Background: Differentiated Thyroid Carcinomas (DTC) constitutes a significant percentage of pediatric malignancies, presenting distinct histological and morphological differences from their adult counterparts. Pediatric DTCs exhibit greater aggressiveness, and are diagnosed at a more advanced stage than adult thyroid cancers, in many cases already having spread to the lymphatic system. This comprehensive review explores the risk factors for lymph node metastases (LNM) in pediatric DTC.
Methods: This review of relevant literature from MEDLINE and Scopus databases was conducted focusing on articles published between 2000 and 2023. The inclusion criteria targeted studies exploring risk factors for LNM in pediatric DTC. Nine studies, encompassing a pooled sample of 3.525 patients, were selected for comprehensive analysis.
Results: Extrathyroidal extension (ETE), tumor size, and multifocality emerged as the most consistently identified risk factors for LNM in pediatric DTC. The analysis of diverse studies revealed variations in the association of LNM with other factors, such as age, sex, and histological type, highlighting the need for further research.
Conclusion: This review underscores the importance of identifying risk factors, particularly ETE, tumor size, and multifocality, to enhance predictive models and guide preoperative strategies. The conflicting nature of guidelines emphasizes the critical need for evidence- based and universally accepted prognostic criteria for pediatric DTC.
Pediatric thyroid cancer, Metastases, Lymph nodes, Risk factors, Childhood thyroid cancer, Differentiated thyroid cancer, Lymph node metastases
DTC: Differentiated Thyroid Carcinoma; LNM: Lymph Node Metastases; ETE: Extrathyroidal Extension; SMNs: Subsequent Malignant Neoplasms; PTC: Papillary Thyroid Carcinomas; FTC: Follicular Thyroid Carcinomas; DSV: Diffuse Sclerosing Variant
Thyroid malignancies constitute the most frequent type of cancer of the endocrine system, 90% of which fall into the category of Differentiated Thyroid Carcinomas (DTC). DTCs comprise the vast majority of thyroid cancers, with roughly 1.8% of these cases occurring in children, according to the Surveillance, Epidemiology and End Results (SEER) program (ΝΙΗ-National Institute of Cancer) [1]. Childhood DTCs are some of the most frequent Subsequent Malignant Neoplasms (SMNs), since they can appear as secondary malignancies in pediatric patients, even years after their initial cancer treatment [2-5].
Pediatric DTCs differ both morphologically and histologically from DTCs of adult patients, exhibiting differences in pathophysiology, clinical presentation, and long-term outcomes [6-8]. They differ so significantly from adult DTCs, to the extent that they are considered as almost entirely different pathological entities. Specifically, pediatric DTCs are rarer, more aggressive and more advanced at the time of diagnosis compared to their adult counterparts [9,10], exhibiting higher rates of metastasis (25%) and lymph node infiltration (40-80%) [11-13]. It is also essential to emphasize that therapeutic management administered to adults may not always be suitable for children. While, children are highly unlikely to succumb to thyroid cancer, they are vulnerable to aggressive treatment methods, such as administration of I-131, and they are at a higher risk of developing long-term side effects due to their longer life expectancy [14]. As a result, although childhood DTCs are easily treated and have a positive prognosis, they are characterized by a significantly higher recurrence rate compared to adults, primarily due to lymph node infiltration. This necessitates lifelong surveillance [14].
Previous guidelines were tailored for adult patients with thyroid carcinomas. However, the remarkable differences between pediatric and adult DTCs have highlighted the necessity for the development of new guidelines and principles specifically aimed at childhood thyroid tumors [6]. Recognizing this need, the American Thyroid Association formulated guidelines for the management of pediatric thyroid nodules in 2016, followed by the newly developed European guidelines in 2022 [6,14].
