Context and objective: Around 8% of incident cases of tuberculosis (TB) were reported among people living with HIV worldwide in 2022. Tuberculosis is the leading cause of death among people living with HIV. Africa accounts for the majority of co-infection episodes, with over 50% of cases in some parts of southern Africa. In the Democratic Republic of Congo (DRC), around 9% of persons living with HIV (PLHIV) develop TB and 11% of TB patients are infected with HIV. The DRC is one of the 30 countries in the world bearing the brunt of co-infection. Despite the efforts made by countries to improve access to antiretroviral traitement (ART), TB remains a major problem among people living with HIV. The Lingwala Health Zone in the provincial city of Kinshasa recorded a large number of cases of HIV/TB co-infection during the study period. The aim of this study was to determine the factors associated with HIV/TB co-infection among PLHIV on ART in the Lingwala health zone (HZ) in Kinshasa.
Methods: This was a case-control study conducted in the state-run HIV care facilities in the Lingwala health district among PLHIV who had visited the health facilities during the period 2021-2023. Cases were coinfected patients and controls were PLHIV who had not developed tuberculosis during the study period.
Results: A total of 281 PLHIV were enrolled in the study, with 70 cases and 211 controls. Factors associated with HIV/TB co-infection after multivariate analysis were viral load (OR = 5.34; 95% CI; 1.8-15.8, p = 0.005). History of tuberculosis (OR = 20.84; 95% CI; 8.6-50.3, p < 0.01). Duration of infection 5 to 9 years (OR = 13.65; 95%CI; 2.2-85.0, p = 0.005) and BMI < 18.5 kg/m2 (OR = 5.34; 95%CI; 1.8-15.82, p = 0.005).
Conclusion: The results of this study indicate that the detection of these enumerated factors should prompt providers to actively search for tuberculosis with a view to organising early management.
PLHIV on ART, HIV/TB co-infection, Viral load, antiretroviral (ARV) adherence
Tuberculosis is the leading cause of death among PLHIV, accounting for around a third of acquired immune deficiency syndromes (AIDS) related deaths worldwide. Globally, 8% of incident TB cases are reported among PLHIV, according to the Joint United Nations Programme on HIV/AIDS (UNAIDS) fact sheet for 2022 [1]. Tuberculosis-related mortality has risen sharply among PLHIV, with 187,000 deaths, more than 100,000 more than in 2020 [2].
Africa has the majority of episodes of co-infection, exceeding 50% of cases in some parts of southern Africa [1]. Forty per cent of deaths from tuberculosis associated with HIV infection occur in Africa [3].
The Democratic Republic of Congo is one of the 30 countries with the highest burden of tuberculosis, HIV/TB co-infection and multi-drug resistant tuberculosis (MDR-TB) in the world. Around 11% of patients who develop TB are HIV-infected, and more than 9% of PLHIV develop TB in the DRC. These statistics are provided in joint annual report of the National Tuberculosis Control Programme and the National AIDS Control Programme (NTCP-NACP). The NTCP reported 202129 new and relapsed cases of tuberculosis in 2020. In 2021, the programme reported 218,000 new and relapsed cases. This represents an increase of 7.8% on the previous year. Nearly 41,000 HIV-negative cases and 9,100 HIV-positive cases died in 2021 [4]. According to the NACP annual report for 2021, 7046 PLHIV were diagnosed with active tuberculosis, i.e. a detection rate of 32% with the HIV gateway, and 13169 tuberculosis patients diagnosed as HIV+, i.e. a detection rate of 8% with the tuberculosis gateway in 2021. Approximately 55640 PLHIV out of 71427 eligible PLHIV received isoniazid prophylaxis, i.e. 78% coverage [5]. The DRC, through the two programmes NACP and NTCP, has implemented two strategies, the one-stop shop and the differentiated models, in order to resolve the shortcomings relating to the performance indicators for the HIV and TB gateways [6].
