Musculoskeletal disorders can be acute or chronic conditions of the musculoskeletal system and are prevalent within the dental profession. Dentistry is a high-risk profession for musculoskeletal disorders due to the use of repetitive hand movements and the adoption of prolonged static procedures. These have been identified as a prevalent cause of early retirement and have been shown to develop during dental training and education. The reported high rates of musculoskeletal disorders in dental and dental hygiene therapy students is a significant cause for concern.
Following university ethical approval, a questionnaire was designed, piloted and distributed to dental students in the third and fourth Bachelor of Dentistry (BDS) cohort. Questions investigated the prevalence of back/neck pain along with other clinical factors identified as risk factors for musculoskeletal disorders, including use of indirect vision, work-place adaptations and four-handed dentistry.
A total of 102 questionnaires were returned from a potential 148 students a response rate of 68.9%. 76.5% (n = 78) of students questioned reported experiencing pain in the neck or back following a clinical session. Of those who experienced pain, 67.9% experienced pain at least once a month or more. 21.6% of students were unsure of the correct height to place their patients to optimise their posture during treatment, and a further 57.8% were only slightly aware. Furthermore, 89.2% of students felt that they did not have adequate nursing support to maintain good posture; 50% had not experienced four-handed dentistry with a nurse; and 7.9% very confident to use their mirror for indirect vision.
The prevalence of neck/back pain within this study is similar to those reported internationally within the literature. High prevalence rates within dental students is a concerning finding that may have significant implications for individuals and the profession. The strongest evidence within the literature supports resistance training and stretching exercise programmes for prevention of musculoskeletal disorders. Students should be educated of the risks, and these preventative strategies should be encouraged within dental education programmes. Greater interventional studies are required.
The authors confirm that this work is an original piece of work. There are no conflicts of interest and no author has received funding or reimbursements regarding the content of this research.
Musculoskeletal disorders (MSD), Work-related musculoskeletal disorders (WRMDs), Posture, Dentistry, Dental students
Musculoskeletal disorders (MSDs) are injuries to the musculoskeletal system (bones, ligaments, muscles, tendons, joints, nerves). They can be acute or chronic and have been associated with a wide array of signs and symptoms that are listed in Table 1 [1].
Table 1: Signs and symptoms of musculoskeletal disorders. Adapted from Graham C - Ergonomics in Dentistry, Part 1 [1]. View Table 1
Whilst the aetiology may be multi-factorial, occupation has been identified as a risk factor for MSD [2-4]. Evidence within the literature would suggest that dentistry is a high risk job for development of MSDs [5] and multiple studies have recorded prevalence rates greater than 50% in the neck/shoulder region [6-9]. Furthermore, a 2009 systematic review of the literature, concluded that "MSD represent a significant burden for the dental profession", with prevalence rates of 64-93% reported [10]. One Australian study found that one dentist in every ten had taken sick-leave due to MSD within the previous twelve months, with 11.5 days of leave required on average [11]. Whilst in the United Kingdom (U.K.), MSDs was at one time reported to be the primary cause of early retirement in 29.5% of the dentists surveyed [12]. Work-related MSD (WRMD) has also been widely reported in other health-care professions such as nursing and medicine [13].
Valachi and Valachi [14] highlighted several risk factors for MSD in dentistry, which include: Prolonged static procedures (PSPs); repetitive movements (RMs); suboptimal lighting and poor positioning. Specific specialties or procedures within dentistry were also suggested as risk factors, with hygiene/therapists more likely to undertake RMs, and those practicing four-handed dentistry likely to occupy PSPs for longer. Poor positioning and PSPs can potentially result in muscle imbalance and ischaemia, with inadequate rest between sustained muscle activity considered as a mechanism for pain development, joint hypo-mobility and joint degeneration. This proposed mechanism for MSD development is covered elsewhere [14].
A number of publications have discussed the importance of prevention in avoiding and reducing risk of MSD, with some suggestions for this listed in Table 2 [1,14-16].
Table 2: Suggestions and tips for preventing muscle strain and musculoskeletal disorders in the clinical setting [1,14-16]. View Table 2
It has been suggested that age, [6,11,17] gender [18,19] and patient treatment time [6] can affect the prevalence rate of WRMDs. Studies have shown that MSD can develop early in clinical careers [20] and older practitioners have been shown to be less likely to suffer from MSD [6,11]. However, this finding may reflect the fact that those who suffer with significant MSD have often left the profession. For this reason, it is possible that current prevalence data under-represents MSD within the profession and greater incidence studies are required. Whilst work remains a potential risk factor for MSD, well-designed work has been encouraged for those that are suffering from MSDs [4].
