Background: Charcot neuroarthropathy (CN) is a destructive condition, commonly affecting the foot, and manifests secondary to diabetes mellitus. We compare basic demographics and investigate trends among patients with CN treated at a large, quaternary academic medical center according to surgical procedure, attendance at physical therapy (PT), and all-cause mortality.
Methods: Following IRB approval, a database was created using CPT and ICD-10 codes to encapsulate patients with CN of the lower extremity who underwent amputation, exostectomy, and/or arthrodesis at a single institution over a 22-year period. Demographics, number of PT appointments, and all-cause mortality were recorded. Descriptive statistics, chi-square tests of independence and logistic regression were conducted.
Results: A total of 1671 patients were identified - 248 of whom had documented PT appointments with 735 (44%) female patients, 1,499 (90%) identified as white, 131 (7%) had Medicaid insurance, and patients attending PT resided in 20 different counties. The relationships between PT attendance versus county of residence (p = 0.035), insurance status versus mortality (p = 0.039), and type of procedure versus PT (p = 0.032), demonstrated statistically significant differences. Lastly, a logistic regression model predicted that as the number of PT appointments increased, mortality decreased with 84% accuracy.
Conclusion: CN is a progressive, degenerative disease that impairs quality of life. Disease progression harbors a complication profile that may be influenced by socioeconomic factors. Access to a hospital equipped with PT infrastructure is essential and affects outcomes associated with CN through facilitation of gait restoration, foot off-loading education, and wound care - which can lead to an increase in survivorship.
Social determinants of health, Charcot foot, Diabetes, Physical therapy, Insurance
CN: Charcot Neuroarthropathy; PT: Physical Therapy; CI: Confidence Interval
Charcot neuroarthropathy (CN) is a pathologic, destructive condition that occurs secondary to diabetes mellitus, and commonly affects the bones and joints of the foot [1,2]. Although the pathogenesis of CN is poorly understood, it is thought to involve peripheral neuropathy that progresses and worsens with repeated microtrauma [3]. The chronic hyperglycemia experienced by patients with longstanding uncontrolled type 2 diabetes mellitus leads to nonenzymatic glycation - damaging axonal proteins, which manifests as the microvascular complications of peripheral neuropathy [4].
Previous literature suggests that geographical barriers and healthcare providers’ awareness of these barriers are pertinent challenges to the delivery of evidence-based assessment, diagnosis, and management of patients who present with CN [5,6]. Additionally, decreased proximity to appropriate healthcare facilities further increases the risk of complications in culturally disadvantaged communities with lower education and income [7-10].
Nevertheless, the extent of the impact of social determinants of health and its association with outcomes in patients with CN is ill-defined. In order to better understand this association, the primary aim of this study was to compare basic demographics and investigate regional trends among CN patients treated at a quaternary, academic medical center by type of surgical procedures they received, attendance at physical therapy (PT) appointments, and all-cause mortality.
This retrospective chart review utilized electronic health record information from a single academic medical center. In consideration of inclusion criteria, the research network, TriNetX, was utilized to preliminarily identify patients at a single institution from January 1, 2020 to January 31, 2022 with CPT and ICD codes delineating a diagnosis of Charcot joint of the lower extremity who underwent amputation, exostectomy, and/or arthrodesis. This patient database was then further characterized using an institutional electronic medical record to identify demographics, including sex, race, type of insurance, and county of residence. Additionally, if a patient attended PT at the study institution, the number of PT appointments attended was collected. Indication of all-cause mortality was also recorded for each patient. This study was approved by the Penn State College of Medicine Institutional Review Board (IRB).
Demographic data was summarized using descriptive statistics. Chi-square tests of independence with a confidence interval of 95% were used to determine the relationship among sex, race, all-cause mortality, type of procedure, type of insurance, county, and attendance at PT sessions. A p-value of less than 0.05 was considered statistically significant. PT appointment attendance and all-cause mortality were further analysed using a logistic regression model.