Despite the burden of HIV/TB co-infection, very few studies have analysed the risk factors for TB among PLHIV on ART in the DRC. This study therefore analysed the factors associated with HIV/TB co-infection in the most affected health zone during the study period.
As part of the analysis of factors associated with HIV/TB co-infection, a case-control study was conducted in the Lingwala HZ in Kinshasa. The study took place between 11 February and 15 July 2023. The study involved PLHIV being followed up in the health facilities providing HIV care in the Lingwala HZ.
The study was carried out in the Lingwala Health Zone, one of 35 health zones in the Kinshasa Provincial Health Division (PHD). The Lingwala Health Zone is located in the administrative district of Lingwala, bounded to the east by Avenue des Huileries, which borders the Kinshasa HZ, to the west by Avenue de la Libération, which borders the Gombe and Kokolo HZ, to the north by Mont des Arts and Itaga avenues and to the south by Boulevard Triomphal, which borders the Kasa-Vubu HZ. The Lingwala HZ is made up of 8 Health Areas (HA): La Voix du peuple, Trente juin, Ngunda-lokombe, Lokole, CNECI, Wenze, Paka-Djuma and Singa-Mopepe. The population of the health zone at the time of the study was estimated at 120268, with an annual growth rate of 3%. The health zone comprises four state-run HIV treatment facilities and one private HIV treatment facility. The state facilities involved in the study were the Kabinda General Reference Hospital (KGRH), the Kalembelembe Hospital, and the Vijana and Kitega health centres (HC).
HIV/TB co-infection status as a dependent variable was considered to be any PLHIV diagnosed with TB either on the basis of biology or medical imaging, or on the basis of a physician decision and started on ART. The other variables have been used as independent variables.
Clinical stage: The World Health Organisation (WHO) clinical stages recorded in the patient registers at the first visit during the study period.
Viral load: The numerical value of the last result obtained by the patient before or at the first visit during the study period.
Tuberculosis preventive treatment (TPT): The notion of regular and complete use of preventive treatment, either a combination of isoniazid and rifapentine for three months (3HP regimen) or isoniazid for six months before the first visit during the study period.
Person with a history of smoking: Patient with a history of smoking prior to the first visit during the study period.
Patient with a history of alcohol use: Patient with a history of alcohol use prior to the first visit during the study period.
Patient's place of residence: The patient's place of residence in the health zone or outside the health zone during the study period.
Adherence to ART: Individuals with poor adherence if the score is < 6, and those with average adherence (score between 6 and 7) and good adherence (if the score is ≥ 8). These last two categories were considered in the present study as acceptable compliance. This was based on the Morisky Medication Adherence Scale [7].
Nutritional status: Underweight if body mass index (BMI) < 18.5 kg/m 2 , normal weight if BMI between 18.5 and 24.9 kg/m 2 , overweight if BMI between 25.0 and 29.9 kg/m 2 , obese if BMI ≥ 30 kg/m 2 [8].
Comorbidity: The presence of at least one of the following comorbidities: Diabetes mellitus, lung disease, (Bronchopneumopathy obstructives, Asthma or other lung disease), heart disease and Covid-19.
The study population consisted of PLHIV on ART aged at least 15 years who were followed up in HIV care facilities in the Lingwala health district and who had visited HIV care facilities during the period from January 2021 to May 2023.
Statistical unit: The statistical units consisted of PLHIV with or without tuberculosis who visited the care facilities during the study period. Cases were coinfected PLHIV who developed TB during the study period, at least 6 months after the start of ART, and whose TB management had been initiated. The diagnosis of tuberculosis in HIV-positive patients was based on the guidelines of the anti-tuberculosis programme integrated into primary health care, version 6 of the NTCP. The diagnosis was made either by biology or clinically, based on the medical decision of the provider. The controls were PLHIV who had visited the HIV care facility and had not developed tuberculosis during the study period. The two groups (cases and controls) in the study were from the same care facilities population.
