Objectives: To determine the prevalence, demographic data, clinical characteristics, microbiologic profile, clinical outcomes and risk factors of mortality among elderly with Community Acquired Pneumonia (CAP).
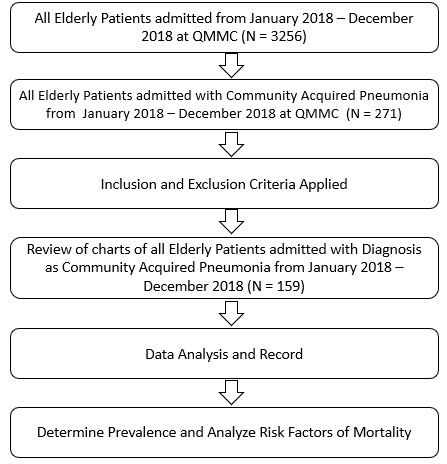
Methods: This study was a retrospective cohort analysis utilizing data from January to December of 2018 among 159 elderly patients admitted with CAP in a tertiary hospital in the Philippines. Demographics, clinical characteristics, microbiologic profile was assessed using percentage and frequency. Chi-square test was used to compare factors to age group and risk factors of mortality were determined using binary logistic regression analysis.
Results: The overall prevalence of elderly patients admitted with CAP was 5% and was noted to be higher in females (55.35%) than males (44.65%). Majority belonged to aged 65-74 years (36.5%). The most common pathogen identified is Escherichia coli (17.24%) and Streptococcus parasanguinis (17.17%) in blood and sputum culture, respectively. Risk factors significantly associated to mortality were history of alcoholic drinking, renal disease, oxygen saturation < 90% upon admission, decrease sensorium, hypotension, lung findings of retractions and decrease breath sounds, Escherichia coli in blood culture and mixed bacterial co-infection in sputum culture (p < 0.05).
Conclusion: CAP is a common problem with clinical impact to elderly patients. The study was able to provide prevalence, demographic data and clinical characteristics associated with mortality among elderly patients admitted due to CAP. This study can also guide clinicians and hospital personnel in infection control and management strategies.
Community acquired pneumonia, Elderly
Community-acquired pneumonia (CAP) is one of the leading causes for hospitalization of the elderly [1,2]. In the Philippines, the age of 60 years is commonly used to define old age and to approximate retirement age [3]. It is expected that by 2025 to 2030, Philippines will be considered an aging society due to an increase of elderly population by at least 10% of the total population [4]. Studies have shown that the risks of pneumonia and pneumonia-related deaths increase with age and are highest in the elderly [1,5,6], indicating that the pneumonia burden is growing in this era of global population aging [7].
Diagnosis of CAP in elderly patients can be very difficult, because the fact that pneumonia in the elderly patients tends to occur more often with extrapulmonary manifestations (delirium, worsening of a chronic conditions or fall to the ground) than with pulmonary findings [2]. Nonspecific symptoms, such as loss of appetite, decline in functioning, mental status changes, worsening of underlying diseases, incontinence and falls may be the presenting signs of infection [8]. The burden of pneumonia is higher among elderly and they are associated with uncommon pathogens than in adult CAP. This category most likely represents multifactorial conditions. Clinical features, drug pharmacokinetics and pharmacodynamics, adverse effects, and outcomes differ in CAP depending on patient age, as age can affect the effectivity of specific antibiotic regimens on clinical outcomes. Current guidelines do not offer specific recommendations for the management of CAP in elderly patients [2,9]. Studies have important implications for effective pneumonia control programs in the aging society. There are limited studies on community acquired pneumonia among geriatric patients in the Philippines. Only pediatric and adult age group had available guidelines for community acquired pneumonia in recent years. There are no specific guidelines for elderly individuals who have higher risk of contracting pneumonia, they usually exhibit atypical symptoms that are not conventional and could lead to mismanagement.
This research serves as a baseline study and aims to provide quantitative information on elderly patients with community acquired pneumonia. Results from this study, might help to modify and expand the current guideline for adult community acquired pneumonia. The study may also be used as evidence for strong implementation and monitoring of public health actions such as Pneumococcal vaccination among elderly and creation of better health programs for elderly patients.
To determine the prevalence, demographics, clinical characteristics and outcomes, microbiologic profile and risks factors for mortality of elderly patients with community acquired pneumonia admitted at Quirino Memorial Medical Center from January 2018-December 2018.
The study used convenient sampling which includes all elderly patients admitted from January-December 2018, and from this population, elderly cases with impression of community acquired pneumonia who satisfies the inclusion and exclusion criteria was selected.