A total of 1671 patients were met inclusion criteria for this study. Two-hundred and forty-eight of these patients had documented PT appointments. Table 1 depicts the basic demographics of patients included in the study. Seven-hundred thirty-five (44%) patients were female and 1,499 (90%) of patients identified as white, with the remaining 10% of people identifying as Black or African American, two or more races, or other. One hundred and thirty-one (7%) patients indicated that they had Medicaid health insurance. Six-hundred ninety-five (42%) patients underwent an amputation, 534 (32%) underwent exostectomy, and 442 (26%) patients had an arthrodesis for surgical management of their CN. Furthermore, patients who attended PT resided in 20 different counties within the state of Pennsylvania, as illustrated in Table 2. Figure 1 demonstrates a geographic heat map of the distribution of patients in each county in relation to the location of the study institution.
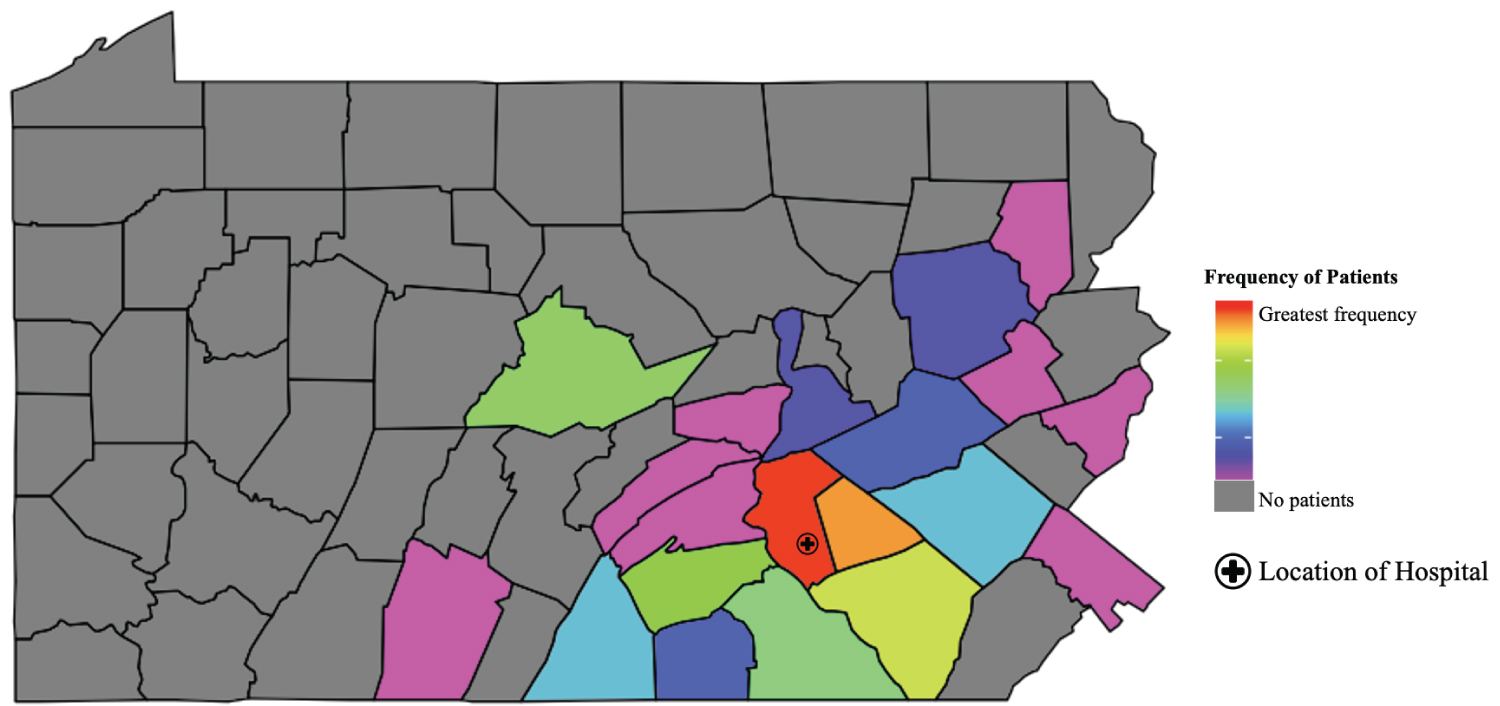 Figure 1: Geographic heat map identifying number patients in each county who attended Physical Therapy Appointments at treating medical center.
