Background: The neonatal mortality rate is still a significant public health problem in Sub-Saharan African countries and an indicator of the quality of prenatal and perinatal care. This study aimed to determine the neonatal intra-hospital neonatal mortality rate and the maternal and neonatal risk factors associated with neonatal mortality in Kyeshero Hospital.
Methods: This research was a cross-sectional analytical study, which took place over a period of 12 months, from January 1 to December 31, 2021, at Kyeshero Hospital in Goma, Eastern Democratic Republic of Congo.
Results: The Intra-hospital neonatal mortality rate was 17.0%. The multivariate analysis showed various risk factors associated with newborns that low birth weight < 2500 gr ORa = 4.11 (2.17-7.77), Presence of cyanosis ORa = 3.88 (1.97-7.65), absence of reactivity ORa = 20.07 (8.07-49.55), and neonatal infection ORa = 4.78 (2.47-9.22) are real predictor factors of neonatal mortality.
Conclusion: This study noted that neonatal mortality was influenced by neonatal factors. Proper care of the newborn should improve neonatal vital prognosis. The study of preventable causes of death and factors that lead to early neonatal death is fundamental to reducing the infant mortality rate in the world.
Neonatal mortality, Risk factor, Goma
The first 28 days of life is an extremely likely time for a newborn to make many physiological adjustments necessary for life outside the womb, making this the most dangerous time of life [1]. Newborns in need of serious medical attention are admitted to the neonatal intensive care unit, which incorporates innovative technology and trained staff to effectively provide specialized care to newborns [2]. Neonatal mortality is an indicator of a country's demographic, biological, and socioeconomic conditions as well as the health system, public health, and population growth rate [3]. Although the neonatal mortality rate has decreased worldwide, it is slower than the under-5 mortality rate and remains unacceptably high at 37 per 1000 live births [4]. Globally, approximately 7,000 babies die every day; Most of these deaths occur within the first week and nearly 2.6 million babies die within the first month of life [5].
Approximately 78% of these neonatal deaths occur in developing countries, particularly in South Asia and sub-Saharan Africa [6], which account for 39% of all neonatal deaths worldwide and are among the top 10 countries with the highest neonatal mortality rate [7]. In Sub-Saharan Africa alone 1.2 million newborns died every year equivalent to 13,000 deaths per day or almost nine deaths every minute, 50% of neonatal deaths occur in just five countries: Nigeria, Democratic, Republic of Congo, Ethiopia, Tanzania, and Uganda [8]. The majority of neonatal deaths in this part of Africa occur at home, in rural communities, among the poor and poorest, less educated, and in war regions [9-11]. Also causes and risk factors of neonatal death vary by country with the availability in relation to the quality of health care [12]. The democratic Republic of Congo ranks second African Africa countries with higher neonatal rate more than 28 per 1000 live births [13].
This situation shows that neonatal mortality remains a public health problem in many countries. To accelerate the achievement of Millennium Development Goals (MDGs) 4 and 5, several countries, including the DRC, have implemented strategies to substantially reduce neonatal mortality. To target actions, an understanding of the causal factors of neonatal mortality is required in the context of the deaths occurring. This study aims to determine the neonatal intra-hospital neonatal mortality rate and the maternal and neonatal risk factors associated with neonatal mortality in Kyeshero Hospital. The hospital is located in Goma, the North Kivu province of the Eastern Democratic Republic of Congo.
We conducted a cross-sectional analytical study, which took place over a period of 12 months, from January 1 to December 31, 2021, at Kyeshero Hospital in Goma, Eastern Democratic Republic of Congo, which is one of the reference health facilities child health care in this region.
All neonates who were admitted to the neonatal intensive care unit and registered as dead and alive during the first 28 days of the last one-year period (2021). The sample size was calculated based on a formula for cross-sectional study [n ≥ Z1-α2 p(1 - p)/d2], in which Z was the confidence interval at 95%, d was the margin of error of 5%, and p was the proportion of neonatal death at 50.0%. Therefore, the minimum sample size for this study was 484 participants. The simple random probability selection method was used as the sampling method. All newborns aged 0 to 28 days, hospitalized and deceased in the neonatology unit of Kyeshero Hospital, during the study period, and having a complete medical file were included. Were excluded, all newborns who died on arrival in the neonatology department, all malformed newborns, and all newborns whose records were deemed unusable.