Inclusion and exclusion criteria: All PLHIV who had developed co-infection or not during the study period and whose informed consent was obtained before participating in the study. PLHIV who were followed up at the care facility and who had started ART at least 6 months after the start of the study were included in the study. Cases were those with evidence of confirmed tuberculosis reported in tuberculosis screening registers during the study period. This evidence consisted of the results of biological analyses, confirmation by providers including anti-tuberculosis treatment reported in the follow-up registers of PLHIV on anti-tuberculosis drugs. The controls were either PLHIV who had been tested for tuberculosis but whose results did not reveal tuberculosis, or PLHIV with suggestive signs whose diagnosis of tuberculosis was not accepted. Any patient in a very critical clinical state (patient in coma, in respiratory distress, in shock). These patients were excluded because of the difficulty of collecting reliable data, with a high risk of recall bias and non-response.
HC Vijana was removed from the list of facilities due to a lack of co-infected cases during the study period. The lists of cases and controls for the study period at each facility were compiled from ARV registers, individual records, patient monitoring software (Tiernet), screening registers and tuberculosis management registers. Cases were recruited exhaustively from the three management structures following a limited number of co-infected cases meeting the inclusion criteria. The number of controls was three times the number of cases for each management facility visited. They were recruited from each facility by simple random sampling from lists of controls compiled during the study period. Patients were classified by their identifier and in ascending order. Excel software was used to generate the random numbers from the lists for each facility. The list of controls was prepared for each health facility (Figure 1).
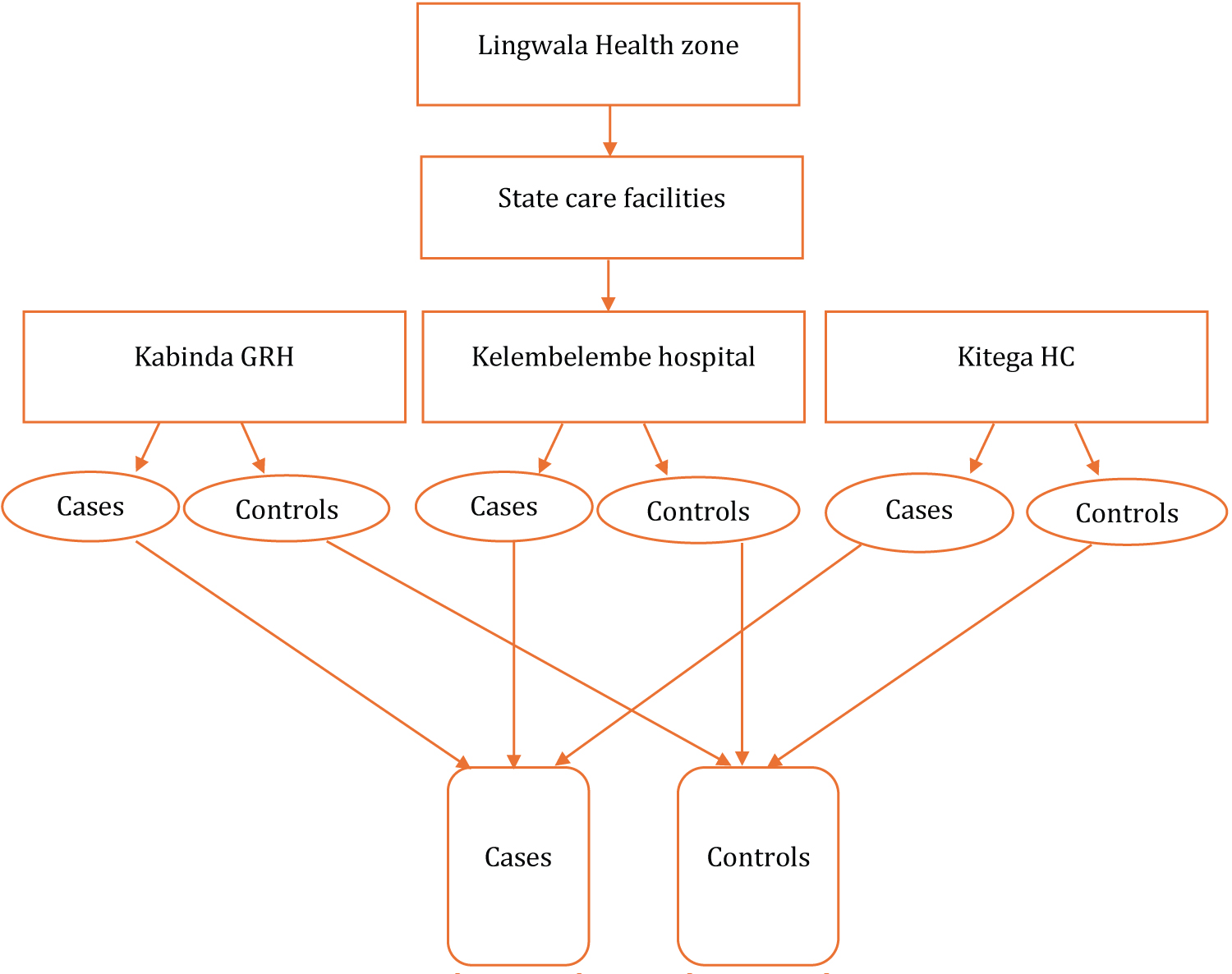 Figure 1: Origin of the cases and controls.
View Figure 1
