A malignant melanoma is an abnormal proliferation of pigmented cells in the body. Half of these tumors have BRAF mutations, with a worse response to treatment. We present the case of a 58-year-old male with a pigmented nodular lesion on the right calf and inguinal lymphadenopathy; a positive biopsy for nodular malignant melanoma (MMN) with the largest diameter of 2 mm, Clark level III and Breslow of 3 mm. Four months after tumor resection of the right pelvic limb and right lymphadenectomy are performed, the patient presents multiple and confluent lesions in the same region. He received treatment with ipilimumab every 6 weeks and nivolumab every 3 weeks, with stability and without progression of the lesions. The patient has one year of survival from the time of diagnosis as well as 10 months of survival from the start of immunotherapy, currently with a year of survival. The combined immunotherapy of ipimumab plus nivolumab has been shown to be one of the most effective regiments for MMN.
Nodular malignant melanoma, Immunotherapy, Ipilimumab, Nivolumab
Programmed Cell Death Protein 1 (PD-1), Cytotoxic T-Lymphocyte-Associated protein 4 (CTLA-4)
Malignant melanoma is an abnormal proliferation of the pigmented cells of the body [1], originating 95% in the skin and 5% in the mucous membranes [2]. It has a high mortality rate of approximately 65,000 deaths per year [1], a global incidence of up to 3% [3-5], and an annual incidence of approximately 200,000 new cases [1,6]. It represents 1.7% of all cancers worldwide, with an increase of 320% since 1975 [6]. In Mexico, about 4,000 people died from melanoma in a period of 5 years, with the disease being more common in urban areas and predominantly affecting the female sex [7]. Quintana Roo has one of the lowest mortality rates in Mexico, with 3 deaths in 2016 [8].
In 1960, the dermatologist Wallace Clark classified melanoma as it is currently known: superficial, lentigo maligna, nodular, acral lentiginous, among others. At the same time, he classified melanoma according to the degree of skin invasion, currently known as "Clark levels" [9]. Among risk factors, the most important one is exposure to ultraviolet rays [10,11], which is related to more than 70% of all melanoma cases, particularly UVA and UVB rays, since UVC is blocked by the layer of ozone in the atmosphere [6]. Other risk factors include race, age, genetics, the presence of nevi, and smoking, with Caucasians being the most affected and a mean age of presentation of 57 years [12-15].
For early diagnosis, the ABCD criteria (asymmetry, borders, color, and diameter) are used, a test with a sensitivity greater than 90% but with low specificity [13,16]. Any suspicious lesion should have an excisional biopsy for further evaluation and staging [13,16]. About half of melanomas have BRAF mutations, 90% of which occur at codon 600. Moreover, these mutations have a worse prognosis with conventional treatments because they cause extracellular regulatory kinase activation, leading to large cell proliferation [16-18].
Herein lies the importance of new treatments that improve survival in patients with melanoma, particularly in advanced stages. Immunotherapy management has increased overall survival in advanced-stage patients [19], as 5-year survival is approximately 10% [1] and a median overall survival of approximately 8 months [20]. Mortality in the United States has decreased from 30% to 10% in the last decade since the inclusion of immunotherapy in 2011 [21].
PPD-1 and CTLA-4 inhibitors are classical checkpoint inhibitors with an antineoplastic effect through activation of cytotoxic T cells [1,17,22,23]. Ipilimumab is a monoclonal antibody that enhances the cellular response of T cells by blocking the CTLA-4 pathway. On the other hand, nivolumab is a monoclonal antibody that enhances T-cell activation and proliferation by disrupting the interaction of the PD-1 receptor with its ligands [1,17,22,23].
We report herein a case of multiple atypical malignant nodular melanomas and the outcome of the patient's survival with immunotherapy.
