Pediatric and youth diabetes mellitus (DM) and pediatric and youth human immunodeficiency virus (HIV) infection are among the chronic diseases with significant public health implications and high mortality. The availability of mortality statistics in type 1 diabetes and HIV/AIDS is critical for addressing the two conditions in one setting.
To compare the mortality of children and youth living with Diabetes (CYLDM) versus children and youth living with HIV (CYLHIV).
This retrospective cross-sectional approach extracted data from registries of Tanzania Diabetes Association (TDA) and National AIDS Control Programme (NACP). Mortality was defined as death recorded in the registry. STATA version 14 was used for analysis.
A total of 3822 data for CYLDM and 33,941 CYLHIV were extracted. Almost fifty-one per cent (50.8%) and 27.2% were males CYLDM and CYLHIV respectively, mean age (SD) at diagnosis was 14 (± 5.8) and 9.4 (± 7.3) years for CYLDM and CYLHIV, respectively.
Total death was 95 (3.0%) in CYLDM and 3718 (11%) in CYLHIV. Mean age (SD) at death was 17 (± 4.5) years for CYLDM and 11 (± 8) years for CYLHIV. The loss to follow up rate was 33.7% for CYLDM and 43.7% for CYLHIV.
The estimated death rate was high in CYLHIV compared to CYLDM. Both conditions had a high rate of loss to follow up. This study serves as the basis for prospective studies to determine causes and possible mitigation against mortality and loss to follow up in these two chronic conditions.
Mortality rate, HIV infection, Type 1 diabetes, Mortality, Children, Youth
Type 1 Diabetes Mellitus (T1DM) and Human Immunodeficiency Virus (HIV) infection are two frequent chronic conditions in children and youth, that create an economic burden to families and countries at large [1,2]. Both have contributed to mortality and morbidity in this age group, even though HIV is an infection while diabetes mellitus is a non-communicable disease. HIV is the leading cause of mortality in adolescents and young people in Africa and the second globally [3] after unintentional injuries. Globally, during the year 2020, about 2.8 million children and adolescents (0-19 Years) were infected with HIV [4] and 5.8% of them were in Tanzania [5] with 260,000 new cases yearly [6]. On the other hand, diabetes Mellitus is one of the top 10 causes of mortality globally [7]. It affects about 1 million children and adolescents (< 20 Years) [8]. Mortality due to Type 1 Diabetes Mellitus (T1DM) is still high in most Sub-Saharan African countries due to the high rate of acute complications [9,10], missed diagnosis [11] and lack of adequate health structures required for the disease management that is age-appropriate and supportive infrastructure for the transition of care from childhood to adulthood [12,13]. In Tanzania, prevalence of T1DM among children and youth ranges between 10.1/100,000 to 11.9/100,000 regionally [14] and a survival rate of between less than 6 months to 6 years [15].
In the early 2000s, the Ministry of Health (MoH) in Tanzania established designated pediatric and youth clinics for the two conditions in referral and regional hospitals and later rolled out to reach the lower health facilities.
The HIV clinics was started in the year 2004 and rolled out throughout the country at the peak of the pandemic through year 2010 when the care and treatment services were fully established. The diabetes clinic designated for children were started in the year 2005 and expanded throughout the country to reach 39 clinics that were fully established by year 2020. These efforts had shown to reduce mortality and morbidity [16,17]. On the other hand, the HIV infection transmission rate decreased and stabilized, since the start of Highly Active Antiretroviral Therapy (HAART) in the 2005 (39, 40) hence reduction of mortality on these conditions [18,19]. There have been improvement in care in both conditions [19,20] however, there has never been any comparative study on mortality to see how these conditions are faring in that respect.
Understanding mortality in both conditions will help to inform the allocation of resources and provision of care; and will also provide lessons for care for the benefit of both conditions. Therefore, this study aims at assessing the mortality of CYLDM in comparison with CYLHIV mortality in Tanzania.
This is a retrospective study of CYLDM and CYLHIV.
Study populationThe target population was all CYLDM and CYLHIV aged 0-25 years at diagnosis recorded in the available registries between 2004 to 2019 and given insulin or HAART, respectively depending on the condition.
Data collection for CYLDM: Methods for data collection for diabetes mellitus has been described elsewhere [21]. Figure 1 procedure for data collection for CYLDM.
