Malaria is an important public health concern among pregnant women, approximately 32 million of them are at risk annually. According to the World Health Organization (WHO), malaria represents annually more than 10.000 maternal deaths and 200.000 neonatal deaths too. Intermittent Preventive Treatment (IPT) is used to reduce disease in pregnancy and their effects on the newborn. Today the WHO recommends that at least three doses of IPT should be taken by pregnant women during Antenatal Care Visit (ANC), this should be taken every month from the sixteenth week of pregnancy till parturition. This study aimed to assess the effect of IPT on the birth weight of the babies of mothers delivering in Dschang District Hospital.
The study was conducted at the maternity unit of Dschang District Hospital located in Dschang (west region of Cameroon). In order to achieve this, a total of 380 participants, constituted essentially of women coming for delivery in the hospital were necessary. Data on the number of ANC, total dose of IPT taken have been taken from their health books. Moreover, information on socio demographic characteristics and obstetrics history of each participant were also recorded through an interview. Furthermore, blood was collected from the maternal side of placenta into EDTA tubes for assessment of maternal anemia. After all these, birth outcomes were then recorded.
At the end of this study we found that 98.7% of participant had made at least one ANC while 65% of them had taken at least three doses of IPT. The uptakes of IPT vary according to the number of ANC (P < 0.05). Furthermore, it appeared that 13.9% of new born had low birth weight, although the prevalence of malaria during pregnancy was (25.3%) and maternal anemia (24.5%) were important. majority of pregnant women were those aged between 24-34 years-old (59.2%) and having secondary level of education (58.8%).
Although the majority of women took more than 3 doses of IPT, after delivery the prevalence of anemia and Low birth weight was 24 and 13 percent. Otherwise, studies are needed to assess the real efficacy of IPT in preventing malaria during pregnancy and the causes of maternal anemia.
ANC: Antenatal Consultation; BW: Babies Weight; Df: Degree of Freedom; IMN: Impregnated Mosquito Net; IPT: Intermittent Preventive Treatment; MIP: Malaria in Pregnancy; SP: Sulfadoxine Pyrimethamine; WHO: World Health Organization
Malaria is a disease caused by an intra-erythrocyte protozoan of the genus Plasmodium which infects the red blood cells of human [1]. These pathogens are transmitted from one person to another through the bites of infected female anopheles mosquitoes or transplacentally by mother to fetus during pregnancy [2].
Malaria is an important public health concern among pregnant women, where approximately 32 million of them are at risk [3]. Five species of this protozoan parasite belonging to the genus Plasmodium are responsible for disease in humans. They are Plasmodium ovale, P. vivax, P. malariae, P. knowlesi and P. falciparum which are not only the most virulent and widespread, but also the one responsible for most cases of disease and death recorded [4].
According to the World Health Organization (WHO), malaria represents more than 10.000 maternal deaths and over 200.000 of neonatal death annually [5]. Globally, it is estimated that more than 2.4 billion of humans, approximately half of the world population lives in areas where disease is found [6]. Sub-Saharan Africa records each year alone about 25 millions of infected pregnant women [7,8]. The prevalence of placental infection by P. falciparum among pregnant women is estimated between 5 to 52% in these tropical countries [9].
Among pregnant women living in stable malaria transmission areas, little (few) infection lead to symptomatic malaria. However, they are related to maternal morbidity such as anemia and adverse effects on the child as abortion, low birth weight and child mortality [10]. In low transmission areas of malaria where women relating to age of procreate have no acquired immunity in malaria, malaria in these pregnant women is related to anemia, an increase in the risk of having serious malaria and can lead to voluntary abortion, mortality and low birth weight of babies at delivery [11]. In high areas of transmission, malaria is more present in primiparous the prevalence and the parasitic density decrease with the number of pregnancies [12].
The diagnostic of this parasitosis passed throught microscopic examination, detection of specific nucleic acid by Polymerase Chain Reaction (PCR) and the detection of plasmodium antigens by Rapid Diagnostic Test using specific kits.
