The incidence of Type 2 diabetes is growing among adults in the Dominican Republic (DR), with little data regarding diabetes among youth. Our primary objectives were to describe the demographic and clinical characteristics of pediatric diabetes patients in the DR.
We conducted a retrospective chart review of 874 pediatric diabetes patients from 2000-2016. Data were abstracted and analyzed using SAS.
The number of pediatric patients seen in the diabetes clinic grew over the study period, with an increasing proportion with Type 2 (0-35%). A majority of our population was female (56%), with a median age of 11.7 years, and diagnosed with Type 1 diabetes (80%). Patients with Type 1 were younger (10 vs. 13, p < 0.0001), male (46% vs. 34%, p = 0.0045), and more often hospitalized (43% vs. 21%, p < 0.0001). Patients with Type 2 were more likely to have a first-degree relative with diabetes (14% vs. 50%, p < 0.0001). Nearly half of patients were overweight or obese; this proportion was higher for those with Type 2 (37% vs. 74%, p < 0.0001).
Pediatric patients with Type 2 diabetes are proportionally increasing in the DR. The study findings can inform policies, programs, and future research on diabetes among youth globally.
Adolescent, Child, Diabetes mellitus type 1, Diabetes mellitus type 2, Dominican Republic
DR: Dominican Republic; SACA: South and Central America Region; INDEN: Instituto Nacional de Diabetes, Endocrinologia y Nutricion; BMI: Body Mass Index; HDL: High-Density Lipoprotein; LDL: Low-Density Lipoprotein; Anti-GAD: Antibodies to Glutamic Acid Decarboxylase; Anti-ICA: Antibodies Islet Cell Antibodies; UNIBE: Universidad Iberoamericana; LAC: Latin America and the Caribbean
While the prevalence of Type 1 and Type 2 diabetes is growing globally, growth is especially prominent in the Caribbean region and other developing middle-income countries [1]. Data from the International Diabetes Federation reports the prevalence of diabetes has climbed to 8.5% in the South and Central America region (SACA); this estimate does not include the large numbers who are undiagnosed [2].
The age-adjusted prevalence of diabetes in the Dominican Republic (DR), which is part of the SACA region, reached 8.6% in 2019 and is expected to grow to 10.2% by 2045 [3]. The increase in prevalence of Type 2 diabetes in the DR, which doubled between 1999 and 2010, is an important contributing factor to the overall increase [4]. A comprehensive study in 2017 reported that, including those that are undiagnosed, the prevalence of diabetes in the DR is closer to 13.45% [5]. This finding is consistent with recent data that confirms over 50% of those with diabetes globally remain unaware [6]. Diabetes accounts for 4% of total deaths among the Dominican population [7]. The cost of treating one person with diabetes in Latin America and the Caribbean in 2015 was predicted to be between $1088 and $1818 per person, higher than the per capita National Health expenditure in that region [8].
Research on Type 2 diabetes has historically focused on populations 18 and older because the disease was seen primarily in adults [7]. However, studies now show that Type 2 diabetes is increasing among children and is often undiagnosed [6,9]. The American Health Association found that in the United States between 2001 and 2009, Type 2 diabetes increased over 30% for all sexes and age groups [10]. While some existing research focuses on diabetes in adults in the DR, little is known about diabetes among youth. A preliminary study showed that diabetes impacts at least 1% of persons under 18 in the DR [5].
Type 2 diabetes has similar effects for children as for adults through insulin resistance and pancreatic β-cell failure, however youth face increased risk for rapid β-cell decline and other future complications [11]. A lack of recognition and knowledge of childhood diabetes may lead to poor maintenance and outcomes [12]. Inpatient hospitalizations, emergency visits, ketoacidosis episodes, and diabetes-related complications increase the costs associated with diabetes [2].
We studied the demographic and clinical characteristics of pediatric diabetes patients over a period of 16 years in the DR, in order to compare Type 1 and Type 2 diabetes and identify changes in the patient population over time.
We conducted a retrospective medical chart review at the Instituto Nacional de Diabetes, Endocrinologia y Nutricion (INDEN) pediatric clinic. INDEN is located in Santo Domingo and serves the entire population of the Dominican Republic. The study population included all patients ages 0-17 seen at the INDEN pediatric clinic between January 1, 2000 and December 31, 2016. We included charts for patients with Type 1 diabetes or Type 2 diabetes, as identified by INDEN pediatric nurses. We did not include patients with other forms of metabolic syndrome.