A literature review was performed using scientific databases. The objectives established to perform the search and interpretation of the evidence were the identification of meta-analyses and systematic reviews highlighting the diagnosis and treatment of nodular melanoma. Furthermore, to recognize relevant information for the analysis of cases of malignant melanoma.
The search strategy focused on key concepts of interest: skin melanoma treatment. The search term used included the recognized medical subject heading (MESH): ("skin melanoma treatment" [Mesh]). The following databases were searched: PubMed, Journal of the American Medical Association (JAMA), New England Journal of Medicine (NEJM), LILACS, Scielo, and arXiv. The maximum publication date of the articles was set at a range of 5 years to present (2017-2022).
Inclusion criteria were full-text scientific articles, meta-analysis, and systematic reviews on the treatment of skin melanoma, published in Spanish and English. The exclusion criteria were articles with a publication date prior to 2017, if they talked about other skin tumors, if they did not talk about treatment, or if this was surgical.
Search results: From the search in the different databases, 33,396 articles were found, resulting in a total of 9,268 articles from the 5-year exclusion. We obtained 249 meta-analyses and systematic reviews, after which we obtained 29 articles by reading titles and abstracts. Eighteen articles were obtained from the complete reading of these, including those that talked about the diagnosis or treatment of nodular melanoma (Figure 1).