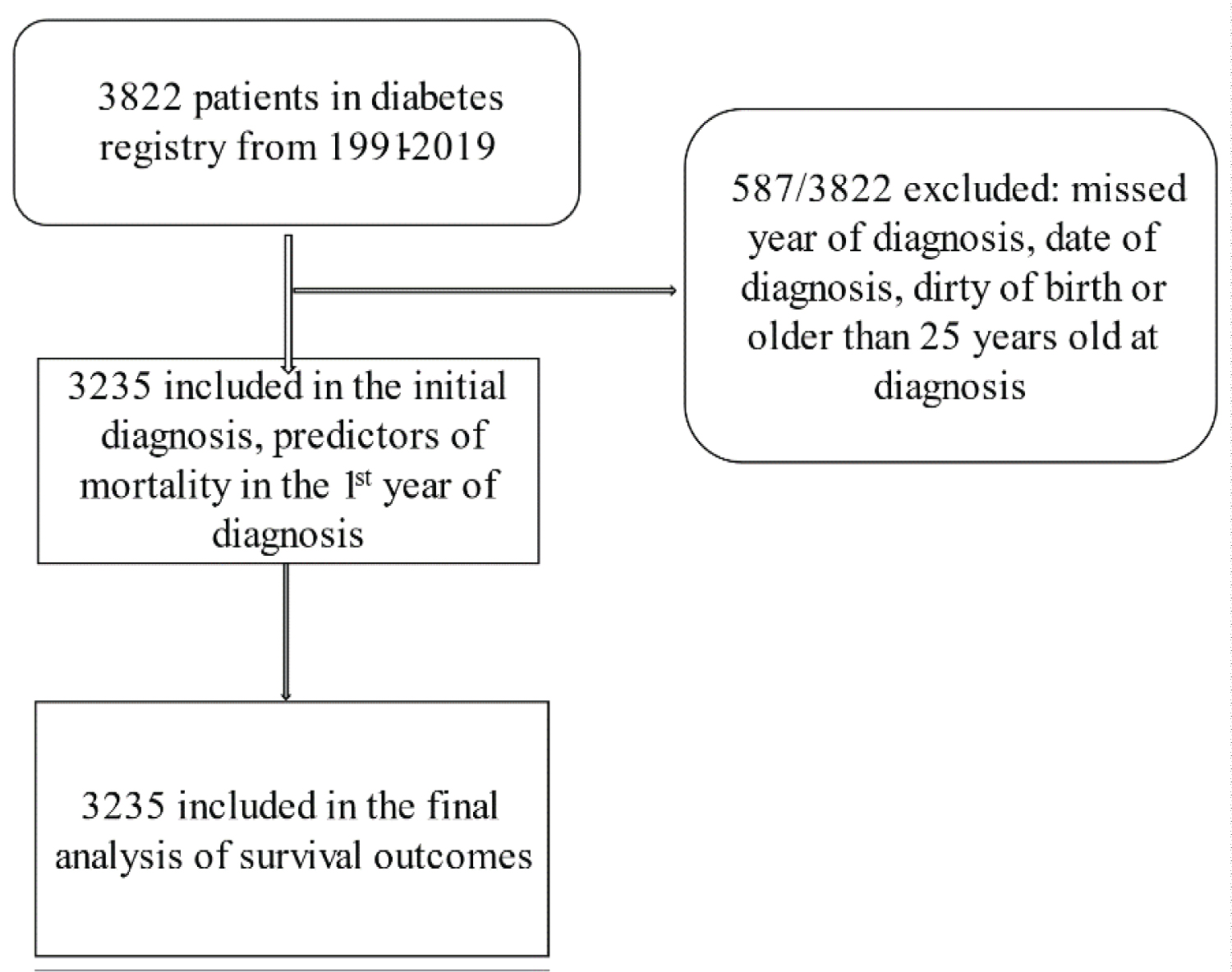 Figure 1: Screening and enrollment flowchart for Children and Youth Living with Diabetes Mellitus.
View Figure 1
Figure 1: Screening and enrollment flowchart for Children and Youth Living with Diabetes Mellitus.
