this was a possible contributing factor to the development of SPM in this patient.
To our knowledge, there is no literature available about intrathoracic and intraabdominal pressure dynamics in relation to patient position during the second stage of labor. Given the similarity of the inverted hands-and-knees position to Trendelenburg position, we hope to draw parallels between pressure physiology associated with the latter, which is better studied, and that with hands-and-knees. Studies investigating pulmonary barotrauma in patients undergoing surgery have explored how mechanical ventilation settings are altered in patients positioned in Trendelenburg, reporting increased positive end-expiratory pressure (PEEP) requirement [9,10]. Increasing PEEP is thought to increase risk of barotrauma due to overdistension of the alveoli and accordingly an elevated alveolar pressure as compared to the pressure in the interstitial space [11]. While the pulmonary mechanics of ventilation settings cannot be applied directly to patients in the second stage of labor, the general concept of increased PEEP being required to overcome the effect of inverted position on the thorax is relevant. The Valsalva maneuver can be conceived of as mimicking the effect of increasing PEEP on the thorax [10,12]. With the pressure of the gravid uterus on the thorax in an inverted position causing restriction of the intrathoracic space and increasing airway resistance, we anticipate that the Valsalva effort would be increased to counteract these changes [13]; this may be part of the reason why some patients feel they push with greater efficacy on hands and knees. Thus, if increased Valsalva effort is likened to increased PEEP in Trendelenburg, the risk of pulmonary barotrauma in the inverted position laboring would be higher. Another consideration is that the known physiologic effect of the gravid uterus in decreasing the residual volume and functional residual capacity could exacerbate the increased intra-alveolar to intra-pleural pressure differential [13], thus increasing the risk of alveolar rupture and subsequent pneumomediastinum.
There is currently insufficient information about pulmonary physiology and pressure dynamics in the second stage of labor. We propose that the intrathoracic pressure dynamics associated with inverted patient position could have contributed to the case patient’s rare complication of SPM. However, further study is indicated into this area to test this theory. In an age with increasingly complicated and high-risk pregnancies, we as obstetricians are obliged to provide the most evidence-based counseling not only on pregnancy but labor as well.
LM: Conceptualization, manuscript writing, editing; CW: Manuscript editing; ZG: Conceptualization, manuscript editing; PF: Conceptualization; JM: Conceptualization, manuscript editing, supervision.
The authors declare no conflicts of interest.