A range of recent research has focused their investigations on the prevalence of WRMDs in dental and dental hygiene/therapy students. A review of the literature by Gupta, et al. highlighted that students in dental education were exposed to MSDs and that greater preventive measures are required within dental programmes [21]. Ng, et al. reported prevalence of MSDs in at least one body area to be 85% in oral health and dentistry students in Australia [22]. This was mirrored in another questionnaire based study from Columbia which recorded 'muscular pain' of 80% in dental students [23]. Ng, et al. also reported the highest level of 'poor posture' in final year dental students, which suggests that poor postural techniques are in fact learnt behaviours that develop during dental education. Morse, et al. summarised the prevalence rates of MSDs across the dental professions in 2009 [20]. It is clear from this research that students are at risk of MSDs and this raises pertinent questions regarding the role of dental education in developing and reducing the risk of MSDs. With this in mind, a pilot study was undertaken at a UK University dental teaching hospital to investigate MSDs in dental students. The aim was to assess prevalence of MSDs amongst this cohort, including their awareness of correct clinician posture, patient position and use of indirect vision, which have all been discussed as possible risk factors for MSD [20].
This cross-sectional, questionnaire based study was completed at a UK dental school. A short questionnaire was devised by the authors and piloted locally on hospital dental core trainees. Participants were recruited from two cohorts of dental students attending mandatory courses within the operative skills suite (phantom head suite). This included students from years 3/4 of the five year Bachelor of Dental Surgery (BDS) degree or from years 2/3 of a four year postgraduate BDS degree. Ethical approval was gained from the University Ethics Committee. All students in attendance during the data collection were given the opportunity to opt into the study. No exclusion criteria were outlined. The questionnaire collected basic demographic data (gender/year of study). Further questions were designed to investigate key factors identified in maintaining good posture (chair adjustments/patient & clinician positioning), good clinical practice (indirect vision/four-handed dentistry) and prevalence of MSDs.
A total of 102 questionnaires were returned from a potential 148 students a response rate of 68.9%. 65 students were from 4th year (63.7%) and 37 students from 3rd year (36.3%). Results were combined to give cumulative totals across the study as no differences were identified between groups. Participant demographics are reported in Table 3. 76.5% (n = 78) of students questioned reported experiencing pain in the neck or back following a clinical session (Table 4). Of those who experienced pain, 67.9% experienced pain at least once a month or more (Table 5).
Table 3: Descriptive data for sample gender and year of study (total number and %). View Table 3
Table 4: Percentage of students that have experienced pain in the neck/back following clinical activity. View Table 4
Table 5: Frequency of pain reported within the sampled dental students. View Table 5
Figure 1 shows the participant responses to a series of questions regarding posture, chair adjustments and patient positioning that may be associated with WRMD. Of note, 21.6% of students were not sure of the correct height to place their patient to optimise their posture during treatment, and a further 57.8% were only slightly aware. Table 6 shows the participants responses to questions regarding nurse support, four-handed dentistry and indirect vision. 89.2% felt that they did not have adequate nursing support to maintain good posture; 50% had not experienced four-handed dentistry with a nurse; and only 7.9% were very confident to use their mirror for indirect vision.