View Figure 1
Data collection for CYLHIV: A retrospective data collection from the Care and Treatment database -(CTC-3Macro) stored electronically at the National AIDS Control Programme (NACP) server was done. This data base was initially created as a case-based surveillance system and recorded monthly and has been improving as the user demand arises. The data was extracted since the beginning of the record which was 2004 up to 2019. Only data common to both groups (HIV and Diabetes) were extracted; this included, date of birth, sex, date of diagnosis, clinic attendance, frequency of attendance, lost to follow up, death, date of death and age at death. Some of the excluded data were type of medications, opportunistic infections, any admissions, because they were missing in the diabetes registry.
Available demographic statistics were determined as of Jan 2004-Dec 31st Dec 2019. Screening process for CYLHIV is shown in Figure 2.
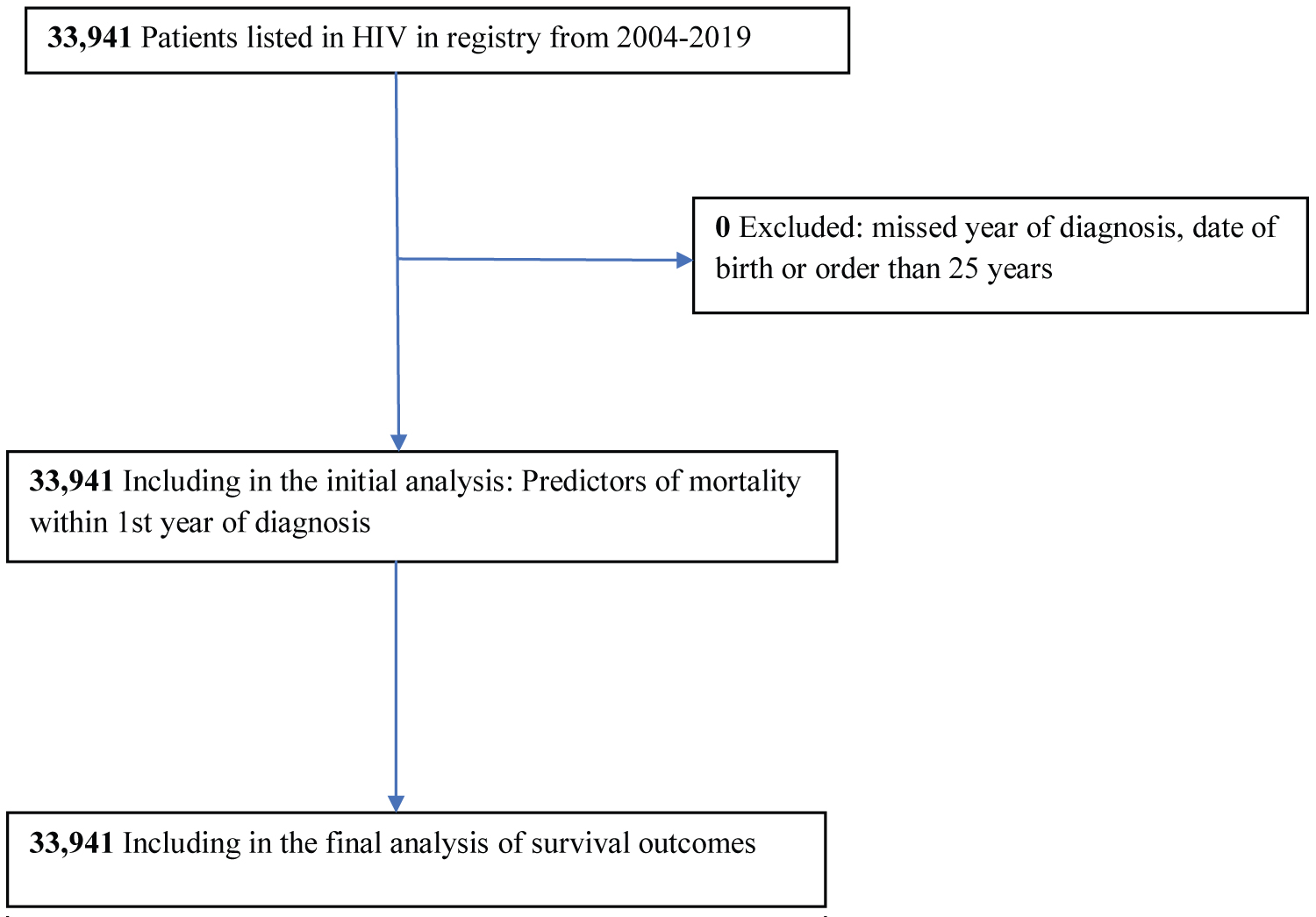 Figure 2: Screening and enrollment flowchart for Children and Youth Living with HIV infection.