Today, intermittent Preventive treatment (IPT) with Sulfadoxine Pyrimethamine (SP) is highly indicated as treatment of simple malaria among pregnant women and children less than five-years-old in malarious areas in Africa [11]. That is why the WHO recommends at least three doses of IPT of malaria for each pregnant women regardless plasmodial infection [13], this because the treatment was found to be efficient against maternal anemia and low birth weight of newborn [11-14].
The study was approved by the Institutional Review Board of the Cameroon Baptist convention Health Board No: IRB2019-38, whereas administrative authorization was obtained from the West Regional Delegation of Public Health. Written informed consent was obtained from all the study participants.
The study was conducted at the maternity units in Dschang District Hospital (Figure 1) located in Dschang in West Region of Cameroon from January and December 2021. Dschang is the chief place of the Department of Menoua with five (5) Districts. He is located between 5°25'-5°30 of North latitude and 10°-10°5' East latitude located at 213 km North of Douala and 350 km North-West of Yaounde. This city is built on the Southern sides of the Bamboutos Mountains and opens in the southwest by the Menouet River flowing to the Mbo plain. At the East, it is closed by the Bani massif that culminates more than 1920 mm. the rainfall is 1900 mm per year for a temperature average of 20.2 °C. Dschang is between the altitude savannah and the mountain forest; the bottom funds are covered with very dense vegetation. The relief is very rough; the city is based on an old base forces volcanic training. The urban area occupied essentially a set of hills. The valleys are occupied by marigots and swampy grounds. The city is subject to the climate level altitude. It is the equatorial climate of Cameroon. Dschang District Hospital was selected for the study because of government-owned institutions that offer antenatal care, preventive, curative and delivery services at affordable costs and is highly accessible.
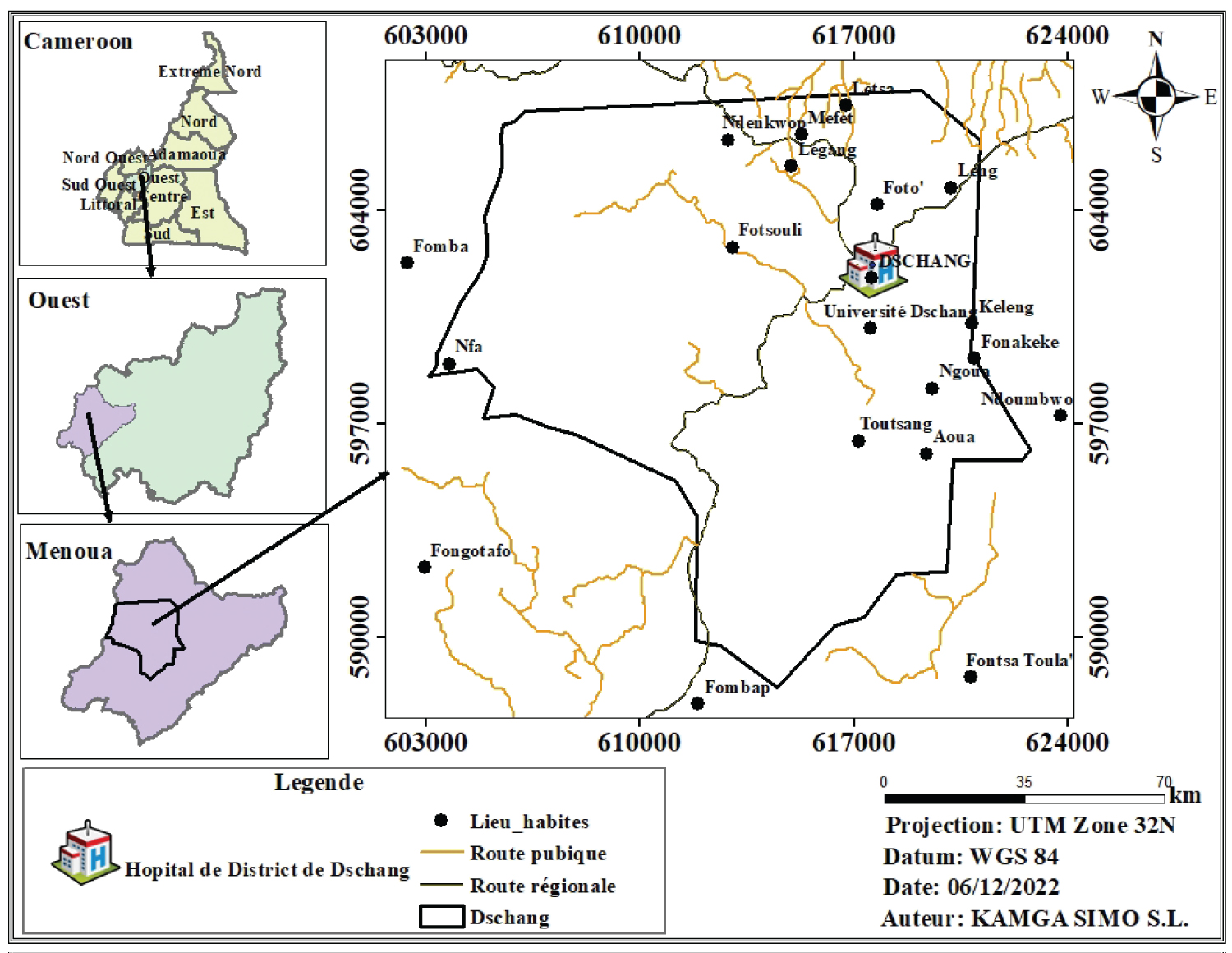 Figure 1: Study site.
View Figure 1
Figure 1: Study site.
View Figure 1
Consenting pregnant women were enrolled consecutively through a cross-sectional survey at delivery in the maternity. Enrolment by the time of delivery ensured uptake of adequate doses of IPTp-SP as stipulated by the World Health Organization (WHO). Mothers with evidence AIDS were not eligible for the study. An interview-guided administered questionnaire was used to obtain information relating to demographic data (age, residence) antenatal clinic data (gestational age, parity and number of antenatal care visits) and ITN usage. The use of IPTp and number of doses as well as new-born birth weights were documented and verified by checking ANC cards, patient's medical record book and health center maternal care register. Body temperature of the mother was measured using a digital thermometer to determine fever.
