The purpose of the medico-surgical treatment of hip fracture in people aged 75 and over is to restore patients with a functional independence that is closest to that pre-fractured, while being as little aggressive as possible, at the shortest possible time and at the lowest financial cost. With this in mind, it is necessary to provide intensive rehabilitation at the beginning of the fortuitous "patient-hip fracture" in order to enable social reintegration as quickly as possible. This usually requires a multidisciplinary approach that can be provided in dedicated geriatric units.
Geriatric Peri-Operative Unit (UPOG), Hip fracture/Proximal femur fracture, Fracture of the upper extremity of the femur, Fracture of the upper end of the femur, Elderly, Geriatrics, Patient care pathway
Suffer a hip fracture (HF) is undeniably the most common pathology found in Traumatology. It is the third most common type of fracture in trauma (11.5% of fractures found in emergency rooms). In the elderly, it is the first most common cause of hospitalization in trauma emergency and the second most common cause of overall hospitalization. Moreover, it is the third budgetary allocation for health from Social Security: According to the French national hospital discharge database (Programme de Medicalisation des Systèmes d'information, PMSI), direct costs of HF have been estimated at 475 million euros and overall annual costs at 700 million euros in 2009 [1,2].
HF occurs mainly as a result of minor trauma (i.e. a fall from a height) and is the result of osteoporosis. The profile of the victims is often confused with that of an "old man" in poor health, linked to the increase of the ageing French population. In almost three-quarters of cases, patients are female (76.4%; sex ratio of 3:1 [3-9]) half of whom are 80-89 years-old. Victims are often poly pathological: Almost all people aged 70 and over have at least one chronic disease, 50% of them have up to 5 or 6 chronic diseases, and 50% of people aged 75 and over consume 7 or more different medications per day.
HF is truly taking on epidemic proportions, potentially over whelming many care and health systems. Its growing number will be a challenge for trauma services, which have now to deal not only with HF but also with the associated medico-social conditions. 50,000 new HF occur each year in France [10], responsible in 2014 for 76,100 hospital stays in medical services, surgery, gynecology and obstetrics in people aged 65 and over [1,11-13] (representing a lifetime incidence rate for people aged 50 and over from 17% to 22% for women and 6% to 11% for men [14-17]). If there was one figure to remember in the coming years, it would be this: By 2050, HF figures could reach 2.26 to 6.3 million people per year worldwide [18,19] and 150,000 people per year in France (given the increase in life expectancy and the impact of the baby-boom in France) [3,10]. HF is not without mortality: Intra-hospital between 2% and 4% [18,20,21]; extra-hospital, 4% to 11% at one month, 13% in the first three months, 13% to 18% at six months [22], 24% at one year [18,20-23], 50% at five years.
The elderly suffer therefore from their comorbid terrain. Compared to young people, geriatric patients are 10 times more likely to suffer from comorbidities and their perioperative risk is multiplied by around 2. Despite the evolution and progress of medicine (particularly related to orthopedic surgery and anesthesia-resuscitation), a multidisciplinary and systemic approach of the elderly person was created. This new model would allow to better aim for the objectives sought to be achieved and to distinguish between the elderly with harmonious and non-harmonious ageing, in order to restore their functional independence to that of before their HF as soon as possible [24-29]. From this observation ortho-geriatrics was born. Different ortho-geriatric unit models have been developed and the 6- to 10-bed ortho-geriatric unit located geographically in the orthopedic unit, providing geriatric care from admission to discharge (Unit for orthopedic Peri-Operative Geriatric care, UPOG) seems to be the most efficient and achievable unit model anywhere in the world with a good cost- benefit ratio [29]. The first French UPOG was created in 2009 at the Hospital de la Pitie-Salpêtrière (Paris) and in 2018 at University Hospital Center Cochin (Paris) opened its own UPOG. The objective of our study is to determine whether management of traumatic HF in UPOG decreases mortality at one year after hospitalization in UPOG and to identify the associated factors of this mortality.
This is a mono-centric retrospective observational study with cohort comparison. The study was conducted on University Hospital Center Cochin, and more specifically on its orthopedic department and UPOG.