View Figure 1
Figure 1: Geographic heat map identifying number patients in each county who attended Physical Therapy Appointments at treating medical center.
View Figure 1
Table 1: Basic demographics of patients with Charcot Neuropathy who did or did not attend physical therapy (PT) appointments. View Table 1
Table 2: Patients with CN who attended and did not attend physical therapy according to Pennsylvania county of residence. View Table 2
A statistically significant relationship was observed between attending PT versus county (95% CI: p = 0.035), insurance status versus mortality (95% CI: p = 0.039), and type of procedure versus PT (95% CI: p = 0.032). When comparing the county where a patient resided with mortality (95% CI: p = 0.966), in addition to type of procedure (95% CI: p = 0.613), and insurance status (95% CI: p = 0.0909), there was no significant difference appreciated, indicating that these variables were independent of each other.
Lastly, a logistic regression model was utilized to predict mortality based on attendance to PT. With 84% accuracy, the logistic regression model predicted, that as the number of PT appointments increases, mortality decreases as shown in Figure 2.
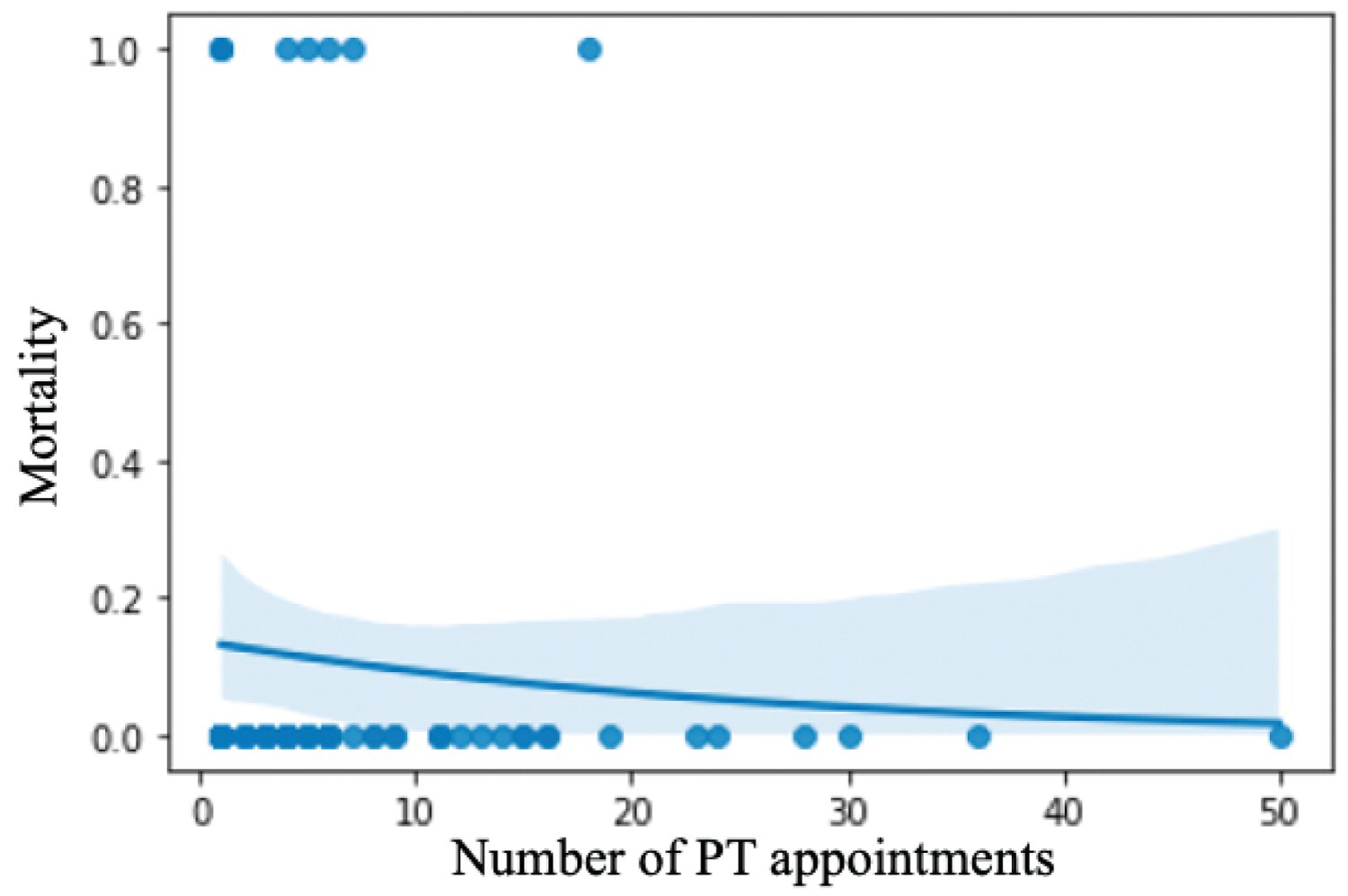 Figure 2: Logistic regression model of Physical Therapy Appointments versus All-Cause Mortality.