After delivery a placental blood sample was collected at the maternal side for haemoglobin (Hb) measurement in EDTA tubes. All samples were transported to the laboratory of the Dschang District Hospital. Haemoglobin concentration was determined using a haemoglobinometer (HemoCue) and strips. Maternal anemia was defined as a hemoglobin level of < 11 g/dL.
Data were recorded on the survey sheet and laboratory note book, then uploaded into Microsoft Excel 2010 Software and analyzed using R Software Version 4.1.4. The significance of differences in proportions were explored using the Pearson's Chi square test, whereas the differences in group means were assessed using Student t test, analysis of variance (ANOVA). Association analysis of number of SP doses, PM infection and LBW was undertaken by logistic regression. A P value < 0.05 was considered statistically significant.
A total of 380 pregnant women were enrolled at delivery among whom those aged between 24-34 years-old (Table 1) were the most represented (59.2%) while aged more than 34 years were the least (11.8%).
Table 1: Characteristics of study population. View Table 1
Moreover, pregnant women having the secondary level of education (56.3%) were the most encountered while those who had primary level of education (1.84%) were the least encountered. It also appeared that 54.2% of participants did not sleep under mosquito bed net while the duration of the majority using it was equal or greater than five months (53%). Furthermore, we observed that 37.9% of women were primigravide while 32.4% did not have children at home. The gestational age was normal for the majority of participants (95.8%).
Out of these pregnant women, the prevalence of Malaria in Pregnancy (MIP) was 25.3% with 24.5% of them presenting anemia, although severe anemia was recorded only in 0.53% of women. We also noted that 93.2% of pregnant women did at least three antenatal consultations (ANCs), while 4.47% of them did two and 1.05% did one. However, four pregnant women did not go for ANCs at all.
Among children born during this study, results revealed that a majority (86.1%) had a normal birth weight while
Some parameters studied could be associated to or not to the Intermittent Preventive Treatment (IPT) intake. Table 2 below summarizes the results dealing with the relationship between IPT doses and all characteristics of study population. According to this table, among the women who slept on mosquito bed net, only 45.12% took more than three (3) doses of IPT while in women who did not slept under, 53.18% of them have taken over three (3) doses of IPT. Speaking of the number of Antenatal Care visit (ANC) the IPT is associated (P < 0.05) to this parameter because the increase of the number of ANC is the increase of the number of dose of IPT taken. In the same order of idea among pregnant women who have taken more than three (3) doses of IPT, the most represented were primigravide. The majority of women who had taken more than three doses of IPT had a normal gestational age but also was saving from maternal anemia and had children with normal birth weight.