Our study deals with men and women aged 75 and over, hospitalized in the orthopedic ward and UPOG at University Hospital Center Cochin (Paris), between November 2015 and November 2017, for the management of traumatic HF, either fracture of the femoral neck or fracture of the massive trochanteric. HF could be operated on or not operated on. People hospitalized in a ward other than the orthopedic unit and UPOG were not included. Those who were excluded, despite hospitalization in the orthopedic unit or UPOG: People under the age of 75 with HF; people aged 75 and over who suffered fractures other than HF; people aged 75 and over with multiple fractures; people aged 75 and over with pathological HF (primary bone tumor, metastasized of solid or hematological cancer); people aged 75 and over with co-arthritis and hospitalized for surgery for programmed hip replacement; people aged 75 and over hospitalized for hip orthopedic infection.
Included patients were targeted over two consecutive twelve-month periods. A patient's inclusion began in November 2015 and was completed in November 2017. The first collection period covered the year 2015-2016 (November to November). The subjects were hospitalized in orthopedics at Cochin Hospital and had exclusively an orthopedic expertise for their HF (in addition and at the request of orthopedic surgeons, one-time geriatric advice could be given). The second collection period covered the year 2016-2017 (November to November). Patients were hospitalized in Cochin Hospital but in UPOG, where in addition to the orthopedic expertise for their HF, they benefited from geriatric support by the geriatricians from Broca Hospital (Paris). The geriatrician was asked by orthopedics when a person aged 75 and over was hospitalized in orthopedics, whether for traumatic HF, multiple fractures with HF, pathological HF.
The first parameters collected included: the civil and demographic data of patients' age (years) and sex (male-1; woman-0); anthropological data of weight (kg) and size (cm); length of total stay and of post-surgical stay, specifying the date of hospitalization, date of intervention and date of discharge; death status measured at one month (thirty days), six months and one year (deceased-1; not deceased-0); the reason for hospitalization by fracture type (cervical fracture-1; pertrochanteric fracture-2; other-3); walking initially contra-indicated (yes-1; no-0); exit mode either in the center (-0) or at home (-1) or in EHPAD (-2). The establishment of comorbidities was inspired by the items of Charlson's age-adjusted score (combined score of the comorbidities of Charlson's score and age: 3 points for an age between 75 and 79 years, 4 points for an age between 80 and 89 years, plus 5 points for an age greater or equal to 90 years). However, these were adapted for the geriatric population. For example, the item "HIV with or without AIDS" was not studied given its low prevalence in people 75 years of age or older. All of the clinical items studied related to medical history: Heart failure (yes-1; no-0); high blood pressure (yes-1; no-0); diabetes (yes-1; no-0); stroke (yes-1; no-0) and in the case of a history of stroke, presence of a sequellar hemiplegia (yes-1; no-0); myocardial infarction (angor-1; post-angioplasty and/or post-bypass-2; none-0); obliterating arterial disease of the lower limbs (yes-1; no-0); chronic liver disease (yes-1; no-0); haemorrhage (yes-1; no-0); peptic ulcer (yes-1; no-0); connectivity (yes-1; no-0); homeopathy (leukemia-1; myeloma-2, lymphoma-3); cancer (yes-1; no -0) and in case of a history of cancer, cancer with metastasis (yes-1; no-2); thrombopenia less than 150,000/mm3 (ye -1; no-0); repeated falls defined here as at least two falls per year (yes-1; no-0); cognitive impairment (yes-1; no-0); dementia (yes-1; no-0); Folstein's MMSE score (between 0 and 30); chronic alcohol use (yes-1; no-0); chronic lung disease (yes-1; no-0). Some other comorbidities had to be assessed by intermediate criteria (biological items): Kidney failure via blood creatinine on admission (μmol/L); anemia via hemoglobin on admission (g/dL) and hemoglobin on exit (g/dL); protein-energetic under nutrition via serum or plasma albumin (g/L); thrombopenia via platelets level (/mm3); vitamin D deficiency through vitamin D (ng/mL) dosage. The following events during hospitalization were collected: Transfusion during hospitalization (yes-1; no-0); infection during hospitalization (yes-1; no-0). Functional independence was measured according to the following parameters: Parker's score on admission and Parker's score after one year (between 0 and 9); ADL scale on admission and ADL scale after one year (between 0 and 6). The occurrence of death was analyzed as follows: Intra hospital, at six months, at one year (yes-1; no-0), cause of death (free text), date of death (DD/MM/YYYY). Poly medication and the most commonly found the rapeutic classes in geriatrics were selected: Number of treatments on admission (digital value); antihypertensive (yes-1; no-0); anti diabetic (yes-1; no-0); benzodiazepine (yes-1; no-0); antidepressant (yes-1; no-0); neuroleptic (yes-1; no-0); morphine (yes-1; no-0); anti platelet agent (yes-1; no-0); effective and/or curative anticoagulant over the long term, by direct oral anticoagulant or anti-vitamin K anticoagulant (yes-1; no-0).