Unfortunately, these guidelines are not entirely compatible, and the recent literature regarding the screening, diagnosis, surgical management and reevaluation of children with DTC emphasizes the lack of sufficient data and long-term studies on this topic, thus producing conflicting results. There is great controversy surrounding the risk factors, ultrasonic identification, diagnosis and management of Lymph Node Metastasis (LNM) and the use of Prophylactic Lymph Node Dissection in the surgical treatment of DTC. The insufficiency of scientific evidence and long-term studies on this issue has led to conflicting opinions on this extremely important matter.
Considering all these factors, and acknowledging that differentiated pediatric thyroid cancer is on the rise [1,15,16], we aimed to address the pressing need for further exploration and determination of the risk factors responsible for lymph node metastases in pediatric DTC cases.
There are four primary types of thyroid carcinomas that occur in children. The first two types (papillary and follicular) are well differentiated, while the other two (medullary and anaplastic) are poorly differentiated or undifferentiated. Papillary thyroid carcinoma represents the most frequent childhood thyroid cancer, primarily affecting teenagers. It is typically multifocal, involving multiple nodules on both thyroid lobes, extends to cervical lymph nodes and metastasizes to the lungs [6]. Nevertheless, the prognosis remains favorable for most cases. Follicular thyroid carcinoma usually presents as a solitary nodule. It tends to metastasize to the lungs and bones, but almost never to the neck region, since it rarely infiltrates the lymphatics. Still, this type of cancer carries a notably favorable prognosis.
Medullary thyroid carcinoma, originating from the parafollicular C cells of the thyroid gland, is most commonly associated with hereditary mutations of the RET gene as well as Multiple Endocrine Neoplasia Type 2 (MEN2) syndrome. It primarily affects children as young as 4-years-old, and is typically diagnosed in advanced stages, already having spread to other parts of the body. Anaplastic thyroid cancer is an exceptionally rare occurrence in the pediatric population [17].
Thyroid carcinoma comprises 20-25% of thyroid nodules in children, but only 5-10% of thyroid nodules in adults [6]. The majority of pediatric thyroid cancer cases (85%) are of the papillary type (PTC) while follicular thyroid carcinomas (FTC) make up only 8% [18-21].
The rate at which pediatric thyroid carcinomas infiltrate the lymphatic system is extraordinarily high [22]. Pediatric PTC typically presents with cervical lymph node metastases and is predominantly multifocal and bilateral [23-25]. In contrast, pediatric FTC usually appears to be unifocal and unilateral, and most often metastasizes to the lungs, following a hematogenous path [23,26]. Disease recurrence is much more common in pediatric patients than in adults, especially in cases of PTC, where recurrence rates range from 13% to 37% [24,25,27,28]. Evidently, the presence of LN metastases plays a major role in recurrence [29,30].
We conducted a search of two databases (MEDLINE and Scopus) using as terms (Differentiated Thyroid Cancer) and (Pediatric or Children) and (risk factors) or (differentiated thyroid cancer) and (pediatric or children) and (lymph node metastasis). The retrieved articles’ citations were also reviewed for any further eligible articles. We included original articles published 1) In the English language, 2) Between January 1, 2000, and September 20, 2023, 3) Related to children (age < 18 years), 4) Focused on the identification of risk factors for lymph node metastases, and 5) With sufficient methodologic quality (data and statistical analysis). There was no restriction on study design, number of patients, or sample characteristics. Data extraction was performed using a predefined data form created in Excel. We recorded author, year of publication, country, number of participants, mean age and gender of participants, study design, and parameters that were examined as potential risk factors and main results, specifically multifocality, tumor size, age, sex, race, histological type, vascular invasion, and Diffuse Sclerosing Variant. Due to the high heterogeneity among studies, no statistical analysis was performed. Thus, the data were only descriptively studied.