View Figure 2
Figure 2: Screening and enrollment flowchart for Children and Youth Living with HIV infection.
View Figure 2
For analysis data was divided into three cohort: i.e. < 2005, 2006-2010 and 2011-2019, indicating the period before clinics (< 2005), during implementation process of the clinics (2006-2010) and rolling out throughout the country (2011-2019). Descriptive statistics, frequency, percentage, mean, median and interquartile range (IQR) were used to summarize different variables. Logistic regression was used to identify factors associated with death. Data analysis was entirely done in STATA-version 14.
The Ethical clearance to conduct this study was given by The Kilimanjaro Christian Medical University College Institution Review Board with certificate number 2478 and permission to use data was given by the Tanzania diabetes Association (TDA) and National AIDS Control Programme (NACP).
Data of 3822 CYLDM were recruited in the study, 3235 (83.1%) analyzed of which 1644 (50.8%) were male. Approximately seventy-two percent (72.2%) were diagnosed in the last cohort (2011-2019) and aged above 14-years-old. The Median (IQR) duration of living with diabetes was 5 (2-8) years and the mean age at diagnosis was 13.8 years (5.7) (Table 1). Observation time ranged from less than one year to 15 years.
Table 1: Demographic characteristics of CYLT1DM and CYLHIV: Tanzania (2004-2019). View Table 1
The overall mortality rate for those who died after the first year of diagnosis was 6 per 1000 person-years (95%CI = 5-7). Females had a higher mortality rate 7.2 (95%CI 5.6-9.3) than male 4.4 (95%CI 3.1-6.1), (Table 2).
Table 2: Mortality rates of children and youth with type 1 diabetes in Tanzania (1991-2019). View Table 2
Table 3 shows results from regression models. Gender were significantly associated with deaths in the logistic multivariable model. Males had lesser risk of dying (OR = 0.43; 95%CI = 0.20-0.93) within the 1st year of diagnosis when controlling for age at onset and diagnosis cohort. However, after the 1st year of diagnosis male gender is at higher risk of mortality 1.7 (95%CI 1.13-1.92).
Table 3: Factors associated with deaths CYLHIV and CYLDM within the 1st year of diagnosis in Tanzania (1991-2019). View Table 3
Data of 33941 CYLHIV were recruited in the study, all of the data (100%) were analyzed of which 12004 (50.8%) were male. Fifty-four percent (54.1%) were diagnosed in the last cohort (2011-2019) and majority aged more than 14 years. The Median (IQR) duration of living with HIV was 4.7 (4, 7) years (Table 1). The mean age at diagnosis was 13 years (8.3). Observation time ranged from less than one year to 15 years.
Eleven percent (11%) died within the observation period. The overall mortality rate for those who died after the first year of diagnosis was 14.7 per 1000 person-years (95%CI = 14.1-15.3). Males had a higher mortality rate 16.7 (95%CI 15.7-17.8) and the rates increased with increasing age of diagnosis (Table 3). The mortality rate was high during the roll out period 2005-2010 (16.1/1000 person years (15.3-17) and low in the last cohort 2011-2019 (139) (95% CI 12.1-14.0).
In Table 3 shows results from regression models. Gender was significantly associated with deaths in the logistic multivariable model. Males had higher risk of dying (OR = 1.31 95%CI = 1.12-1.54) when controlling for age at onset and diagnosis cohort within the 1st year of diagnosis. However, after the 1st year of diagnosis male gender was protective to death 0.73 (95%CI 0.66-0.88) (Table 3).
The flow charts: The overall number of children and youth was more in the HIV group than in diabetes. HIV had more complete data as compared to diabetes, as a result about 587 CYLDM were excluded due to missed date of birth or diagnosis (Figure 1 and Figure 2).