Patients' census was conducted during 2018-2019, based on data from University Hospital Center Cochin's PMSI. Data was collected after the study period, from 2018 to 2020, thanks to the patient's identity (name, first name, date of birth and permanent patient ID). Data was then anonymized during the statistical analysis procedure. Clinical parameter data was collected from computerized medical records in local software Actipidos Cochin® and Actipidos Broca®, for data from before the summer of 2018, and then Orbis® for data from summer 2018. Telephone calls and e-mails to patients, those they associate with to varying degrees (trusted persons, family, friends, neighbors, acquaintances), EHPADs and treating physicians were also needed to complete the data collection, according to the information of these coordinates in computerized medical records. Data on biological parameters was retrieved via local software Stare®.
The primary endpoint of our study is one-year mortality after HF surgery. Intermediate stages of the study of mortality at one month (thirty days) and six months were also taken into account to distinguish between the occurrence of early (< one month) or late (> six months) mortality. The secondary endpoint is factors associated with one-year mortality after HF surgery.
Assuming a baseline one-year mortality rate of 30% (source: Guzon-Illescas O, Perez Fernandez E, Cresp-Villarias N, Quirs Donate FJ, Pea M, Alonso-Blas A, Garcia-Vadillo A, Mazzucchelli R, Mortality after osteoporotic hip fracture: incidence, trends, and associated factors, Journal of Orthopedic Surgery and Research (2019) 14:203) and a mortality reduction of 30% in the geriatric cohort (from 30% to 20%), we estimated that we would require 154 patients to obtain an 80% power with a two- tailed first-species risk (α) at 0.05.
Data was coded from Excel®. Statistical analysis was carried out with the software ‘R' version 3.1.3 (R Foundation for Statistical Computing, Vienna, Austria). Patient characteristics were studied using simple descriptive statistics: Average and standard deviation for continuous variables, number and percentage for categorical variables. Adapted univariate tests were used to compare patient characteristics by period of hospitalization: Student test for continuous variables and Chi-2 test for category variables. Non-parametric tests were used when the validity of the usual tests was not verified. Determinants of mortality were studied using a multivariate analysis. Two multivariate analyses were performed: A logistic regression model with the use of an adjustment on age and sex and confounding factors, allowing to calculate odds ratio (OR) and confidence intervals at 95% (CI 95%); a Cox model with the use of an adjustment on age and sex and confounding factors, calculating hazards ratio (HR) and 95% confidence intervals (CI 95%). Graphic representations were also made: "Kaplan-Meier Curve" to represent the survival function, "Forrest plot" for the logistic regression model. All p values were two-sided and p < 0.05 was considered significant.
As studies reporting research involving human participants, this specific study was reviewed and approved by an institutional review board (ethics committee) before the study began. This study received a favorable opinion from the ethics committee GEROND'IF, the geriatric organization of the Ile-de-France region.
The need for consent was waived by the ethics committee.
From November 2015 to November 2017, 620 patients aged 75 and over were admitted to Cochin Hospital for HF. 469 patients were analyzed and divided into 255 patients in the orthopedic cohort and 214 patients in the geriatric cohort (UPOG) (Figure 1).
 Figure 1: Flow-chart.
View Figure 1
Figure 1: Flow-chart.