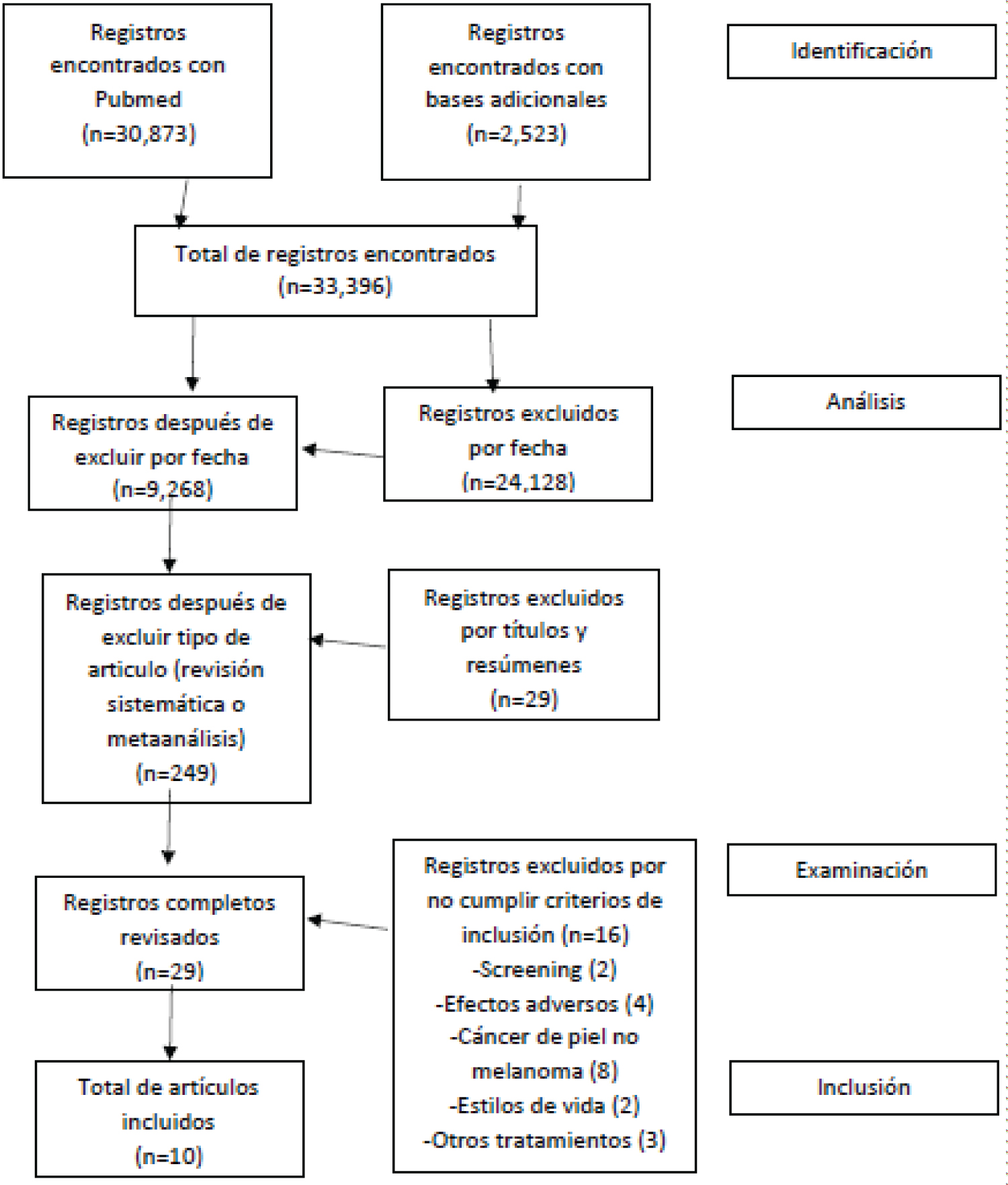 Figure 1: Search diagram.
View Figure 1
Figure 1: Search diagram.
View Figure 1
A 58-year-old male presents to the oncology consultation without a prior family history of neoplastic diseases, with a 15-year history of type 2 diabetes and hypertension under management with insulin and metformin, and losartan, respectively. The current condition began in August 2021 with the appearance of a pigmented nodular lesion (Figure 2a) on the right calf, inner side, 1.5 cm in diameter, painless, without ulceration or bleeding, and without lymph node growth. Subsequently, he presented with accelerated growth as well as inguinal adenopathy, 2 × 3 cm in diameter, for which a biopsy of the lesion was performed. A histopathological study was performed and reported a positive border for a neoplastic lesion. Nodular malignant melanoma was diagnosed with a 2 mm diameter, Clark level III (papillary dermis), and Breslow 3 mm. A low mitotic count was also reported.
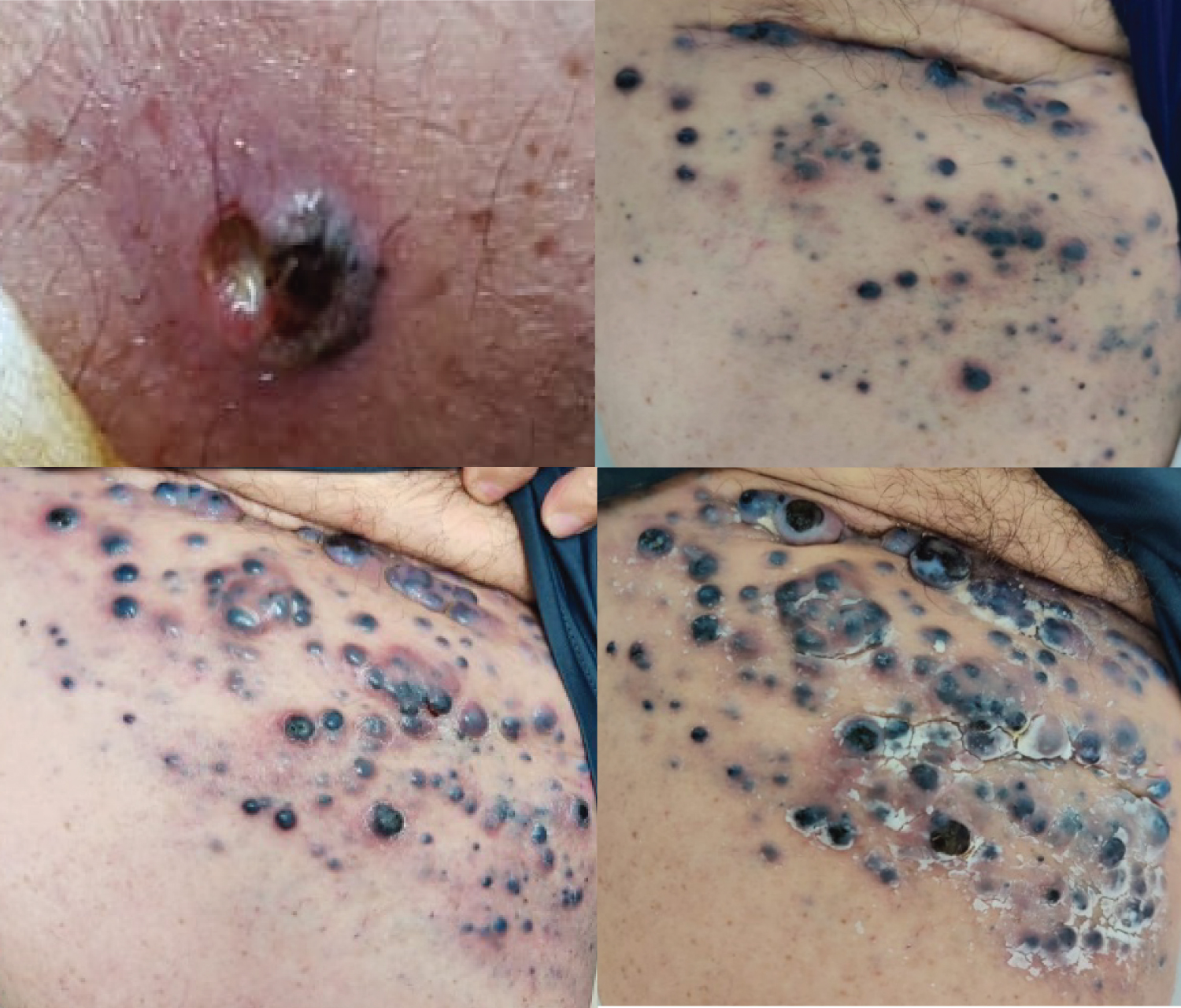 Figure 2: Evolution of injuries (a) August 2021; (b) May 5; (c) May 20, 2022; (d) July 2022.
View Figure 2
Figure 2: Evolution of injuries (a) August 2021; (b) May 5; (c) May 20, 2022; (d) July 2022.
View Figure 2