Figure 1: Origin of the cases and controls.
View Figure 1
To establish the sample size, the study drew inspiration from a study conducted in Ethiopia in 2020. The sample size was calculated using Open Epi version 2.3.1 software, incorporating the proportion of 79.7% of patients with a viral load < 1000 copies in PLHIV without tuberculosis (controls) as the proportion of exposed persons among the controls and 41.6% of patients with a viral load < 1000 copies among the cases, significance level of 5%, ratio 1/3, power of 80% and with an OR = 5.5 (30). The minimum sample size calculated was 228 PLHIV, with 57 cases and 171 controls. In the field, the cases were all selected because of the limited number of cases. The sample size was therefore increased from 228 to 281, with 70 cases and 211 controls.
Data were collected using a questionnaire with closed-ended questions. Data were collected on the day of the patient visit or by inviting patients to the health facility. It consisted firstly of an interview with the patients for data relating to the search for risk factors and the socio-demographic characteristics of the patients enrolled in the study. This information was supplemented by the collection of information relating to the physical, biological and clinical characteristics reported in the patient management registers, patient follow-up files, patient monitoring software, screening registers and tuberculosis management registers during the study period (Appendix).
This was done at several levels, beginning with the development of the research protocol under the supervision of the dissertation director. The data collection tool was pre-tested with a view to readjustment. Each time, a meeting was held with the field agents and feedback was given to them after the meeting. The field supervisors worked closely with the interviewers to detect any errors. After each day's work, the principal investigator reviewed all the questionnaires. The data entry mask was created using a check program that filtered out any inconsistencies. Double data entry was carried out to minimise data entry errors.