View Figure 1
The majority of patients were female (76.33%) and corresponded to a geriatric patient since they were on average almost 87-years-old (86.90 years). Functional independence levels were on the ADL scale at an average of 4.5/6 (ADL 4.58) and on the Parker scale at an average of 6/9 (Parker score 6.32). Patients carried a polypathology, with an average of around 7 comorbidities (Charlson score 7.19) of which the 5 most represented were high blood pressure (59.4%), neurocognitive disorders (59.38%), major neuro cognitive disorders (41.3%), cancer disorders (27.35%) and repeated falls (24.36%). The average number of daily medications was close to 5 (4.80%), and 1st place was occupied by antihypertensive treatments (60.22%). Nutritional status referred to under nutrition according to the WHO biological criteria with serum or plasma albuminuria around 31 g/dL, but anthropometric status was maintained since BMI was greater than 21 kg/m2. Note that here we did not consider in flam matory and/or infectious perioperative and perioperative conditions which can interfere with the rate of albumin. Patients were hospitalized at Cochin Hospital for cervical fracture (51.17%) or for pertrochanteric fracture (48.83%). For hospital stays, the total average length of stay was 9.72 days. After surgery the average length of stay was 8.07 days. Patients were mainly transferred to rehabilitation (68.44%) (Table 1 and Table 2).