The source of data for this study was the neonatology registers at Kyeshero Hospital which consisted of new-born information recorded on the characteristics of the newborn: the gestational age at birth, the age of the newborn at admission, the sex, the birth weight, the notion of crying, the APGAR score at the 5 th and the 10 th minute, the notion of resuscitation, the reason for hospitalization, the clinical signs on admission, the diagnosis, the treatment received and mode of feeding, the duration of hospitalization, the mode of discharge, the age and probable cause of death. But also, factors related to the mother: age, parity, origin, number of prenatal consultations, pathological pregnancy history, the notion of multipregnancies, and premature rupture of membranes, maternal fever 48 hours before delivery, antenatal treatment received, place and mode of delivery.
Variables were described as absolute frequencies and percentages. The determinants of the intention to vaccinate the child or adolescent were evaluated by univariate and multivariate analyses. The associations between independent variables and the primary outcomes (neonatal mortality) were tested using a t-test or Chi-square test as appropriate. The results of the multivariate analyzes were presented as odds ratio (OR) with standard error (SE) and 95% confidence interval (95% CI). A step-by-step, bottom-up Wald analysis was performed to define the variables to be included in the final logistic regression model, according to the results of the univariate models and was complemented by analysis of the model’s predictive power using the Receiver Operating Characteristic curve (ROC).
Authorization to carry out the study, and ethical clearance were obtained from the hospital authorities and the hospital ethics committee. The data were kept confidential.
During our study period, among 501 newborns admitted in the neonatology unit; 85 newborns died. The neonatal intra-hospital neonatal mortality rate was 17.0%.
The study of the epidemiological characteristics of the newborns revealed that 92% of the newborns were aged between 0-6 days, the male sex was more represented with 59.1% vs. 40.9 for the female sex and in this about weight, and the 2500 to 4000 g bracket was more represented with 59.9% (Table 1).
Table 1: Descriptions of socio-demographic characteristics of newborns. View Table 1
The maternal age group greater than or equal to 18 years was more represented with 95.5%. The gestational age range from 37-40 SA was more represented with 61.7%, the number of CPN follow-ups less than or equal to 3 was more represented with 68.2% vs. 31.8 for the number greater than 3 The vaginal mode of delivery was the most practiced for these parturients, i.e., 58.3% vs. 41.7% vaginally. These patients were 30.7% parous pauci. For the place of delivery, 99% of these parturients were from Kyeshero hospital (Table 2).
Table 2: Description of the maternal characteristics of newborns. View Table 2
Statistical analyzes of newborn characteristics associated with mortality with a statistically significant association were found in low birth weight newborns (p = ≤ 0.0001) with an Apgar score of less than 7 (p = ≤ 0.0001), with the presence of respiratory distress (p ≤ 0.0001) with the presence of cyanosis (p = ≤ 0.0001), neonatal infection (p = ≤ 0.0001), absence of sucking - swallowing (p = ≤ 0.0001) and absence responsiveness in neonates (p = ≤ 0.0001) (Table 3).
Table 3: Description of the characteristics of newcomers associated with neonatal mortality. View Table 3
It appears from this Table 4 that the non-followed prenatal consultation, the premature rupture of the membranes, and the delivery at home were associated with the risk of neonatal mortality without this association being statistically significant.
Table 4: Maternal characteristics associated with neonatal mortality. View Table 4
Table 5 shows that low birth weight < 2500 gr aOR = 4.11 (2.17-7.77), presence of cyanosis aOR = 3.88 (1.97-7.65), absence of reactivity aOR = 20.07 (8.07-49.55), and neonatal infection aOR = 4.78 (2.47-9.22) were significantly associated with neonatal mortality.
Table 5: Logistic regression. View Table 5
The age of the parent being < 40 years (aOR: 2.40, CI: [1.50-3.83]), fearing that the parent or a member of his/her family will contract COVID-19 (aOR: 2.35, CI: [1.38-4.02]), thinking that the parent and the children are vulnerable to COVID-19 (aOR: 1.70, CI: [1.005-2.2881]), believing that the family or the parent could contract COVID-19 (aOR: 3.07, CI: [1.80-5.23]), and having been vaccinated against COVID-19 (aOR: 16.47, CI: [8.39-32.33]) were significantly associated with the intention to have the children or adolescents vaccinated.