Overall, 236 records were retrieved. Duplicates and irrelevant studies were excluded; hence, a total of 87 articles were selected. After screening the full text of the articles, 9 studies were eligible for inclusion (Figure 1). The nine publications (with a pooled sample of 3.525 patients) fulfilled our inclusion criteria are shown in Table 1. Among the included studies, 5 were conducted in Asia, 3 in the USA, and 1 in Europe. Of all parameters examined as potential risk factors for LNM, ETE was examined in seven (1,2,3,4,5,6,7), tumor size in six (1,3,6,7,8,9), multifocality in seven (1,2,3,6,7,8,9), young age in two (3,7), sex in two (6,7), race in one (6), histological type of the DTC in one (6), vascular invasion in one (2), and diffuse sclerosing variant of the PTC in one (2).
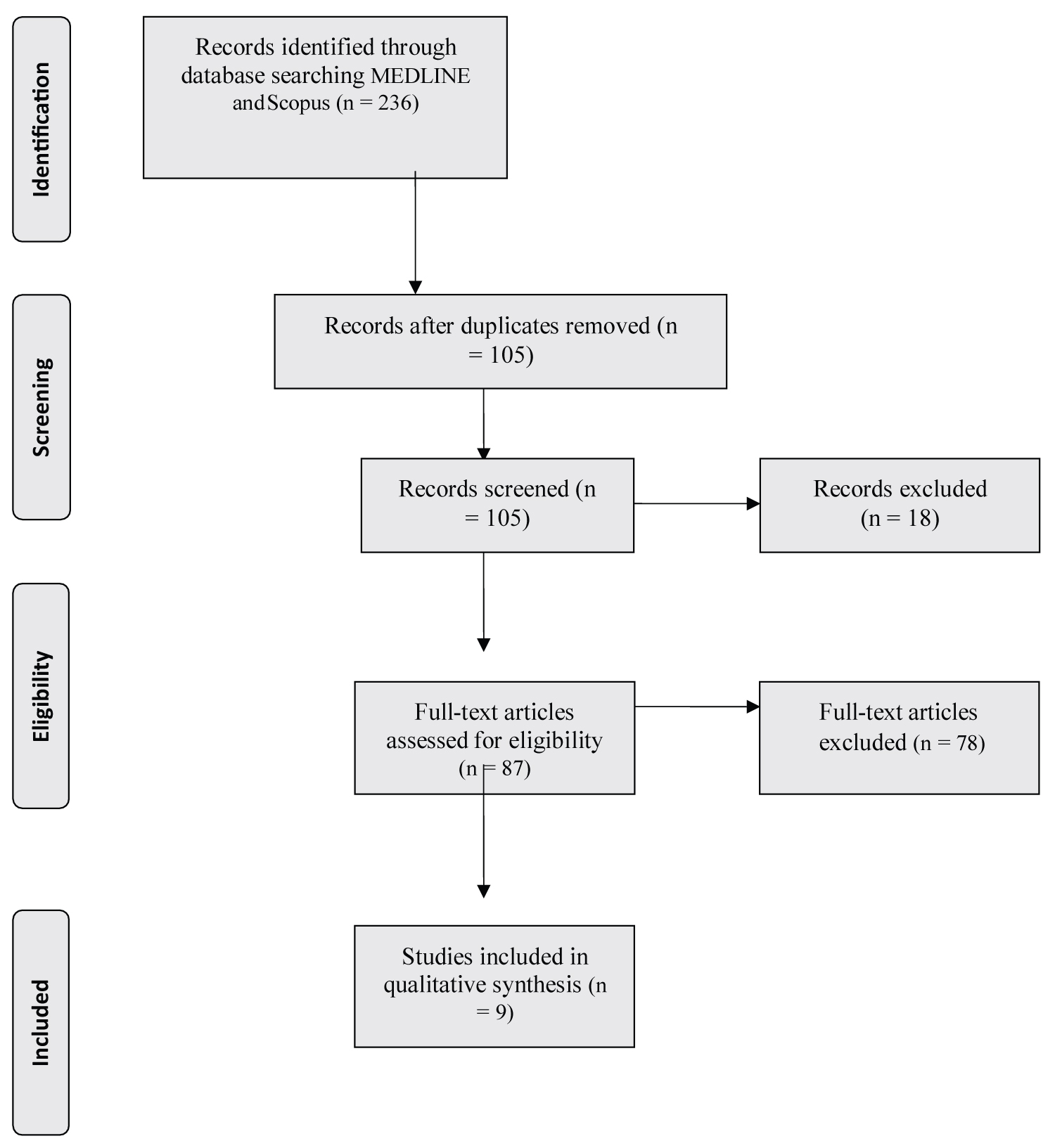 Figure 1: Study flow diagram (Prisma Flow Chart).