Table 1: All patients' characteristics. View Table 1
Table 2: Patients' characteristics in the orthopedic cohort and the UPOG cohort. View Table 2
One-year mortality after HF surgery does not differ statistically between the two cohorts studied (p = 0.78), it amounts to almost 18% in each group analyzed (17.63% in the total base). Intermediate mortality was also studied: Intra-hospital, one-month and six-months. Intra-hospital mortality is significantly lower in the geriatric cohort than in the orthopedic cohort (p = 0.02), it is 0.47% in the 1st group compared to 2.75% in the second group, and 1.71% in the total base. One-month mortality after HF surgery does not differ between the geriatric cohort and the orthopedic cohort (p = 0.19; 3.17%). Six-month mortality after HF surgery does not differ statistically between the two cohorts studied (p = 0.89): It is almost 12% (11.34%) (Figure 2).
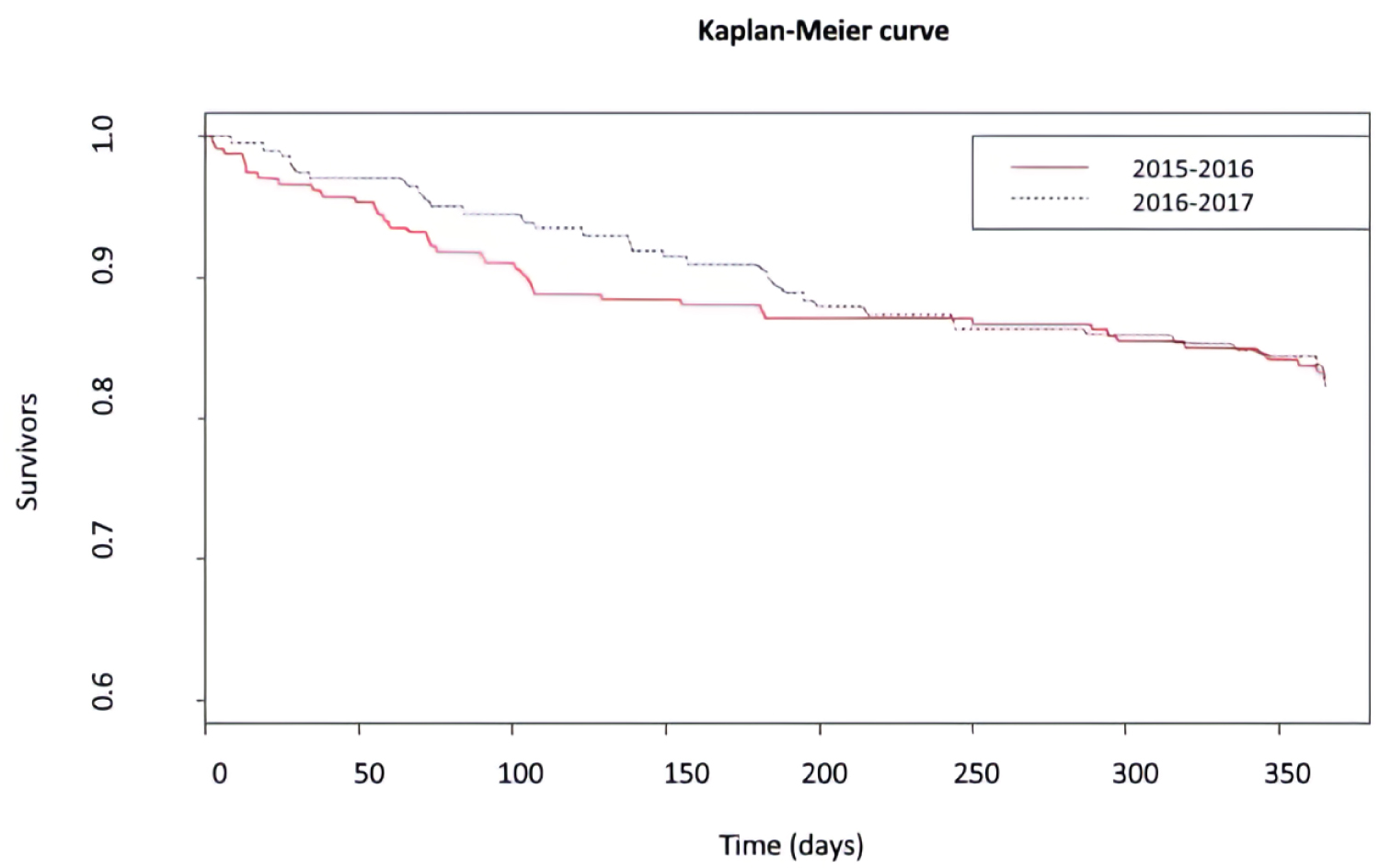 Figure 2: Kaplan-Meier curve.
View Figure 2
Figure 2: Kaplan-Meier curve.
View Figure 2
Factors associated with one-year mortality after HF surgery according to the study cohort are shown in the following diagrams (Figure 3, Figure 4 and Figure 5).
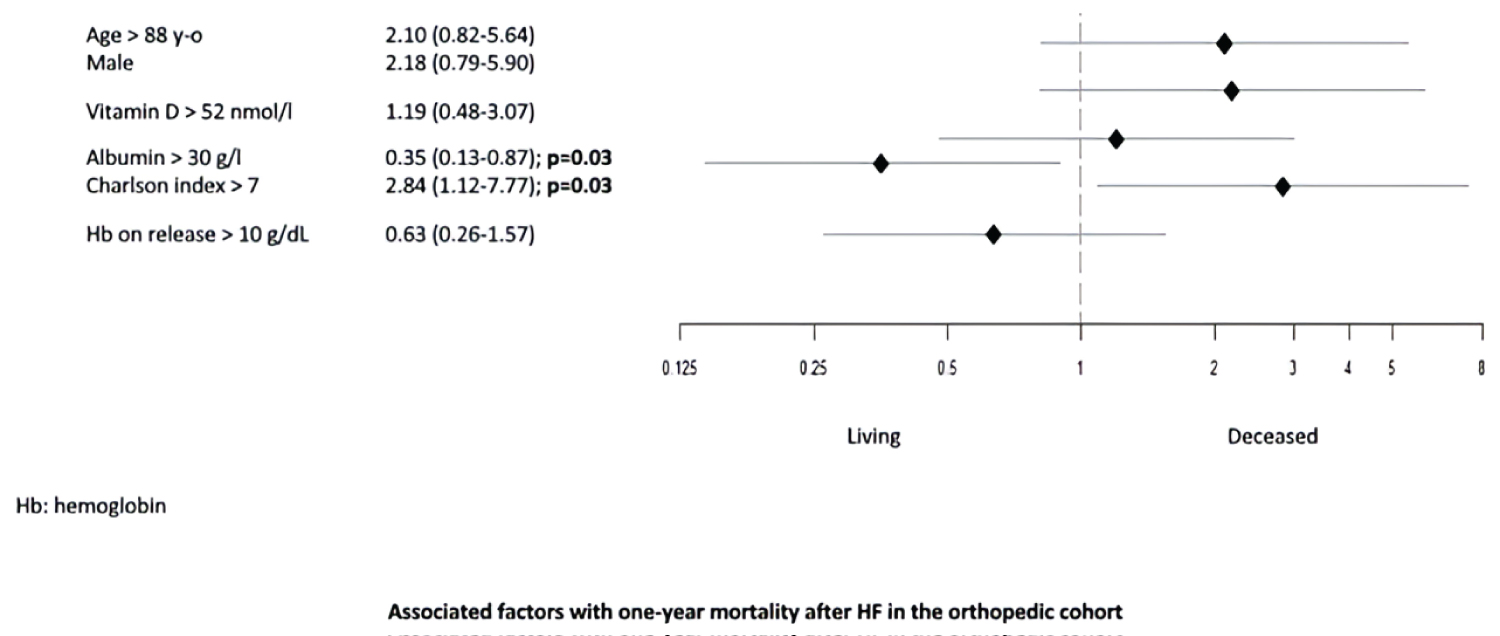 Figure 3: Associated factors with one-year mortality after HF in the orthopedic cohort.