We abstracted data from each medical chart using a form modified from a similar study conducted on diabetes in the adult diabetes clinic at INDEN [13]. The first 74 charts were used to pilot test our data collection process. We modified the form to more accurately reflect information available in pediatric charts, and based on the feedback of the Hospital Director. We translated medical chart notes from Spanish into English for the abstraction forms. All data were recorded on paper forms and then each form entered into Microsoft Excel.
We collected data for demographic characteristics, including age at diagnosis, sex, residence, and family history of diabetes; clinical characteristics, including body mass index (BMI), duration of diabetes, average annual visit frequency, hospitalizations, hypoglycemic episodes, ketoacidosis episodes, loss to follow up, and presence of self-monitoring; laboratory results for HbA1c, cholesterol, triglycerides, HDL, LDL, c-peptide, anti-GAD, and anti-ICA; and treatment modality.
We generated descriptive statistics for each variable. Variables were then compared by type of diabetes using the Wilcoxon Rank Sum test with independent samples for continuous variables and Pearson's chi-squared test for categorical variables. We used Fischer's Exact Test for categorical variables with small cell sizes (5 or less). P-values less than 0.05 were considered statistically significant. All statistical tests were run using SAS 9.4 software.
We received University of Virginia Institutional Review Board for Health Sciences Research (#19846) and Universidad Iberoamericana (UNIBE) ethics committee approval, and we were granted a waiver of informed consent. After data were abstracted from the INDEN pediatric medical charts, they were de-identified and entered into Microsoft Excel prior to analysis.
The number of new pediatric patients with diabetes at INDEN clinic varied from a low of 10 in 2001 to a high of 75 in 2012. In general, this number appeared to increase over the 16-year-period; between 2000 and 2016, the number of new patients more than tripled. Likewise, the proportion of new patients with Type 2 diabetes appeared to increase, from 0% in 2000 to 35.48% in 2016, the year with the highest proportion (Figure 1). In two other years (2006 and 2015), the proportion of patients with Type 2 diabetes reached approximately 30%.
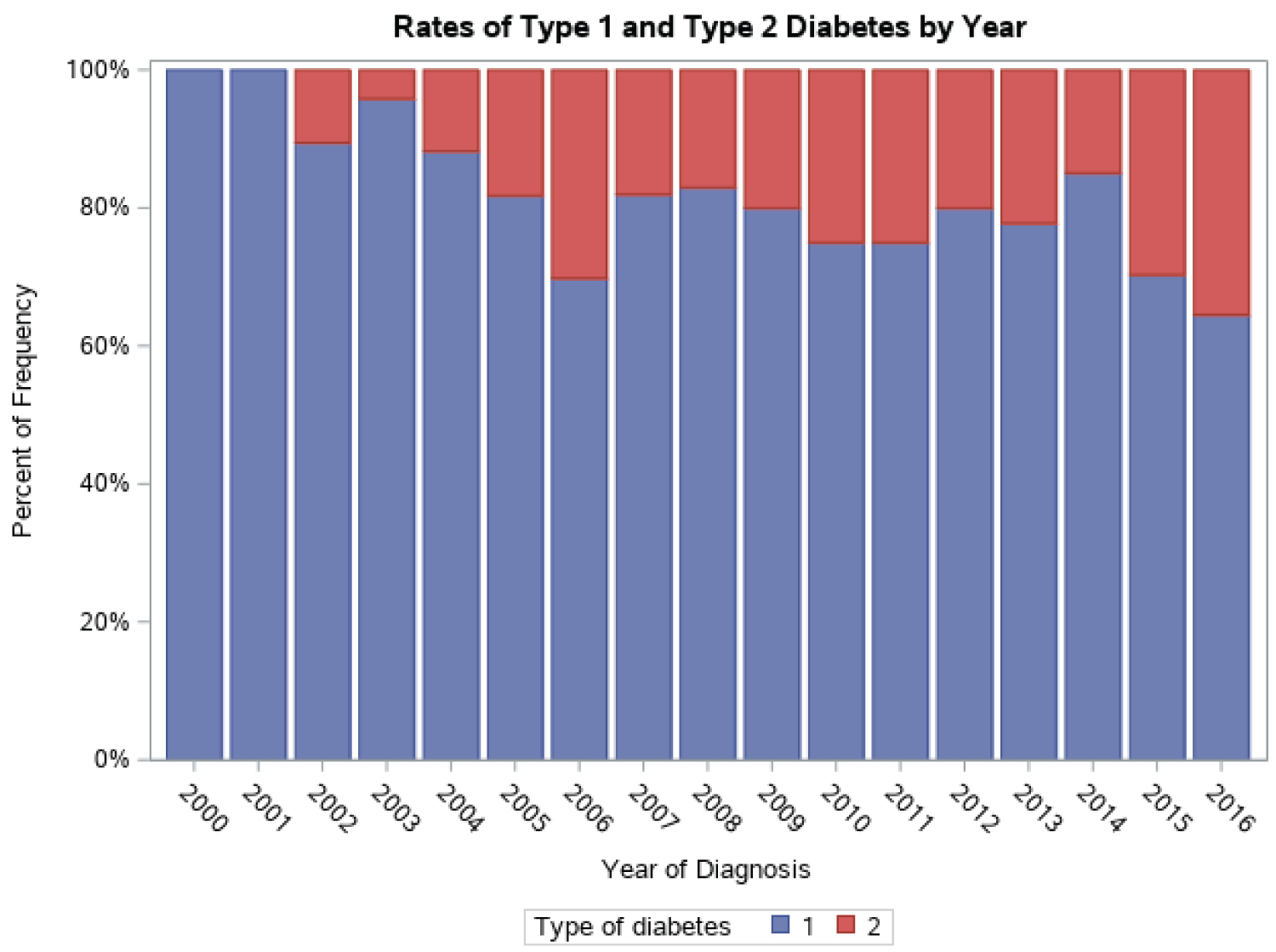 Figure 1: Rates of Type 1 and Type 2 Diabetes by Year.
View Figure 1
Figure 1: Rates of Type 1 and Type 2 Diabetes by Year.