View Figure 2
Figure 2: Logistic regression model of Physical Therapy Appointments versus All-Cause Mortality.
View Figure 2
In this study of socioeconomic factors that impact CN patients at a single institution, attending PT was significantly associated with the county in which a patient lived and all-cause mortality. Secondarily, insurance status was significantly associated with all-cause mortality rates. These findings support previously published data characterizing socioeconomic health disparities in CN management [5].
Type 2 diabetes mellitus is a growing global health concern, affecting approximately 462 million people worldwide, with a substantial impact on morbidity, mortality, and hospital expenditures [8]. This chronic disease disproportionately affects racial and ethnic minorities and low-income populations. One of the many complications that is associated with this disease pathology is CN, a serious and life-threatening condition that is often misdiagnosed [11]. The progressive and degenerative nature of CN strongly impairs quality of life, with disease progression and complications being highly influenced by socioeconomic factors. Particularly, Canedo, et al. demonstrated that lack of insurance coverage and education underpinned some of the racial/ethnic disparities observed in diabetes quality of care in regard to hemoglobin A1C testing for Hispanics, Blacks, and Asians - as well as diabetic foot exams for Hispanics with type 2 diabetes mellitus [12]. Additionally, Mahoney, et al. determined that private health insurance coverage was associated with 0.82 (CI: 0.67, 0.99) decreased odds of undiagnosed diabetes mellitus [13]. Our findings are consistent with the current literature on the impact of social determinants of health on disparities in type 2 diabetes mellitus in addition to the impact of effective delivery of evidence-based management for the assessment, diagnosis, and management of patients with CN [5,12-14].
Many studies have reported that CN has a major negative impact on the quality of life of a patient [15-17]. In addition, financial burden is increased because patients with CN require life-long support as they are at increased risk for ulceration, infection, and amputation [17]. Given that there is no gold standard treatment for CN, patients may require more than one procedure in the management of CN in conjunction with medical management for progressive diabetes mellitus. As such, caring for the Charcot patient requires a multidisciplinary approach - which should involve primary care providers, endocrinologists, wound care teams, social work, physical therapists, and surgeons.
There are limitations inherent to this study. Namely, our data encompasses data collected at a single academic institution. Thus, the true extent of the interaction among the variables being studied may not be fully characterized. Selection bias may exist - particularly with respect to inclusion of patients who were able to attend PT appointments during this time period. Additionally, this study does not account for patients that opted to pursue PT at an outside facility. Despite these limitations, the results are relevant and support the growing body of literature on disparities in Charcot management.
Patients with CN are medically complex and an easily accessible hospital equipped with PT infrastructure. Our findings demonstrate that patients with CN who are engaged in their care - through participation in PT appointments, which facilitate gait restoration, foot off-loading education, and wound care - have higher survivorship, on average. The aforementioned findings provide insight underlying areas for health prevention as primary care providers may often treat a patient with Charcot foot. Providers should consider patients presenting with diabetic neuropathy and lower extremity swelling, pain, edema, redness, or deformity for further medical workup because of the possibility of a diagnosis of Charcot neuroarthropathy. Furthermore, additional outreach is required for patients who do not have quality health insurance because insurance status is significantly associated with all-cause mortality.
All authors have made substantive contributions to this manuscript and have no conflicts of interest to disclose.