View Figure 3
Figure 3: Associated factors with one-year mortality after HF in the orthopedic cohort.
View Figure 3
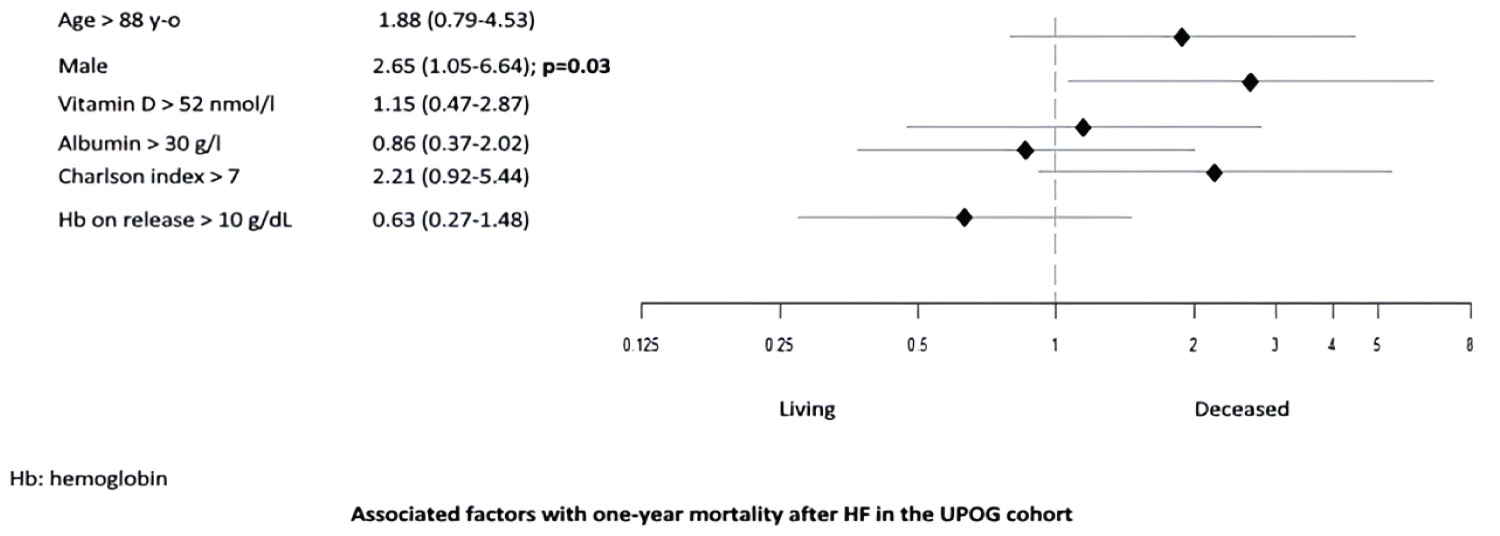 Figure 4: Associated factors with one-year mortality after HF in the UPOG cohort.
View Figure 4
Figure 4: Associated factors with one-year mortality after HF in the UPOG cohort.