The questionnaire was installed on the interviewers' phones using the ODK application, with different codes for cases and controls. Inconsistent data were corrected after verification. The data were exported to Excel 2016 followed by coding and then to SPSS version 25 for statistical analysis. Different categories were created, these included nutritional status with BMI (< 18.5 kg/m 2 , 18.5 to 24.99 kg/m 2 , 25 to 29.99 kg/m 2 , ≥ 30 kg/m 2 ). Viral load (< 1000 copies/ml and ≥ 1000 copies/ml). Duration of HIV infection (< 1 year, 1 to 4 years, 5 to 9 years and ≥ 10 years). The various codes were generated to facilitate analysis (profession, WHO clinical stage, comorbidity, use of alcohol or tobacco, 3 HP or isoniazid prophylaxis, co-infected status). Proportions were generated for categorical variables, and measures of central tendency and dispersion for quantitative numerical variables. The median and interquartile range were used when the distribution was not normal for the age variable. The U mann Whitney test was used to compare the median age of cases and controls after rejecting the hypothesis of the normality of the distribution. A bivariate analysis was first performed with each variable of interest to judge their effect on HIV/TB co-infection status. Variables with p ≤ 0.20 were retained in the multivariate regression model. Crude and adjusted odds ratios and 95% confidence intervals (CIs) were calculated for each variable of interest. The Hosmer-Lemeshow test was used to assess the fit of the logistic regression model. The value of p < 0.05 in the multivariate regression model was considered a statistically significant threshold value.
The informed consent of the participants and the authorisation of those in charge of the facilities were required prior to the interview and use of the patients' medical documents. The study was conducted in strict compliance with the ethical principles of biomedical research and monitoring. Subjects were informed about the conduct of the survey, and were told that there would be no remuneration after the interview, and that no health care would be provided. No physical, social (stigmatisation, indexation), psychological or economic harm was done to them. They were informed of the possibility of interrupting their participation in the study at any time. Confidentiality was strictly observed throughout the data collection process. This included data management, analysis and dissemination of results. The study was approved by the Ethics Committee of the School of Public Health at the University of Kinshasa under approval no. ESP/CE/188/2023.