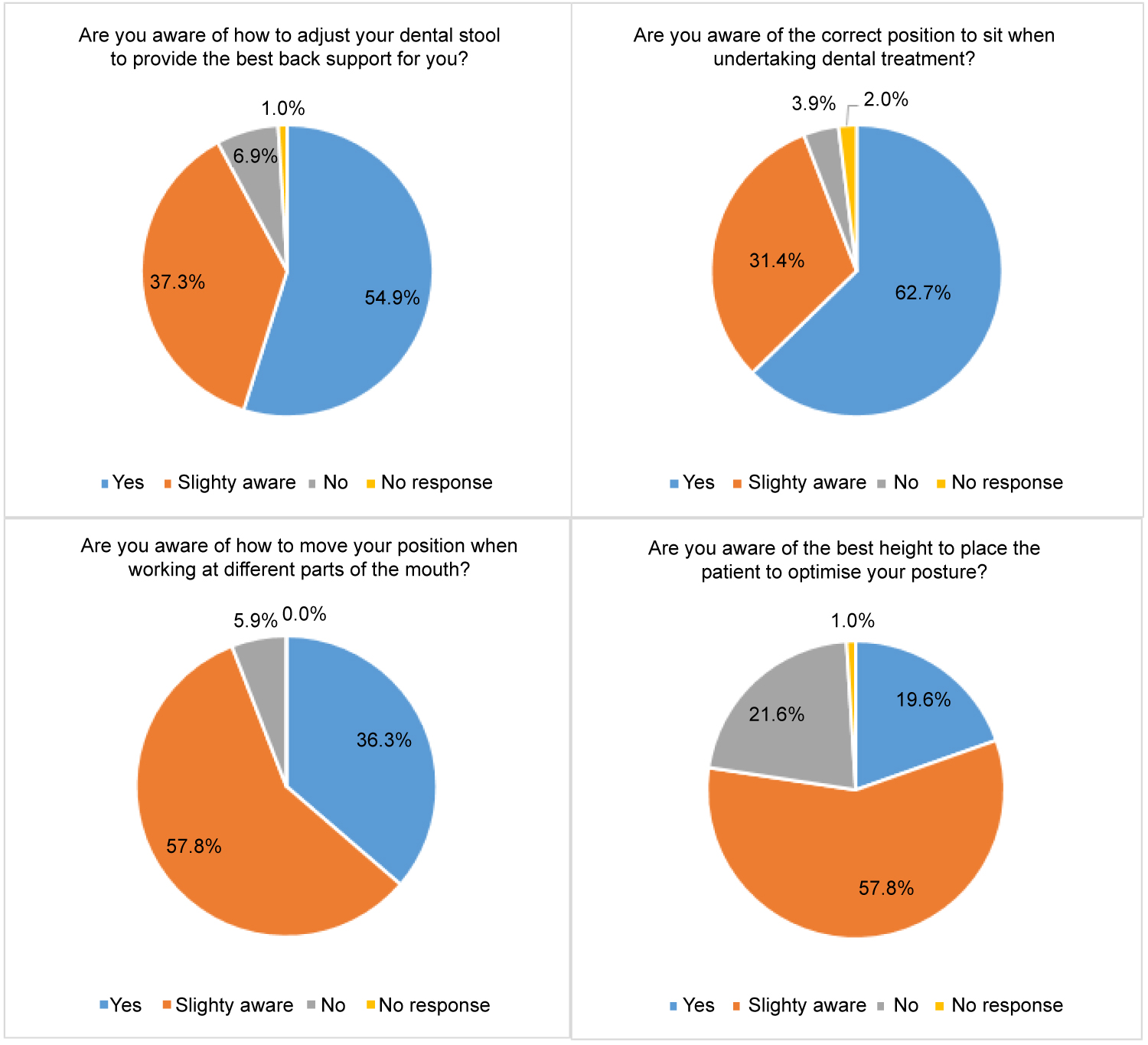 Figure 1: A table to show the frequency of participant responses to a series of clinical skill-related questions associated with WRMD.
View Figure 1
Figure 1: A table to show the frequency of participant responses to a series of clinical skill-related questions associated with WRMD.
View Figure 1
Table 6: Shows the participant response frequencies to a series of clinical questions linked with WRMD. View Table 6
It is widely acknowledged that clinical dentistry requires good manual dexterity and fine motor control to perform a wide array of procedures and tasks. Procedures are frequently lengthy and performed in a seated position with repetitive movements of the hands and wrists. The reported high rates of WRMDs in dentistry should be of great concern to the profession with WRMD a prevalent source of early retirement [12] and lost productivity [24]. Whilst a number of potential lifestyle factors would influence the development of WRMD, the practice of dentistry frequently involves prolonged static procedures and repetitive movements and as such makes dentists and DCPs at increased risk of WRMD.
Of great concern is the potential development of MSDs in dental students. As trainees, who are developing their clinical skills, in order to demonstrate competency in technically difficult tasks, [25], they are likely to take longer than qualified practitioners to complete similar dental procedures. In addition, they require more concentration and focus on a particular task [26] and as a result, students appear to be less likely to consider working posture and could be at greater risk of WRMD [20]. Furthermore, it is not clear the level of training dental students receive regarding the risks of poor posture and the development of good clinical practice. Four handed dentistry, good lighting, magnification and appropriate chair and patient positioning are but a few of the recommended modifications to improve clinical practice.