View Figure 4
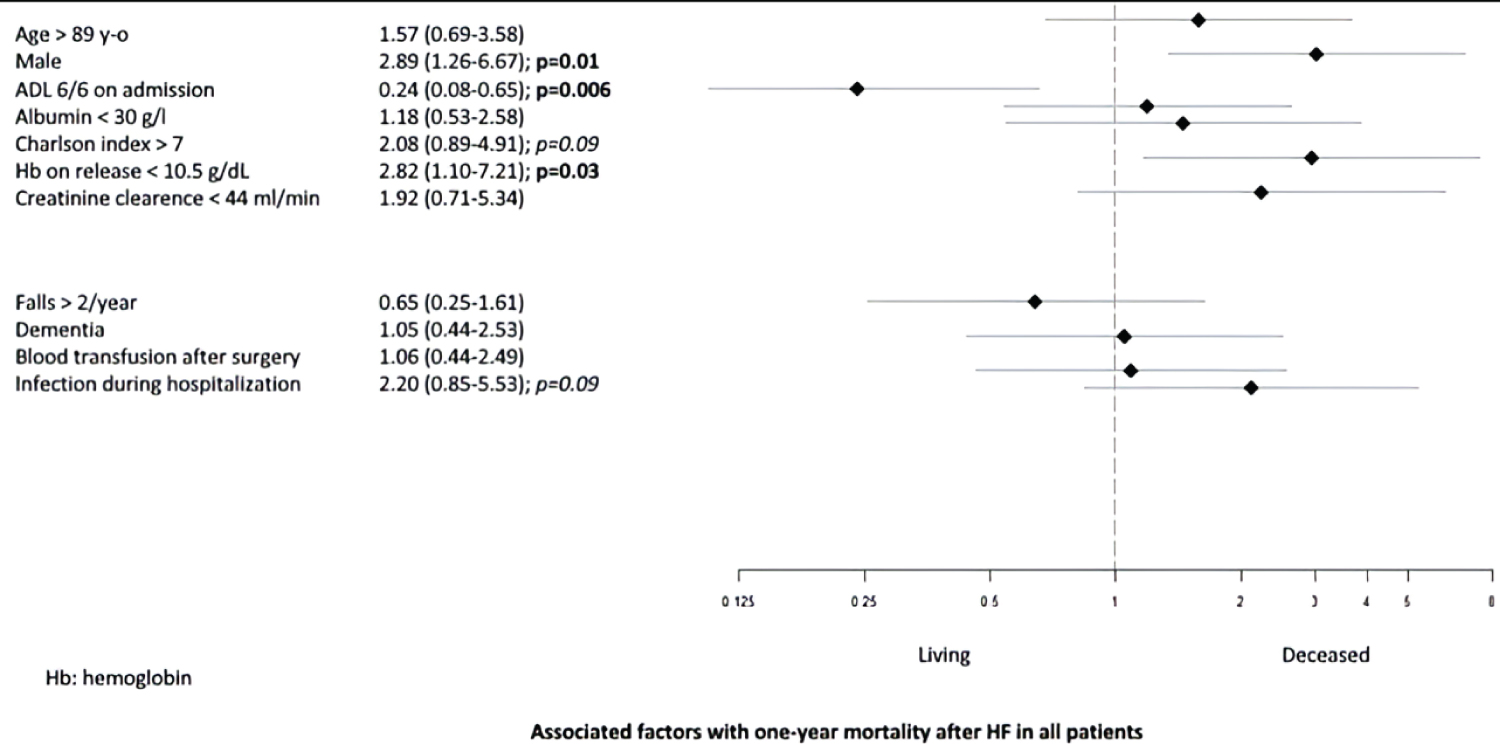 Figure 5: Associated factors with one-year mortality after HF in all patients.
View Figure 5
Figure 5: Associated factors with one-year mortality after HF in all patients.
View Figure 5
Factors related with one-year mortality after HF surgery were: Male sex, comorbidities with Charlson score > 7, nutritional status with albumin rate < 30 g/l, anemia at release with Hb < 10.5 g/d. One protective factor related with one-year mortality after HF surgery was found: Anterior autonomy with ADL scale 6/6 on admission.