View Figure 1
Figure 1: Study flow diagram (Prisma Flow Chart).
View Figure 1
Table 1: Characteristics of the 9 included studies. View Table 1
After carefully examining these articles, it was made clear that ETE, Tumor size, as well as multifocality, were the three most agreed-upon significant risk factors correlated to a higher risk for LNM. These three parameters were proven to be statistically significant predictors for LNM after thorough statistical analyses conducted by six or more studies each. Less frequently associated with LNM are age, sex, race, histological type of the DTC, vascular invasion, and diffuse sclerosing variant of the PTC, which are parameters that were found statistically significant as risk factors by two studies or less.
Reviewing the risk factors responsible for lymph node metastases on pediatric DTC aims to provide a comprehensive understanding of the associated parameters, leading to the emergence of better informed and more precisely guided treatment decisions. The consistent conclusions drawn by scientists across multiple studies correlate certain factors to the likelihood of lymphatic metastases and identify some of them as strong predictors. Kim J, et al. in 2016 extracted their data from the SEER Program database to study the factors responsible for LNM in a large cohort of children with DTC. They concluded that tumor size, extrathyroidal extension, and multifocal disease are statistically significant risk factors correlated to nodal metastases in pediatric DTC. The authors suggested that patients with tumors exhibiting these characteristics should undergo thorough preoperative examination for LNM in the lateral and central cervical compartments, and almost certainly undergo central lymphadenectomy [31]. To identify predictors for lymph node metastatic disease, Spinelli, et al. studied 132 pediatric patients who underwent total thyroidectomy, 87 of whom also underwent simultaneous lymph node dissection. The results showed that multifocality, infiltration of the thyroid capsule, vascular invasion, sizeable extrathyroidal extension, DSV, distant metastases, and the presence of LNM in the lateral compartment, were all significantly associated with LNM in the central compartment [32]. In 2020 Ngo DQ, et al. conducted a retrospective study that included 32 pediatric cases of DTC aiming to shed some light on this highly debatable topic. They thoroughly examined the characteristics of these cases and ultimately confirmed that age (≤ 15 years; p = 0.028), tumor size (> 1 cm, p = 0.008), multifocality (p = 0.028), and extrathyroidal extension (p = 0.041) were strongly associated with a higher risk for lymph node metastases [33]. In a more recent survey conducted by the same scientists, it has been determined that age (p = 0.021), male sex (p = 0.011), tumor size (> 10 mm, p = 0.002), multifocality (p < 0.001), extrathyroidal extension (p = 0.001) and central LNM (p < 0.001) were significantly related to a higher possibility for lateral lymph node metastases [34]. Jain NK, et al. offered a new insight with their study. They retrospectively examined pediatric PTC patients for several associated factors, including tumor size, tumor laterality, tumor focality, ETE, vascular invasion, extra-nodal extension, regional LN metastasis, and/or distant metastasis. They determined that micro-ETE (defined as the presence of one or two microscopic foci measuring < 5 mm each located outside of the thyroid capsule with extension into perithyroidal soft tissue or skeletal muscle tissue), is strongly correlated to LNM in pediatric cases of PTC, and could be a strong risk factor for post-surgical disease [35]. In the multivariate analysis of a cohort of 86 pediatric patients with DTC, performed by Qureshi SS, et al., extrathyroidal extension (ETE) emerged as the single most statistically significant risk factor for LNM [22]. In another study, Min Y, et al. collected data from pediatric DTC patients from the SEER (Surveillance, Epidemiology, and End Results) program database and conducted a thorough analysis, to identify parameters that are associated with lymph node metastases. They determined six definite predictive factors including male sex, race (specifically Asian/Pacific Islander and American Indian/Alaska Native), PTC histological type, multifocality, extrathyroidal invasion (EI) and tumor size (> 5 mm) to be significantly correlated with regional LNM and proposed a model for predicting the possibility for lymphatic metastases in such cases [36]. Liang W, et al. statistically analyzed data from 102 children with PTC, aiming to determine specific parameters for lymph node metastases and to establish a prediction model for such cases. These scientists concluded that multifocality and tumor size proved to be statistically significant individual risk factors for central lymph node metastases [37]. In the same year, Paik C, et al. performed a student’s t-test on a group of 75 pediatric DTC patients and conducted a univariate and multivariate analysis to find any possible risk factors for LNM. They demonstrated that increased tumor volume in pediatric thyroid cancer was associated with lymph node metastases and more advanced-stage disease in general [38].