1. Age ≥ 60 years old.
2. Only the first from multiple admissions in the same year for the same patient was included.
3. Elderly patient diagnosed with community acquired pneumonia based on local clinical practice guidelines of pneumonia in immunocompetent adult 2016 [10].
1. Age < 60 years old.
2. Elderly patient admitted for reasons other than CAP and had pneumonia only during hospital stay or health care associated pneumonia.
3. Elderly patient with CAP but who had been initially treated in another institution.
All information on demographic data, clinical characteristics, microbiologic profile, co-morbidities was collected. Frequency and percentage were used to determine the microbiologic profile, clinical characteristics and co-morbidities of elderly patients with community acquired pneumonia. Chi-square test was used to compare these factors to age group. Binary logistic regression was used to determine the association of risks factors to mortality. STATA version 13.0 was used for data analysis. Null hypothesis was rejected at 0.05-alpha level of significance.
In accordance with Philippines Republic Act 10173 known as Data Privacy Act of 2012, all information gathered were used for this research only, the names and hospital number of the patients were not disclosed.
One hundred and fifty-nine elderly patients was diagnose with CAP with a prevalence rate of 5% (159/3256).
Patients were categorized into four age groups: 23.3% (n = 37) of patients aged 60-64 years, 36.5% (n = 58) aged 65-74 years which represents majority of our patients. Followed by 27.0% (n = 43) patients aged 75-84 years and 13.2% (n = 21) patients aged ≥ 85 years. The age range was 60 to 99 years, the average age was 72.7 years, and the median age was 71 years. Demographic and baseline clinical characteristics of study patients were shown in Table 1 according to age.
Table 1: Demographic and clinical characteristics of study patients according to age. View Table 1
There were a higher percentage of female patients at 88 (55.35%) and gender was significant to age group with p-value of 0.037. This distribution showed that percentage of female patients were higher among those 60-64 years old, 75-84 years old, and ≥ 85 years old while male patients were higher among those aged 65-74 years old. Smoking history was shown in 62 (38.99%) while 48 (30.19%) patients had history of alcoholic beverage consumption.
On admission, 136 (86%) of patients had an underlying co-morbidity with diabetes 40 (25.16%) being the most frequently, followed by renal disease 29 (18%) and heart failure 28 (17%). The rest of the demographic profile was not significant with p-value above 0.05. No data on history of vaccination and occupation gathered hence not included in the table.
The most common symptom was cough (69.81%), followed by difficulty of breathing (60.38%). Other symptoms such as chest pain, abdominal pain and vomiting compromise 47.8%. Overall, crackles were observed in 124 patients (77.99%), and decrease in breath sounds in 26 patients (16.35%). Other signs such as bipedal edema, wheezes and irregular heart rate were seen in 68 patients (42.77%). As shown in Table 2, age was significantly associated with body weakness (p = 0.001), difficulty of breathing (p = 0.023), and crackles (p = 0.009). Body weakness and crackles were higher among those 75 years old and above while difficulty of breathing was higher among those 74 years old and below. Vital signs and the rest of the models were not significant to age with p-values above 0.05.
Table 2: Clinical manifestation and CXR findings of study patients according to age. View Table 2
Among 159 patients included in the study, the most frequent chest x-ray findings upon admission were Infiltrates seen in 121 (76.1%), pleural effusion in 17 (10.69%) and consolidation in 11 (6.92%).
Upon admission, 122 (76.73%) patients were identified as having moderate-risk pneumonia and 37 (23.27%) patients as having high-risk pneumonia. A total of 37 patients died, hence the mortality rate of elderly patients admitted with CAP is 23.37%.
Blood culture on 2 different sites and sputum culture were evaluated. As shown in Table 3, the most common organism in blood culture was Escherichia coli (17.24%), and Staphylococcus hominis ss hominis (10.34%).
Table 3: Microbiological Profiles of Elderly Patients with Community-Onset Pneumonia. View Table 3
For Sputum Culture, the most common organism were Streptococcus parasanguinis (17.17%); ESBL negative Klebsiella pneumonia (12.12%), and mixed pathogen infection (8.08%), with Klebsiella and Acinetobacter growth with another bacteria as the most frequent co-infection.
Out of 122 patients who recovered, 114 (93.44%) were discharged without sequalae and 8 (6.56%) were discharged requiring oxygen at home. All patients admitted were given antibiotic treatment during hospitalization.
As shown in Table 4, using binary logistic regression analysis, the association was done among those who survived (without sequalae and with sequalae combined) and those who died. Those categories with "0a" mark were used as basis for comparison. Age and gender were not significant with p-values above 0.05.