A tumor resection of the right pelvic limb and right lymphadenectomy for melanoma was performed on October 25, 2022, with the following report: Nodular melanoma 1.8 × 1.7 cm, 5 mm thickness, invading reticular dermis, vertical growth, satellite nodules not identified, macroscopic pigmentation present, ulceration present, mitotic index: 1 mitosis per mm3, lymphatic invasion present, perineural invasion not identified, tumor regression not identified, lymph nodes with metastasis: 1, surgical edges without evidence of neoplastic cells. A bone gamma gram was performed on September 23, 2021, with a negative result for osteoblastic activity.
In February 2022, a new lesion appeared in the right inguinal region (Figure 2b), melanoma in transit of approximately 0.0 × 0.8 cm, in addition to a nodule in the internal region of the right muscle 5 cm from the groin, with nodular characteristics. Subsequently, new multiple and confluent lesions appeared in the same region, some of them already healed. In April, treatment with nivolumab 1 mg/kg was started. Due to the rapid progression of the lesions as well as pelvic limb edema, in May, ipilimumab 3 mg/kg was added, as well as BRAF determination. The schedule used was ipilimumab every 6 weeks and nivolumab every 3 weeks. Subsequently, the disease remained stable, with no progression of lesions. The patient is currently under follow-up by oncology (Figure 2c and Figure 2d).