The neonatal mortality prediction model is as follows (Figure 1):
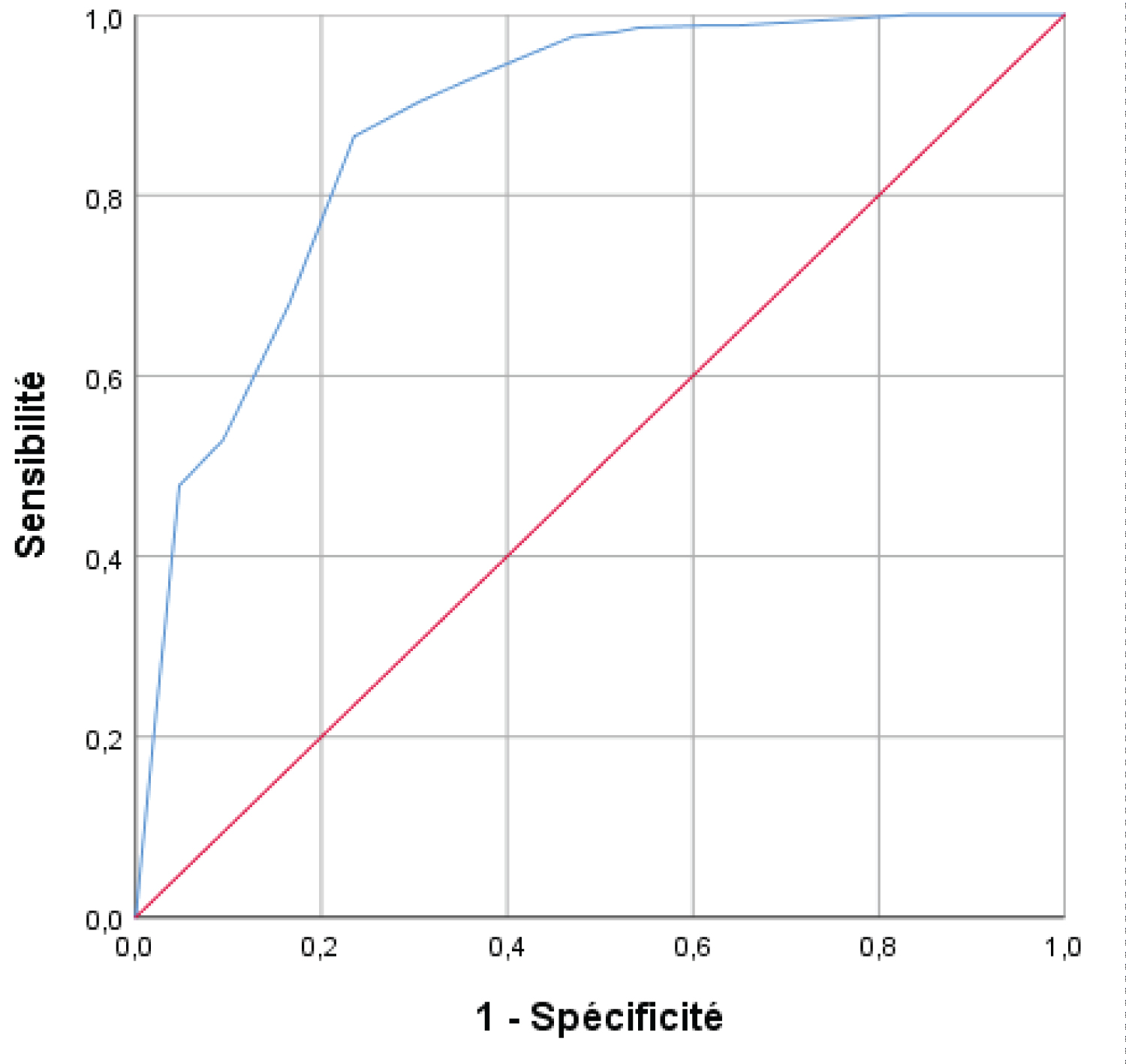 Figure 1: The neonatal mortality prediction model.