View Figure 1
Table 1: Demographic and clinical characteristics of Type 1 vs. Type 2 patients at admission to INDEN's pediatric clinic between 2000 and 2016.† View Table 1
A description of the study population is provided in Table 1. The study population included 874 patients, the majority of which were female (56%) with a median age of 11.66 years (μ = 10.95) at presentation to the clinic. Data on race and ethnicity were not available.
A large majority of the patient population (79.63%) were diagnosed with Type 1 diabetes, while the minority (20.37%) had Type 2 diabetes. Patients with Type 1 diabetes were on average younger (10.43 vs. 13.27, p < 0.0001), and more often male (p = 0.0045). A majority of the patients (56.82%) were from the Santo Domingo province, however there was a relatively even distribution of patients among the other 30 provinces in the Dominican Republic (data not shown). One-fifth of all patients (21.29%) had a first degree relative with diabetes, while nearly one-half (46.49%) had at least one grandparent with diabetes. Compared to patients with Type 1 diabetes, patients with Type 2 diabetes were significantly more likely to have a first (13.89% vs. 50.00%) or second degree relative (43.27% vs. 58.99%) with diabetes (p < 0.0001).
Clinical characteristics of the study population are also shown in Table 1. While a majority of the patient population (53.92%) were normal or underweight according to WHO guidelines, nearly half (46.08%) were either overweight or obese. Of those with Type 2 diabetes, significantly more had a BMI classified as overweight or obese than those with Type 1 diabetes (73.68% vs. 36.94%, p < 0.0001).
Patients diagnosed with Type 1 had a significantly longer duration of diabetes and average annual visit frequency than those with Type 2 (3.43 vs. 2.07, p = 0.0003; 3.14 vs. 3.30, p = 0.0051). Forty-three percent with Type 1 were hospitalized while only 21% of those with Type 2 were hospitalized while patients at INDEN. Patients with Type 1 diabetes were significantly more likely to experience two or more episodes of hospitalization, hypoglycemia, or ketoacidosis (6.53% vs. 2.34%, p = 0.0348). Nearly two-thirds of patients (64.15%) were lost to follow up before their 18th birthday. Despite instructions given by the care provider, only one-third of patients (37.16%) monitored their blood levels or brought in self-monitoring records. Data on comorbidities in the medical charts were incomplete, however common comorbidities included asthma (4.12%) and thyroid disease (5.72%).