Demographic characteristics: There were more males in the diabetes group male to female ratio was 1.03:1, as compared to the HIV group where there was a female preponderance (Male to female ratio of 1.8:1). In both groups, the mean age of diagnosis was about 14 years with more people diagnosed in the 2011-2019 cohort. The majority of diagnoses were done in the urban area 82% and 74% for diabetes and HIV, respectively, with rural having 17.4% and 26.1% for diabetes and HIV, respectively (Table 1).
Status of CYLDM and CYLHIV: Table 2 shows how many children and youth were alive, dead, or lost to follow up. At the end of 2019, 62.4% and 45.3% of CYLDM and CYLHIV, respectively were alive. There was a loss to follow up of 37.7% for CYLDM, and 45.3% for CYLHIV.
Mortality data for diabetes has been described elsewhere [21] CYLHIV had a mortality rate of 3718 (11.0%). The mortality rate in the first year of diagnosis for CYLDM was twice in female 7.2/1000 persons years (5.6-9.3), as compared to males (4.4/1000 person-years (95% CI 3.1-6.1), whereas in CYLHIV males had higher mortality of 16.7/1000 person-years (95% CI 3.1-6.1) as compared to females 13.5 (12.8-14.2). Overall Mortality after the first year of diagnosis was higher among CYLHIV at 14.7(14.1-15)/1000-person years, as compared to CYLDM 5.8(4.7-7.4)/1000 person-years (Table 2). The mortality rate was higher for those diagnosed above 14 years of age, at 6.5/1000 person-years (95%CI 4.8-8.9) and 15.7/1000 person-years (95% CI 14.7-16.9) for diabetes and HIV, respectively. CYLHIV die slightly younger (mean age 16.6 (8.9)) than CYLDM (mean age 17.7(4.7)) (Table- Appendix File). Gender was one of the factors associated with mortality, female had higher mortality in CYLHIV, while in CYLDM males had high mortality. Also being diagnosed at the age above 14 years was a protective factor for mortality in both conditions (Table 3). The HIV mortality was 11% at 10 years and diabetes mortality was about 6% at 10 years.
In this study, we have analyzed data for the cohort of CYLDM and the cohort CYLHIV comparing mortality between the two groups.
There has been increase in diagnosis after the establishment of the clinics especially the cohort immediately after implementation (2011-2019) in both HIV and diabetes. This tremendous increase in diagnosis between 2010-and 2019 for both conditions has gone hand in hand with a reduction in mortality showing the improvement of medical care and provision of free medicine as well as awareness and access to the services. Also, stabilization of programs to roll out to more regions covering larger areas has moved services closer hence more and early access to care.
For both conditions, there have been higher losses to follow-up as compared to other parts of sub-Saharan Africa [22] for HIV patients. However, in the case of diabetes, the loss to follow up was comparable with other studies [23]. The loss to follow-up observed in our cohort is 10% more in HIV (43.7%) than in diabetes (33.7%). The loss to follow-up for children and youth with HIV in some studies is between 16-36% [11,23,24], whereas, in our study, this was observed to be high. This might be related to self-transfer to other clinics without previous information or death which created failure to attend to clinics. The high number of clients to health care providers, hence youth giving up on long queues. Nevertheless, it remains unknown the true outcome of loss to follow up which might be either unknown to the clinics or not recorded in the registry. This might underestimate the true mortality rate.
It has also been shown that most children and youth are dying within the first year of diagnosis in both conditions, the observation that has been shown in other studies due to delay in diagnosis and severity of the disease in diabetes [11], and HIV [24]. Also, delay in diagnosis for both Diabetes [25] and HIV.
Incidentally our findings also have shown that survival increases are inversely proportional to the age of diagnosis for both conditions. These were comparable to CYLDM in Rwanda [26], Mozambique, Zambia [15], and in developed countries [25,27]. This pattern has been observed in HIV as well where mortality was higher for those diagnosed above 14 years of age. Possibly early diagnosis helps to manage a patient better and reach a better metabolic control/viral suppression before they start getting complications, hence delay of complications and reduction in mortality. The second cause of increased mortality in this age group might be the fact that adolescents/youth is the period of autonomy and responsibility, critical physical, physiological, and emotional changes, coupling with peer pressure and transition to adulthood while the knowledge is not at the maximum [28], hence have a high risk of complications for those with diabetes and high rate of infection. Also, they are not yet ready to take full responsibility hence an imbalance between what they know and the responsibility they need to take.