Of the four care facilities identified, only three were included in the study after counting cases for each facility. Vijana HC was excluded for lack of HIV/TB co-infection cases meeting the selection criteria during the study period. The two health facilities, namely the Kabinda HGR and the Kalembelembe Hospital, have one-stop shops for HIV and TB care. The Kitega centre was the only facility that did not have a one-stop shop. A total of 281 PLHIV were included in the study, 70 of whom were considered cases and 211 controls (Figure 2).
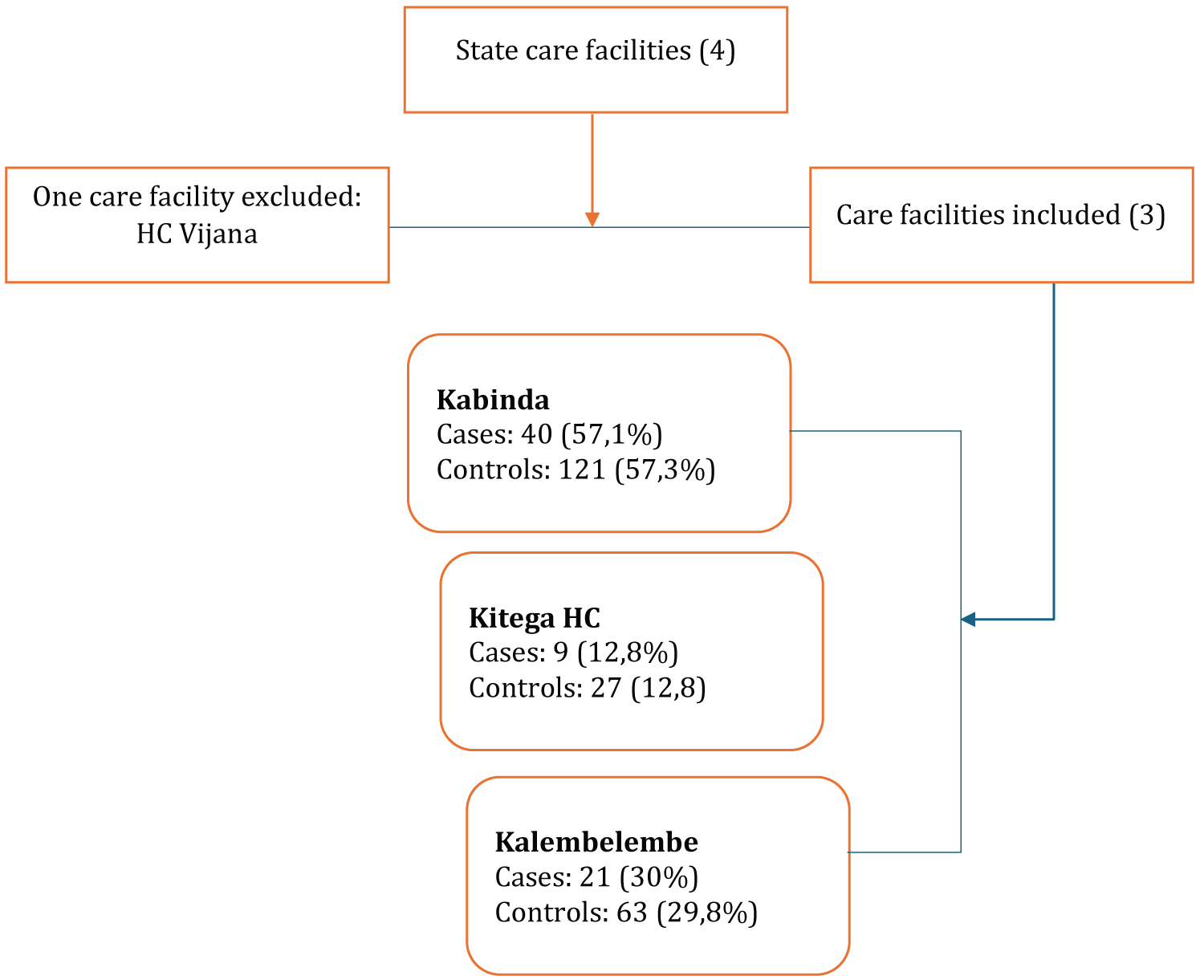 Figure 2: Distribution of patients enrolled in the study by care facility in the Lingwala health zone from 2021 to 2023.
View Figure 2
Figure 2: Distribution of patients enrolled in the study by care facility in the Lingwala health zone from 2021 to 2023.
View Figure 2
Overall, the median age of the PLHIV enrolled in the study was 45 years (SIR: 35 to 55 years). The majority of patients were female, with a sex ratio of one man to two women. The study showed that very few of the PLHIV enrolled reported having spent time in a prison environment, with a frequency of around 1.4% (Table 1).
Table 1: Socio-demographic and economic characteristics of PLHIV followed in care facilities from 2021 to 2023 (n = 281). View Table 1
The median age was 45 years (SIR: 37 to 53 years) in controls and 42 years (SIR: 29 to 55 years) in cases. However, the difference was not statistically significant. The gender distribution in the case and control groups was almost homogeneous. Many of the PLWHA were single (43.7%), followed by married (39.1%), divorced (12.4%) and living common-law (4.6%). Some 33.5% of PLWHA were not gainfully employed. The frequency of co-infection among PLHIV not in paid employment was high, at 30.8%, whereas 22.0% of those in paid employment had developed co-infection. Most of the PLHIV had an acceptable level of education, with at least primary schooling, while only 8.5% had no schooling. The majority of PLHIV (91.1%) lived outside the Lingwala health zone. All three facilities showed a remarkable predominance of PLHIV living outside the health zone, with a high contribution from the Kabinda HGR (57.8%), followed by the Kalembelembe hospital (30.5%) and the Kitega centre (11.7%).
The group of PLWHA with a duration of infection of between one and five years was in the majority, accounting for more than half (53.0%). Those with less than one year's infection and those with more than nine years' infection accounted for 14.2% of each. The contribution in number of cases from the one to five year age group was significant at 45.7%, followed by the 5 to 9, over 9 and < 1 year age groups (Figure 3).