Table 4: Factors Associated with Mortality among Elderly Patients with Community-Acquired Pneumonia. View Table 4
Factors associated with increased risk in mortality among elderly with community acquired pneumonia are as follows: history of alcoholic drinking, renal disease, oxygen desaturation level of < 90% upon admission, decrease sensorium, hypotension, retractions & decrease breath sounds on physical examination, Escherichia coli in blood culture, mixed bacterial pathogen in sputum culture, and being classified as having high risk pneumonia (all p < 0.05).
The prevalence rate of pneumonia among elderly patients admitted in the study was 5%. In the Philippines, the incidence of CAP per 100,000 discharges is 4205 patients (4.2%) and when plotted against age group, it was noted to have a U-shaped curve indicating impact of burden on the youngest and oldest groups [11]. The older group tended to have higher case fatality rate secondary to pneumonia.
Many studies reported that community acquired pneumonia has higher prevalence in male gender (usually aged 65-74) [5,12-15], but in our study, it revealed that it is more commonly associated to female than male, this is because the female population in our country is more than males. Lifestyle factors such as smoking and alcohol drinking were associated with increased risk of mortality in pneumonia among elderly [1,16]. In our study, only alcoholic drinking is associated with mortality risk. In the study of Chebib, et al. it stated that alcohol consumption has a dose dependent effect and for older drinkers, they are more at risk for severe type of pneumonia and in-hospital mortality when compared to non-drinkers [17].
Pneumococcal vaccination and previous occupation was not stated in the history upon review of records of patients. The information could be useful in assessment of program implementation regarding the use of Pneumococcal vaccines among elderly and its effect in prevention of primary episode of community acquired pneumonia [6,18-20].
Given that majority of elderly patients have multiple co-morbidities that increases their risk for pneumonia, this study showed that most of elderly admitted have diabetes, renal disease, heart failure as well as pulmonary tuberculosis and hypertension similar to other studies [4,12,14,19,21-23]. Among numerous underlying conditions evaluated, the study showed that renal disease has an increased risk for mortality among elderly with community acquired pneumonia. In a 2-year, prospective population-based cohort study of hospitalized elderly patients with pneumonia of Arnold, et al., it revealed that having renal disease, heart failure and staying in nursing home residence were associated with longer time in clinical stability, longer length of stay in hospital and higher mortality [12]. Older adults have an impaired immunity owing to multiple factors such as immune senescence, chronic diseases, polypharmacy, malnutrition, and functional impairments which predisposes to infections like pneumonia.
The clinical manifestations of elderly with pneumonia stated in various literature were not limited to respiratory symptoms but usually presented with atypical symptoms such as body weakness, changes in sensorium, loss of appetite and can significantly increase the risk of mortality among elderly [8,9,16,22,24-26].
In study of Yoshikawa, et al. fever which is a cardinal sign or symptom of infection was observed only in one third of the elderly population [19]. There are also changes in lung physiology which predisposes elderly to pneumonia which includes decreased elastic recoil, increased air trapping, decreased chest wall compliance and reduced respiratory muscle strength [27]. These factors would increase the work of breathing, however as one gets older, less respiratory, and fewer symptoms were reported since delirium and cognitive impairment became more prominent in advance age [26]. This might be the reason wherein difficulty of breathing was observed more in patients less than 74 years old in the study. These atypical presentations may lead to diagnostic delays and may hinder appropriate intervention in elderly.
Upon admission, the presence of the following signs and symptoms such as decreased breath sounds, and retractions were noted to be significantly associated with mortality among elderly with pneumonia. As cited in the clinical practice guideline of community acquired pneumonia in immunocompetent adult in the Philippines, higher risk stratification was given to adult patients presented with decrease in sensorium, hypoxemia and/or hypotension [10]. In addition, Lupisan, et al. identified that drowsiness and hypoxemia is an independent risk factors associated with mortality. Hence, the presence of these findings in an elderly would warrant a more aggressive treatment [12].
Elderly patients presented with a baseline oxygen level of less than 90% was associated with increased risk of mortality in our study which are also similar with other studies [12,15,28]. In fact, oxygenation level was one of the criteria recommended by Myint, et al., when they develop SOAR (Systolic Blood Pressure, Oxygenation, Age and Respiratory Rate) Criteria as an alternative Pneumonia Severity Index for Elderly. Respiratory Failure is the leading cause of Death among patients with pneumonia [29].