Treatment regimens varied based on diagnoses (Table 2). The same proportion of patients with Type 1 and Type 2 were prescribed long-acting insulin (19.38% vs. 18.02%, p = NS). However, patients with Type 1 were more likely to receive long-acting insulin with peri-prandial short acting insulin (79.73% vs. 33.72%, p < 0.0001), while Type 2 patients accounted for nearly all of oral hypoglycemics (0.30% vs. 25.00%, p < 0.0001) and combination regimens (0.59% vs. 23.26%, p < 0.0001). A majority of patients (68.27%) changed their medication while at INDEN, and more than 60% of patients were referred by their doctor to dietary modification and/or exercise.
Table 2: Treatment modality by type of diabetes at most recent visit to INDEN's pediatric clinic.† View Table 2
Our chart review is the first demographic and clinical investigation into diabetes among youth in the Dominican Republic and remains one of the few descriptive studies on youth diabetes to date. The purpose of this study was to better understand the underlying characteristics of youth with diabetes and the growth of Type 2 in the Dominican Republic and globally. The findings of this study can be used to inform future investigations of youth with diabetes, especially in the Latin America and the Caribbean (LAC) region, and provide demographic and clinical data to design and implement intervention strategies to reduce diabetes in this and other populations.
While information is limited on Type 1 versus Type 2 diabetes among pediatric populations, Type 1 remains the most common among youth [14]. Previous studies have documented that 85-95% of young patients were diagnosed with Type 1, while 1.3-10.8% had Type 2 [15,16]. The wide range of frequencies is likely due to variations between geographic regions [15]. While 80% of our study population had Type 1 diabetes, we found a higher proportion (20%) of patients with Type 2 than previous studies. Past studies from a variety of geographic regions have found that Type 2 diabetes is on the rise in pediatric populations. A study from the United States found that the adjusted prevalence of Type 2 diabetes among youth increased by over 30% between 2001 and 2009 [10]. Our findings indicate that the rate of Type 2 diabetes in Dominican youth may be especially high and is likely increasing.
While data are limited, Type 2 diabetes in youth populations is more common in girls, and is more often diagnosed at an older age than Type 1 [15-17]. One study noted that girls have a 60% higher prevalence of Type 2 than boys [10]. While age at diagnosis was not available for our study, our Type 2 patient population was also more often female and had a higher mean age than those with Type 1 diabetes.
Family history is a major contributing factor to both Type 1 and Type 2 diabetes, however, we found that patients with Type 2 diabetes were significantly more likely to have a family history of diabetes than their Type 1 counterparts. A study on the epidemiology and pathophysiology of Type 2 diabetes in youth found that among children with Type 2 diabetes, more than 75% have a first- or second-degree relative with diabetes [18]. Research notes that Type 2 diabetes, especially, is a complex interaction of genetic and environmental factors that is not completely understood [19].
Lifestyle factors likely contribute to the high rate of Type 2 diabetes in Dominican youth, as countries in the SACA region continue to urbanize. Populations in this region already face higher rates of obesity due to loss of physical activity and an increase in high sugar, low fiber consumption that contribute to increasing rates of diabetes in the region [9]. We found that Dominican youth with Type 2 diabetes were more likely to be overweight or obese than their Type 1 counterparts. A study the United States found that the prevalence of obesity in youth (up to age 19) with Type 2 diabetes was nearly 80%, and the prevalence of overweight was over 10%; even those with Type 1 diabetes were more likely to be overweight than people of the same age without diabetes [20].
Current available treatments for Type 2 diabetes are limited to lifestyle modifications and two pharmaceutical drugs [11]. Pediatric patients with Type 2 diabetes often receive similar treatment to those with Type 1, however management of Type 2 requires more lifestyle changes [16]. While a majority of patients in our study switched treatment type, we do not have data indicating the reasons they were prescribed various treatments. The IDF reported that access to insulin in the SACA region is limited in many places, and the price of insulin is variable between countries [8,9]. For patients with Type 2 diabetes, one study discovered that just over 50% of study participants met their targets for attending 75% of lifestyle intervention meetings [21]. However, the same study noted that there was not a significant difference in glycemic control or BMI for patients who did reach their participation goals compared with those who did not. This study is among few randomized trials that address the use of lifestyle modification in diabetes management among youth, and all call for further research on its effectiveness as first-line therapy. Thus, change in treatment within our patient population could be a result of lack of access, affordability, or improvement in glycemic control or BMI.