Table 2: Association of characteristics of study population and IPT. View Table 2
Anaemia was defined as haemoglobin concentration less than 11 g/dL (< 11 g/dL). The Table 3 below shows the relationship between haemoglobin levels and characteristics of the study population. It appears from this Table 3 that haemoglobin levels are not related to characteristics of the study population except for malaria in pregnancy (P < 0.05). With regard to the use of the mosquito bed net the proportion of women who did not use (52.98%) in term of anemia is higher than those who use (47.01) this parameter was not dependent on anemia (P = 0.8056). With regard to the gravity the multigravide present anemia more than the primigravide. Women who took less than three doses of IPT present anemia in contrary to those who took more than three doses of IPT.
Table 3: Relationship between anaemia and characteristic of the study population. View Table 3
Low birth weight (LBW) is defined as the weight of baby less than 2500g. It could be associated or not to characteristics of the study population. According to Table 4 below, low birth weight is associated with gestational age and duration of use of mosquito bed net (P > 0.05). concerning the use of mosquito bed net, the majority of women who had children with low birth weight are those who did not use mosquito bed net (52.83%) contrary to those who use it (47.16%). Multigravida had a high number of children with low birth weight (50.94%) who is higher than those of primigravide (37.73%). Women who took less than three doses of IPT are those who had a high number of children with low birth weight (67.92%) contrary to the proportion of those who took more than three doses of IPT (67.92%).
Table 4: Association between birth weight of babies and the characteristics of the study population. View Table 4
We carried out a survey in order to assess the effect of Intermittent Preventive Treatment (IPT) on the birth weight of newborns. Out of the 380 pregnant women participating in the survey, it appeared that 64.99 % of participants received at least three doses of Intermittent Preventive treatment (IPT). These results are higher than the 17.1%; 35.4%; 46.6% and 47.0% obtained by Feng G, et al. [15] in Malawi; Biaou COA, et al. [16] in Benin; Arnaldo P, et al. [17] in Chókwè District, Southern Mozambique and by Agyeman YN, et al. [18] in a study made in the Mount Cameroon and Kamissoko M [19] in Chókwè area respectively. This could by du to the fact that more the time passed more women are informed about the importance of IPT. These results show adherence and respect of recommendations by the World Health Organization (WHO) on the number of doses of IPT to be taken during pregnancy.
After delivery, anemia was found in 24.5% of women. This could be due to the fact that anemia is not always linked to plasmodial infection but can be due to other parasitosis such as helminthiasis.
The weight of the newborn was taken after delivery and, we noted that 13.9% of them had a low birth weight. This finding was higher than the 12.1%, 28%, 9.7% and 9.6% reported in Bamako by Toure OA, et al. [20], in Ivory Coast by Braun V, et al. [21], in Uganda by Ahmed R, et al. [22]. The decrease in rate of babies with low birth weight showed that women coming for antenatal consultation in Dschang District Hospital respected instructions by their physicians. These results are lower than the 37.1% obtained by Ahmed R, et al. [22] in Indian and 38.4% obtained by Zara MO, et al. [23] in Niamey (Niger).
Malaria in pregnancy was assessed and the prevalence was 25.3%, it was lower than the 65.6% obtained by Iwuchukwu IC, et al. [24] in Owerri, IMO State, Nigeria 29.5%, by Kamissoko M [19] in Bamako, but higher than the 7.9% and 19% reported in Ghana by Anto F, et al. [25] respectively. The high prevalence of malaria in pregnancy in Dschang could be due to the fact that since 2020, the campaign and distribution of Impregnated Mosquito Net (IMNs) had stopped. Furthermore, it is likely that the drug used for the IPT was not effective.