View Figure 1
Figure 1: The neonatal mortality prediction model.
View Figure 1
The child mortality rate is considered the best proxy indicator of general population health and the level of socioeconomic development. The child mortality rate is also a useful marker of overall development and a Millennium Development Goal (MDG) indicator [14].
During our study period, the in-hospital neonatal mortality rate was 17.0%. However, this contrasts with the higher rates noted by Mashako K, et al. who conducted a study at the neonatal intensive care unit of the North Kivu Provincial Hospital in Goma, eastern Democratic Republic of Congo (19.7%). The decrease of neonatal mortality rate in Goma may be linked to differences in the quality of health care governance including early intervention which includes the availability, accessibility and affordability of health care systems for children. Quality of care plays an important role in improving neonatal outcomes, and the high levels of neonatal mortality in many resource-limited countries can, in part, be attributed to poor quality of care [15,16]. Effective implementation of quality improvement is possible in low income settings [17], with appropriate strategies including the identification of quality gaps, followed by the development of action plans (and their implementation) to overcome barriers [15].
However, the result was lower than studies in Ghana at 20.2% [18]; Mizan Tepi Teaching Hospital, South West Ethiopia, at 22.8% [19]; Hiwot Fana University Specialty Hospital, Eastern Ethiopia, at 14.3% [20]; and Gondar Referral Hospital in northwestern Ethiopia at 23.1% [21]; University Clinics of Lubumbashi at 36.9% [22] and general referral hospital in Kamina at 25% [23]. Our prevalence of neonatal mortality was higher than in studies conducted in Somali region, Ethiopia, at 5.7% [24]; in Kolwezi, DRC, at 18.8% [25]; and in Mekelle, Ethiopia, at 6.6% [26]. The discrepancy could be due to the presence of socio-cultural and socio-economic differences between Ethiopian regions. This variation could also be due to variation in sample sizes. Another possible justification may be the difference in the use of health services, including delivery in health facilities by skilled care providers and seeking care for sick newborns, variation in health facility configuration (equipment available and trained people) and economic disparities among study participants [27].
This study found that newborns with a birth weight were 4.11 times higher risk of death than those with a normal or higher birth weight (ORa = 4.11; CI 95% [2.17-7.77]). The possible justification is that low birth weight increases children's susceptibility to infection and lowers their immune system and other body defense mechanisms, which control newborns' exposure to disease. As a result, neonatal survival is reduced [28]. Other possible explanations could also be due to low birth weight that newborns are expected to suffer from hypothermia, infection and poor immunological function, which increases the risk of neonatal death [29,30].
In the final logistic regression model of this study, we found neonatal infection was statistically associated with neonatal mortality. Thus, the risks of neonatal mortality were almost five times higher in newborns who had an early neonatal infection than in those who did not (ORa = 4.78; CI 95% [2.47-9.22]). This result is comparable with previous hospital studies conducted in the health zone of Kenge in the DRC [31] and in Eastern Ethiopia [32]. The possible explanation could be justified by newborns that had an infection in the neonatal period who risk dying during the first month of life because their immunity can be significantly affected by the course of the disease.
However, in a multivariate model, the association between cyanosis and neonatal mortality was also noted (ORa = 3.88; CI 95% [1.97-7.65]). For Mona A Simões, et al. the presence of cyanosis, gestational age, cause of death, first- and/or fifth-minute Apgar < 6, and pH value were associated with death in the first week of life [33]. Neonatal cyanosis is always a sign of serious pathological processes and may involve diverse organs and impose a significant diagnostic and therapeutic challenge.
The limitation of this study was it might not indicate a cause-effect relationship because the study design was cross-sectional. Even though this study investigates the most important determinants of neonatal mortality, our study encountered limitations like missing information both on mother and neonates. For instance, economic status and contextual were not assessed.
The intra-hospital frequency of neonatal deaths is 17.0% was justified by four main causes including: Low birth weight, neonatal infection, presence of cyanosis and absent reactivity. Neonatal mortality was influenced by neonatal factors. Proper care of the newborn should improve neonatal vital prognosis. The study of preventable causes of death and factors that lead to early neonatal death is fundamental to reduce the infant mortality rate in the world.
The results of the current study could be used to determine priorities, plan, evaluate services, and improve newborn health care.