In our study, there was no association of chest X-ray findings to mortality among elderly patients with pneumonia. This is in contrast to a study done by Mangen, et al. which showed that radiographically confirmed pneumonia has a two-fold higher mortality risk than those without radiographically non-confirmed pneumonia. Plus, poor film quality of standard chest radiograph was seen in elderly may well be because of patient's poor cognitive status, poor muscle strength, and inability to take care of posture during the procedure [8]. Some elderly patients have multiple co-morbidities and chest wall abnormalities which can complicate the interpretation of chest radiographs. Our study revealed normal chest x-ray findings present in 6.28% of patients. As cited by Gonzalez, et al., up to 30% of cases radiologic signs might not be evident especially in elderly with neutropenia and dehydration. Thus, when clinical findings of pneumonia are highly suspected, it is recommended to repeat radiography at 24-48 hours [18].
Majority of the studies identified the most common etiologic agent in sputum culture in elderly patients with community acquired pneumonia is Streptococcus pneumoniae. However, this was not seen in our study. The most common isolated pathogen is Streptococcus parasanguinis which may be a contaminant, followed by Klebsiella pneumoniae and other gram-negative bacilli. In Philippines antimicrobial resistance surveillance program annual report 2018, the most common pathogen in respiratory isolates was Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter baumannii [30]. Same pathogens were also identified in the study of Han, et al. [15]. Additionally, Azmi, et al., identified that Klebsiella pneumoniae is a typical community acquired pneumonia pathogen in Asia Pacific [11]. This was also seen in studies by Song, et al., that Klebsiella pneumoniae was endemic in countries like Taiwan, Malaysia, Thailand, India, and therefore the Philippines (all > 10% of total CAP cases), which showed a stark contrast to East Asian countries (usually 5%) [7]. Both Klebsiella pneumoniae and Acinetobacter were identified frequently as mixed pathogen infections in our study which is associated with mortality risk. The presence of bacterial co-infection was usually seen among older patients with multiple co-morbid conditions [8].
The different pathogens, sputum cultures with no growth and no specimen for cultures obtained in our study may indicate poor specimen collection on majority of elderly patients since most of them have swallowing disorders, decrease cough reflex and cognitive impairment that hinder proper specimen collection [8,9]. Elderly has an increased risk for pharyngeal micro aspirations which aid in colonization of gram-negative bacilli and other uncommon organisms in pharynx [18]. The 2018 Longitudinal Study on Aging and Health in the Philippines also revealed that older Filipinos have a poor level of oral health as indicated by the low number of natural teeth and lack of dentures. This factor may additionally contribute to susceptibility to pneumonia.
The study revealed that Escherichia coli in blood culture is associated with increase risk in mortality among elderly with pneumonia. The most common isolated organism in blood culture is Escherichia coli, Micrococcus and Staphylococcus. In Philippine antimicrobial resistance surveillance program annual report of 2018 [30], the most common pathogen isolated in blood was Coagulase negative Staphylococcus, Staphylococcus aureus and Micrococcus sp. which was similar to the study.
Pneumonia in the elderly happens fast and the prognosis is poor, and elderly are susceptible to moderate to severe pneumonia. The mortality rate of CAP moderate to severe in our study is 23.37%. The mortality rate for severe pneumonia is as high as 20% in the United States [31] and the reported mortality rates varied between 12% in Malaysia and 30% in Indonesia, depending on the country, study population, and hospitalization [7].
Elderly patients have different demographic profile and clinical characteristics which makes them susceptible to CAP infection. The study revealed prevalence of CAP in elderly was 5% in our institution. It is important also to take note of the risk factors associated to mortality. The presence of these factors serves as indication for immediate referral and aggressive management. This study serves as a baseline study in the Philippines and aims to provide information on elderly patients with community acquired pneumonia.
The study is underpowered due to small study population taken. This can be a reason why some risk factors which are significant in large population research were not significant in present study. Study did not include laboratory parameters and pneumonia severity indexes which might provide additional association to risk factors of mortality among elderly with community acquired pneumonia. It also did not include antimicrobial resistance profile of the pathogens identified. These may provide additional information regarding commonly identified pathogen per age group and its proper antibiotic guidance based on available antibiogram of the institution. Despite these limitations, the data generated from this study may contribute to the CAP data in the Philippines.
The authors would like to thank Quirino Memorial Medical Center for allowing us to access data for the purpose of this research. We would like to thank the Research and Ethics Committee of Quirino Memorial Medical Center for approval to undertake this study. We would like to thank the experts who participated and provided input during conceptualization and finalization of the study.
None.
N/A. All authors contributed equally in this research.