In this study primigravids accounted for 37.89% of the study population. These results are lower than 49.6% obtained by Manirakiza A, et al. [26] in Malawi, but are higher than 28.7% [19] in Bamako District Health 29.6% and 24% obtained by Toure OA, et al. [20] and Arnaldo P, et al. [17] in Ivory Coast and 26% by Manirakiza A, et al. [26] in Ghana. Eighty two point fifty seven percent (21.57%) of women were primiparous. These results are lower than those obtained by Manirakiza A, et al. [26] in Ghana and Biaou COA, et al. [16] who had obtained 33.1% and 38.2% of primiparous women respectively.
Concerning attendance at ANC, 93.2% of women made at least one ANCs. These results are similar to 93.3% and 95% obtained by Diengou NH, et al. [27] in Bangui (Central Africa Republic) and Kamissoko M [19] in Bamako (Mali). However, these results are higher than the 72.8%, 75.3%, and 72.68% obtained by Aminata F, et al. [8] in Bamako (Mali); Toure OA, et al. [20] in Ivory Coast and Biaou COA, et al. [16] in rural area (southern Benin). This would be due to the fact that Dschang is a rural area with a high level of education. Here women are sufficiently informed about the importance of ANC.
Less than half (45.8%) of these women did not sleep under mosquito nets. These results are less than the 81%, 77.3%, 97%, 85% obtained by Kamissoko M [19] in a study made in a rural area in Bamako (Mali); by Anto F, et al. [25] in Ghana and Anchang-Kimbi JK, et al. [28] in Bamenda Health District (Cameroon). This difference can be due to the low distribution of mosquito nets to pregnant women during Antenatal Consultation and the absence of mosquito net distribution campaigns. These results are higher than the 35.5% obtained by Dosoo DK, et al. [29] 2021 in Ghana.
The most represented group was those aged between 24-34 years. Results were comparable to those of Feng G, et al. [15] in Tanzania where they found that the most represented group were aged between 20-34 years and those of Mutanyi JA, et al. [30] in Sabatia (Kenya) where they found that the most represented were aged between 24-34 years. This observation suggest that, it is at this age that women acquire maturity and consequently could be responsible and even knowing what they done. However, the finding was different from earlier reports of Toure OA, et al. [20] in Ivory Coast where the most represented women were aged more than 30 years and those of Igboeli NU, et al. [31] in Nigeria (women aged between 18-34 years). The difference observed between all these studies could be due to how the grouping of participant according to their age was done by the author.
The majority of women (56.8%) participating in this study had a secondary level of education. The finding corroborates the 57.9% obtained in Bangui (CAR) Diengou NH, et al. [27] and those of Toure OA, et al. and Mutanyi JA, et al. [20,30] in Kenya. However, it was not in accordance with those of Feng G, et al. [15] in Tanzania and Anto F, et al. [25] in Ghana who rather found women with primary level of education and those not educated at all respectively. The high percentage of pregnant women in this study could be explained by the fact that Menoua Division generally has many government and private high school, higher institutions including a University and Training Colleges.
At the end of this study whose main objective was to assess the effect of Intermittent Preventive Treatment (IPT) on the birth weight of babies at delivery, it revealed a significant improvement in the uptake of ≥ 3 doses of IPT in Dschang with a coverage of 64.99%, Frequent visits to the ANC clinic, and type of health facility determined uptake of adequate doses of IPT. Although the majority of women took more than 3 doses of IPT, after delivery the prevalence of anemia and Low birth weight was 24 and 13 percent. Otherwise, studies are needed to assess the real efficacy of IPT in preventing malaria during pregnancy and the causes of maternal anemia.
KSSL wrote the first draft of the paper. All authors contributed to interpretation of data and revision of the Manuscript. All authors read and approved the final Manuscript.
We thank all the women who agreed to participate in this study. We are also grateful to the Director of the Dschang District Hospital for giving us space and a laboratory in which to work to the accomplishment of this work. Special thanks to all the midwife of the Maternity of Dschang District Hospital and Juluis Visnel FOYET F for the data analyses with R.
We don't have any potential conflicts of interest to disclose.
The datasets generated during the current study are available from the corresponding author on reasonable request.
Not applicable.
This study did not receive any funds but is a part of the parents of the student (personal funds).