Currently, the patient has one year of survival from the time of diagnosis as well as six months of survival from the start of immunotherapy. Since rapid progression was seen, an upscaled therapeutic approach with nivolumab-based immunotherapy was started. Studies have shown that nivolumab-based immunotherapy has the highest overall survival rate in patients with advanced melanoma [3,8,24,25].
In a meta-analysis [3] with 11 reports from 8 randomized controlled trials, it was stated that Nivolumab is effective in advanced melanoma, regardless of PD-L1 status, BRAF mutations or drug type, with an improvement in overall survival. In this case, despite the start of treatment with nivolumab, the patient had a rapid progression of the disease in one month, and therefore immunotherapy with ipilimumab was added. According to Zoe, et al. [20], the combined therapy of ipimumab plus nivolumab is more effective than ipilumumab monotherapy. In another review by Zhang, et al., where 12 studies were included, they made the same assertion, with an overall survival greater than 5 years with combined therapy versus monotherapy [1].
In regard to melanoma with some degree of metastasis, Menshawy, et al. [16] in a study that included 31 studies with a total of 1910 patients, found that combined immunotherapy with ipilimumab and nivolumab had a greater impact on overall survival in comparison with monotherapy in these patients. In a systematic review and meta-analysis with 10 reports in a total of 790 patients, the clinical efficacy of the combination of ipilimumab and nivolumab versus ipilimumab alone was evaluated in patients with melanoma in advanced stages, having a greater impact on overall survival and response than the aforementioned combination [18].
Another important aspect of immunotherapy is to recognize the BRAF mutation in melanoma, since treatment variations are made depending on the mutations found. According to the ASCO guidelines, patients with BRAF-negative melanoma should receive immunotherapy with nivolumab, pembrolizumab, or the combination of dabrafenib and trametinib [4]. In an unresectable setting, as in our patient, treatment should be with ipilimumab plus nivolumab, nivolumab alone or pembrolizumab. In addition to the therapies mentioned, BRAF-positive patients should be given dual therapy with a BRAF/MEK inhibitor and encorafenib/binimetinib or vemurafenib/cobimetinib [4,5,23].
Another option studied is therapy with pembrolizumab, a PD-1 inhibitor approved as immunotherapy for advanced melanoma, with differences in overall survival with its use [3,16].
In patients with BRAF V600E or V600K positive mutations, the combination of dabrafenib and trametinib has been used, with improved free survival and metastasis-free survival [14,26]. The most effective treatment, in terms of overall survival in BRAF-positive melanoma, is the combination of BRAF inhibitors plus MEK inhibitors (trametinib), and PD-1 inhibitors being the safest [5,25].
Another treatment used in advanced melanoma is interferon, with variable results. In a meta-analysis with 7744 patients, adjuvant IFN-α was found to significantly reduce the risk of relapse and improve overall survival by up to 3% [27]. Similarly, chemotherapy is used to treat melanoma, particularly in countries without access to immunotherapy, with an overall survival of up to 11 months [24]. However, the efficacy of chemotherapy is lower than that of immunotherapy [25]. Among the prognostic factors is the stage of the disease, lactate dehydrogenase (LDH) levels, and ECOG, with a better prognosis for those with targeted therapy or immunotherapy [28].
The use of immunotherapy in patients with malignant melanoma is a novel treatment. The importance of this treatment lies in an increased overall survival rate of up to 70 to 80%, either in monotherapy or combined therapy. Current evidence points to the initiation of immunotherapy in patients with malignant melanoma. The combination of nivolumab and ipilimumab is the dual therapy with the best evidence that it has the greatest impact on overall survival, according to the systematic review performed. More specifically, in BRAF 600-positive patients, it is the combination of BRAF inhibitors plus MEK inhibitors (trametinib). The recognition of malignant melanoma in early stages is important as it implies timely treatment, particularly with immunotherapy. Likewise, early recognition and management allows us to avoid the progression of the disease to metastasis.
The authors declare that they have no conflict of interest in this review.
The authors received no funding for this case report.