Among the major reasons for hospitalization among Type 1 pediatric patients are diabetic ketoacidosis and hypoglycemia [22]. Although Type 1 patients experience episodes of ketoacidosis more often than their Type 2 counterparts, up to 40% of pediatric patients with Type 2 experience episodes of ketoacidosis [15]. While we were unable to collect data on patient compliance with treatment, previous research conducted in the SACA region documented that expected hospitalization rates were 3 times higher among those who do not follow their treatment regimen [9]. Further, hospitalizations in this region account for 50% of diabetes related costs. These findings suggest promoting better glycemic control will reduce high rates of hospitalization among our study population and lower associated costs.
The reported rate of patient self-monitoring was very low in our study, potentially due to a true lack of patient compliance, a lack of communication between provider and patient, or incomplete record keeping. However, studies show that management of diabetes is integral in delaying and minimizing future adverse outcomes; increasing self-monitoring practices is critical in such management, especially among youth [23]. Incorporating technology to facilitate more frequent monitoring has been suggested [24]; the possibility of increasing technology in diabetes management could be explored for Dominican youth and similar populations as cell phones and other technology have become more widespread.
We were limited in our ability to assess comorbidities. These were not frequent in either group of patients, however these patients are young and their risk of comorbidities will likely increase with age.
Our study has some limitations. The pediatric clinic at INDEN was the only department that had not switched over to Electronic Medical Records; thus we transcribed the data from paper records with less of a standardized method for recording data than an EMR. We observed variations in recording by healthcare provider; for example, one nurse (identified by handwriting) consistently recommend diet and exercise in her patient notes while others did not always note those recommendations. No data were available for income, and data were missing for some variables. Data were also not available for race and ethnicity. Finally, these data are from a chart review, thus we were unable to document rates of Type 1 or Type 2 diabetes in the Dominican population.
Our study also has multiple strengths. We abstracted all charts available between 2000 and 2016. Our data collection tool was piloted and modified appropriately for the pediatric charts. We were able to clarify questions about the data with the clinicians who had recorded the information. This study is the first to describe demographic and clinical characteristics of pediatric diabetes patients in the Dominican Republic.
We found an increase in the number of pediatric patients with diabetes, and an increased proportion with Type 2 diabetes, between 2000 and 2016. These findings point to the need for programs and policies to address this disease in this population, as well as for further research to expand our understanding of the contributing factors and the characteristics of those most at risk.
Among youth with Type 1 diabetes, management needs to be improved. Providing affordable access to medication and accessible procedures for monitoring glucose levels are two suggestions that could reduce adverse outcomes. In addition, more comprehensive programs should be considered. An analysis on interventions for young patients with Type 1 diabetes noted an increase in glycemic control for patients with additional emotional, family, or other social support compared to those with only a behavioral regimen [25].
Type 2 diabetes may be prevented and/or managed through lifestyle and behavior change. It is unclear, however, how much populations understand diabetes and diabetes management [12]. Increasing awareness and early detection within communities is a first step. A subcommittee of experts in the United States concluded that treating youth with Type 2 diabetes with medication was more effective in combination with immediate lifestyle change. The committee also noted that personalized plans considering each individual's cultural preferences and age were necessary in successful management [26]. Systematic reviews also conclude that a successful management plan for young patients with diabetes involves more than providing medication in isolation [26,27]. It is important to address this disease not only because of the added strain on health systems and increased medical costs, but also because Type 2 diabetes especially has been shown to have effects on emotions, focus, productivity, and quality of life among youth [28].
We would like to thank Dr. Marcos A. Nunez C. FICS, M.Ed., Dean of the School of Medicine of the Universidad Iberoamericana, for his leadership in establishing the Universidad Iberoamericana-University of Virginia research collaboration.
P.H., A.P. and A.I. conceptualized and designed the research study. J.D., J.C., N.S., O.E., and A.I. acquired the data. J.D., P.H. and A.P. analyzed and interpreted the data. J.D. and P.H. wrote the draft. J.D., P.H., A.P., J.C., N.S., O.E. and A.I. revised the paper.
J.D., P.H., A.P., J.C., N.S., O.E. and A.I. approved the final manuscript. J.D., P.H., A.P., J.C., N.S., O.E. and A.I. agree to be accountable for all aspects of the manuscript.
This work was supported by the University of Virginia's Center for Global Health.