This pilot study suggests that back and neck pain is prevalent amongst dental students with 76.5% having experienced neck or back pain of which 67.9% experienced pain at least once per month. Whilst no causative links can be demonstrated with this study design, it is of some concern that 21.6% of respondents were not aware of the correct position in which to place their patient for treatment and only 26.5% of students routinely adjusted their chair at the start of clinical sessions to optimise their posture. Furthermore, 29.4% of participants were not confident in using indirect vision and 50% of participants felt they had no experience of four-handed dentistry with a nurse. These factors have been discussed as exacerbating factors for the development of MSDs. One Brazilian study [27] concluded that the practice of four handed dentistry had no influence over the prevalence of WRMDs, but alternative literature exists to support this practice and as such this remains a controversial topic [16,28]. Further well designed studies should be considered to investigate the causative role of work station set-up and ergonomics in the development of MSDs.
Despite a reasonable response rate of 68.9%, the use of negative consent incorporates selection bias into the study. It is possible that responses will be from those students more aware or with greater experience of MSDs and no explanation could be found for the lower response rate from dental students in year 3 of their studies. However, it could be that as their clinical experience was less than the 4th years, they did not yet perceive MSD as a potential problem. Furthermore, a number of important factors were not investigated and this introduces further confounding factors, which the authors are unable to mediate for. No information was collected regarding the age of subjects due to ethical reasons as this could have led to possible identification of participants. It would be beneficial in further studies to investigate the intensity of pain experienced; the location and duration of pain; the presence of pre-existing MSD; the use of any preventative strategies such as stretching and exercise and the amount of previous training in posture. Cumulative clinical time was another factor not investigated that would have enabled greater comparison across the entire cohort of dental students.
Despite these limitations, this study presents comparable prevalence data to a range of similar studies [6,9-11,17,19,22]. A recent publication from another UK dental school reported 79% of respondents reported at least one episode of neck, upper or lower back pain compared to 76.5% within this study [29]. As discussed above, these UK prevalence rates for self-reported back, neck and upper limb pain are comparable to studies from other countries such as; Australia (85%) [22], Columbia (80%) [23], Brazil (76.2%) [30], Malaysia (93%) [31] and the United States of America (61%) [32]. These findings suggest the issue of WRMDs is a global concern for the dental profession and teaching institutions.
A range of management strategies and workplace interventions to prevent MSDs have been proposed (Table 2). The use of a physical exercise programme was reported to reduce symptoms of lower back pain in one study of dental students [33]. However, it seems unlikely that dental schools worldwide will be able to adopt similar programmes into already congested curricula. A recent systematic review into the effectiveness of workplace interventions on WRMDs, highlighted strong positive benefits from resistance training and moderate positive benefit for stretching exercise programmes [24]. Interestingly, ergonomics training and adjustment of a worker's workstation had mixed findings and not enough evidence was available to inform current practice. It is therefore important that the two interventions with the strongest evidence-base should form the basis of dental education into the prevention of MSDs; resistance training and stretching exercise programmes. Educating students about the risks of developing MSDs is imperative, alongside encouraging students to take responsibility for their own health by adopting proactive preventative strategies. A MSDs student fact sheet may be beneficial for clinical university programmes.
It is clear from the findings of this study and the literature discussed within this article that dentistry is a high risk profession for MSDs. Of great concern, is the high prevalence reported amongst students studying dentistry and dental hygiene/therapy. Greater focus and education on the risk of MSDs within the undergraduate programme may encourage students to adopt greater postural habits and pursue beneficial lifestyle choices. Small group workshops on resistance training or stretching programmes are being considered locally to help guide students to adopt these strategies, as well as greater focus on posture and patient positioning during clinical sessions. Utilisation of student fact sheets or digital applications may further support decision making in this respect.
The literature spanning several decades remains dominated by prevalence studies and there appears to be sparse research into the effectiveness of workplace interventions in the prevention of WRMDs in dentistry. Further well-designed intervention studies should be performed to investigate strategies that will help inform dentists and dental care professionals how best to avoid MSDs and prolong their practicing careers. Future research within this field should adopt the Nordic musculoskeletal questionnaire (NMQ) [34] or a modified NMQ [29] to enable more accurate and repeatable comparisons across cohorts. Future comparisons across dental specialities may also assist with workforce planning and risk stratification.
This cross-sectional study highlights that MSDs are prevalent amongst a cohort of dental students within a U.K. dental school. Dentistry frequently relies upon excellent manual dexterity and fine motor control to complete a range of clinical treatments. Procedures often involve prolonged static positions and repetitive movements which have been suggested as possible causes for muscle pain and musculoskeletal disorders. A number of management strategies and workplace interventions have been discussed including resistance training, stretching programmes and workplace modifications such as adjustment of patient position and chair height, which should be adopted and taught by educational institutions.