Pediatric thyroid cancer is currently on the rise [39]. The principal therapy for DTC is surgery. However, in children, DTC typically appears with cervical lymph node metastasis, far more often than in adults [40]. Additionally, pediatric DTCs have a much higher recurrence incidence than adult DTCs, and thus, multiple studies in the literature strongly suggest prophylactic lymph node excision in these cases [6].
Given this data and considering the limited evidence supporting the sensitivity and specificity of imaging techniques in determining the presence of LNM in pediatric DTC, it is of great importance to further investigate the controversy surrounding the use of prophylactic central (CND) and/or lateral neck node dissection (LND) in the surgical treatment of children with thyroid carcinoma.
On one hand, prophylactic lymph node dissection promotes a more accurate disease staging, reduces the risk of cancerous micro-infiltrations remaining in the lymphatic drainage system, and thus minimizes the possibility of recurrence while maximizing cancer-free survival [40,41]. On the other hand, considering the overall good prognosis of DTCs, lymph node dissection surgery carries potential complications and dangers that could greatly impact the patient’s quality of life, such as vocal cord palsy and laryngeal nerve damage or injury [8]. Even the guidelines of esteemed medical organizations are conflicting on the topic of lymph node dissection. European Guidelines suggest that only children with advanced DTC should undergo therapeutic central LND (high suspicion of LNM, ETE, distant metastases), while children with less alarming features can be limited to ipsilateral LND or none [6]. Moreover, the same panel of experts suggests both central and lateral lymphadenectomy in children with pre-operatively proven pre-existing lymphatic metastasis [6].
On the contrary, guidelines from the American Thyroid Association (ATA) suggest Central Node Dissection for children with extrathyroidal extension and/or locoregional metastasis or cytologically confirmed LNM. For patients that don’t fulfill these criteria, it is recommended by the ATA that CND may be selectively considered based on the experience of the surgeon and certain tumor parameters, such as focality and size. The same experts propose ipsilateral CND for unifocal tumors, followed by possible Lateral CND based on intraoperative decisions according to intraoperative findings [14].
The need for clear, evidence-based, and unanimously accepted prognostic criteria and treatment strategies for pediatric DTC is also increasing.
Pediatric DTCs retain an exceptionally high incidence of Lymph node metastasis, which greatly differentiates them from adult types of DTCs. Multiple studies have contributed to the identification of the three most important risk factors for LNM: extrathyroidal extension, multifocality, and tumor size. Less frequently associated with LNM are young age, sex, race, histological type of the DTC, vascular invasion, and diffuse sclerosing variant of the PTC. These findings shed some light on the complexity of this highly controversial and poorly investigated topic, forming a basis for advancing predictive models and informing preoperative strategies for pediatric thyroid cancer cases.
We would like to recognize and acknowledge the efforts and dedication put into this manuscript. We also thank the resources and support systems that have contributed to our research efforts. No funds were used. We declare no conflicts of interest related to this manuscript.