At one year from hospital discharge, we showed no decrease or even difference in mortality after HF surgery in the geriatric group compared to the orthopedic group. This may be because after their hospitalization in orthopedics or UPOG at Cochin Hospital, patients were not regularly reassessed by a geriatrician, or even simply by a physician. The absence of follow-up consultation (at one month, three months or six months for example) may have resulted in them not maintaining the initial benefit of UPOG care. HF should therefore be considered as a serious geriatric pathology to be managed over the very long term. To our knowledge, no national or international study has yet sought to analyze one-year mortality after HF surgery and hospitalization in UPOG compared to hospitalization in the orthopedic unit. Therefore, we cannot comment on our work on this. As for one-year mortality after HF surgery for those aged 75 and over, we found that one-year mortality after HF surgery in our total base of patients aged 75 and over approaches 18% (17.63%). This figure is slightly lower than that found in the literature, particularly in the 2016 DRESS survey, which reported mortality ranging from about 30% among those aged 75 to about 60% among those aged 95 [3].
The study of six-month mortality after HF surgery was not part of our study objectives. Despite this, in our study we did not see a difference in six-month mortality after HF surgery between our orthopedic cohort and our geriatric cohort. Compared to the cohorts in Pr. BODDAERT's study, our six-month mortality after HF surgery in the orthopedic cohort and in the geriatric cohort is somewhat lower: In our analysis we find 11.54% and 11.11% respectively when the Pitie-Salpêtrière Hospital's team finds 24% and 15% respectively. All of these results are similar to those in literature which are between 13% and 18% at six months [22].
As in our current study, Pr. BODDAERT's team showed that age, male sex and comorbidities were predictive factors for mortality that were distributed differently between the orthopedic cohort and the geriatric cohort. As for the comparison of patients living and deceased after their HF, our study showed that, more than anything, it is sex and functional independence status that really impact the occurrence of one-year mortality after HF surgery: Male sex is a provider of one-year mortality after HF surgery and pre-fracture total functional independence on ADL scale protects against one-year mortality after HF surgery. Literature is consistent with this conclusion as it highlights patient's health status, age and gender as the three most correlated elements to survival.
Our study has two main positive points. We conducted an original study about one-year mortality after HF surgery in an orthopedic unit and an ortho-geriatric unit. Interest in a geriatric cohort is usually under studied, we don't know of any similar national or international studies with as large an analyzed population. In our study, we analyzed our primary focus (i.e. one-year mortality after HF surgery) using two statistical models of multivariate analysis: A logistic regression model and a survival model. Both adequately found the same associated factors which were statistically significant for one-year mortality after HF surgery. This sensitivity analysis thus demonstrated the statistical strength of these associated factors considered to be potential risk factors for one-year mortality after HF surgery.
Our study has several limitations. First of all, it was a retrospective and observational survey, i.e. with low levels of evidence according to the French high authority of health (Haute Autorite de Sante, HAS). The study's design responded to that of before/after studies with site contemporary control of the intervention. The HAS recalls in a June 2007 report that "the major difficulty of these studies is to find a population-control comparable in every way to the population-intervention. It suggests the results of before/after studies may overestimate the effects of interventions aimed at improving the quality of care. This type of study simply shows in reality the practice's evolution, without it being possible to say that the observed changes are related to intervention [30]. In addition, the orthopedic cohort we have form eddoes not fully fit the definition of an "orthopedic" cohort as we may see at first glance. Indeed, in 2015-2016, individual geriatric advice was given two half-days per week by the geriatricians from Broca Hospital for orthopedic patients at Cochin Hospital. This cohort is therefore not in fact a pure orthopedic cohort and this element may have influenced the results on the lack of difference in six-month mortality after HF surgery compared to the cohorts in Professor BODDAERT's study. As for missing data in our study and with respect of the primary endpoint, we collected between 5.49% and 8.63% of missing data mainly due to patients lost to follow-up and data collection pitfalls (for the item "death at thirty days": 5.49% in the orthopedic cohort and 6.07% in the geriatric cohort; for the item "death at six months": 8.24% in the orthopedic cohort and 7.48% in the geriatric cohort; for item "death at one year": 8.63% in the orthopedic cohort and 7.48% in the cohort).
In this population of very old patients studied in "real life", intra-hospital mortality is significantly reduced in the geriatric cohort compared to the orthopedic cohort. However, one-year mortality after HF surgery is similar in both groups.
Specific studies in ortho-geriatrics are needed to better assess, on the one hand the patients' path of care after discharge from hospital following HF surgery, and on the other hand, the overall long-term medical-socio-economic contribution of UPOG management.
Dr H. Bouloudani is the designated author signing on behalf of all co-authors of the contribution.