This study has shown that children and youth aged between 15 and 21 years, had high mortality in all the three cohorts. Age at diagnosis showed that early diagnosis delays time to death, probably because at that time the care is in the parents' hands and the initial stage of care managed to achieve better control during this phase of the disease. As shown in the Diabetes Control and Complication Trial (DCCT), earlier control confers protection/delay in complications [29], hence delay in time to death. The same pattern is being observed in HIV infection as well where adolescents and youth are disproportionately affected [30] and the death rate is high [31]. Children below 10 years were less likely to die especially in the 2010-2019 cohort, an observation similar to a study done by Gisela, et al. in diabetes and Judd A, et al. in HIV [32,33].
With availability of separate pediatric and youth clinics, there is more awareness and access hence less misdiagnosis and better management with better control until they enter early adulthood. This conquers with the study done by Marshal, et al. in Pittsburg, where the life expectancy of type 1 diabetes had improved and there was no death in young children with type 1 diabetes [27]. A finding which is comparable to HIV infection, after the rollout of antiretroviral treatment, the number of deaths has decreased and the diagnosis has become earlier [34]. Again, with the advance in technology HIV incidence has decreased except for the youth [31] which might be another factor contributing the observed deaths in this age group.
This study was able to compare the largest cohorts of CYLDM and CYLHIV in Tanzania that have been followed up for about 30 years. The analysis has included children and youth recorded since the beginning of registries, which allows for the different cohorts, from misdiagnosis to diagnosis, no treatment, to insulin/antiretroviral for survival to insulin/ARTs for better care. The two cohorts have faced unawareness in both public and health care providers, about diabetes/HIV in children and youth to care policies for both conditions in Africa, hence a better perspective of the cohorts.
There are many subjects lost to follow-up, in which case we could not account for: We counted them as a live outcome, however, if they were counted as part of death, mortality would have been very high.
Incomplete data and missing information are the main limitations of this study as well as the fact that this data was solely hospital-based, hence data on children who never got diagnosed or never reached the health system might have died undiagnosed or were diagnosed but the programs missed them and hence missed in the registry which might have interfered with the percentage of overall mortality and might not give a true picture of mortality on the ground.
Unfortunately, in our setting the cause of death was not shown in the registers and the possibility of tying it to the death certificate was even more challenging.
The estimated death rate was high in CYLHIV compared to CYLDM. Both conditions had a similar duration of the condition and high rate of loss to follow up. This study serves as the basis for prospective studies to determine the causes and possible solutions against the high mortality and loss to follow up.
Further, the study findings could inform policy actions in health sector as appropriate.
The Ethical approval to conduct this study was given by the Kilimanjaro Christian Medical University College Institution Review Board with certificate number 2478.
There was no consent needed since there were de-identified registry data.
Not Applicable.
The study did not have any material to work with however all raw data generated in this study is available from the authors due to limitation in ethical issues.
The authors have no competing interests that might be perceived to influence the results and/or discussion reported in this paper.
There was no external funding for these studies except that there was a sort of in-kind contribution by authors and other people assisted to the conduct of this study.
Edna S Majaliwa, Proposal development, design, data collection, analysis, presentations, manuscript writing and critically reviewing the manuscripts. Prof. Blandina T Mmbaga, Proposal development, design, analysis manuscript writing and critically reviewing the manuscripts, Prof Kaushik Ramaiya, Proposal development, design, manuscript writing and critically reviewing the manuscripts. Prof. Sayoki Mfinanga, proposal development, study design and critically reviewing the manuscript, Mr. Joel Ndayongeje conceptualization of study designs, and review formal data analysis and interpretation of data, formatting, editing and critically reviewing the manuscripts.
Prof Jaffer Shabbar for reading through the draft, Miss Mary Mosha for the help with data from the Tanzania Diabetes Association (TDA) head office, Professor Andrew Swai, who continuously cleans the data at the Tanzania Diabetes Association- head office, Drs Martha Mkony, Kandi Catherine Muze, Namala Mkopi, and Valentina Chiavaroli for their comments and time to read through the draft, Benjamin Kamala for starting the analysis of these data. Patients and parents whose children's data have been used in this study.