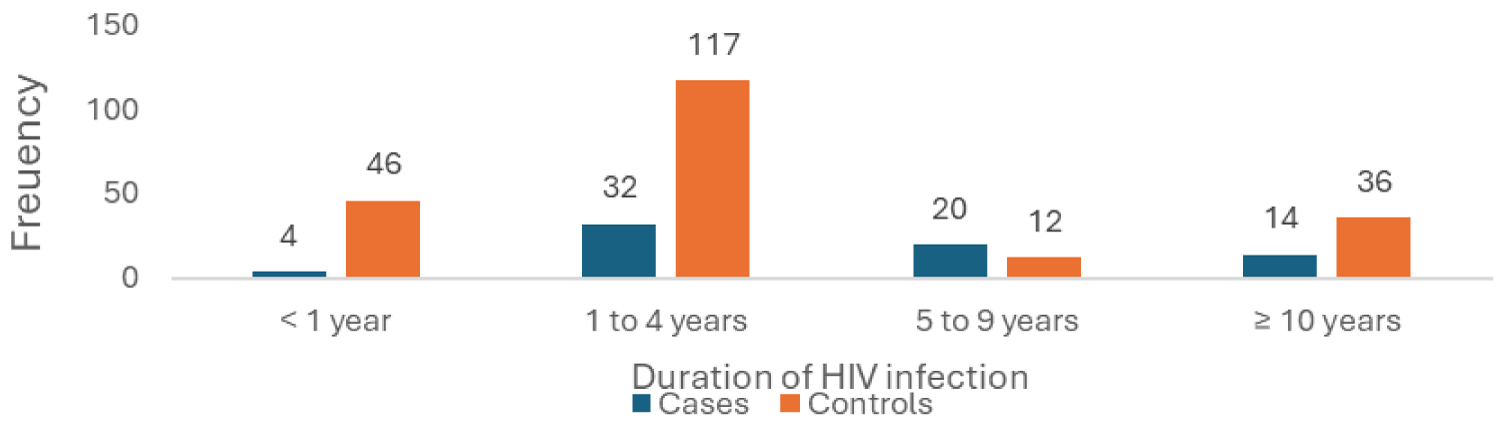 Figure 3: Breakdown of PLHIV followed up at care facilities by duration of HIV infection since discovery.
View Figure 3
Figure 3: Breakdown of PLHIV followed up at care facilities by duration of HIV infection since discovery.
View Figure 3
The study showed that the frequency of PLHIV with co-morbidity was 11% (p = 0.149), but the contribution of each disease was very low: 1.4% for diabetes mellitus, 3.9% for COVID-19, 1.8% for the presence of heart disease and 4.3% for lung disease [2]. Table 2 shows the other clinical characteristics considered in the study. The advanced clinical stage, particularly WHO stage 3, was predominantly represented among PLHIV who had developed co-infection, with a frequency of 80% compared with the other clinical stages.
Table 2: Clinical characteristics of PLHIV followed up in care facilities in the Lingwala HZ from 2021 to 2023 (n = 281). View Table 2
Approximately 51% of the PLHIV had a BMI within the normal range of 18.5 to 24.99%. Of these PLHIV with a normal BMI, 51.4% were co-infected. Underweight was observed in 17% of the PLHIV included in the study. Of these, 45.8% were coinfected. A history of tuberculosis was reported in 26.7% of the PLHIV enrolled, 70.6% of whom were co-infected. A large number of PLHIV reported having used alcohol at least once in the past. Nearly 27% of these were co-infected. Smoking was reported by only 12.8% of PLHIV. Forty-four percent of these had developed co-infection.
PLHIV in the Lingwala health zone received either INH or 3HP for the preventive treatment of tuberculosis. Some 56.0% of patients had received INH, 28.0% had received 3HP and 16.4% had not taken any preventive treatment (Figure 4). Of the PLHIV who had not received preventive treatment, the majority (97.8%) were at HGR Kabinda, followed by Kalembelembe Hospital (2.2%). Table 3 gives details of the biological and therapeutic characteristics analysed in the study.
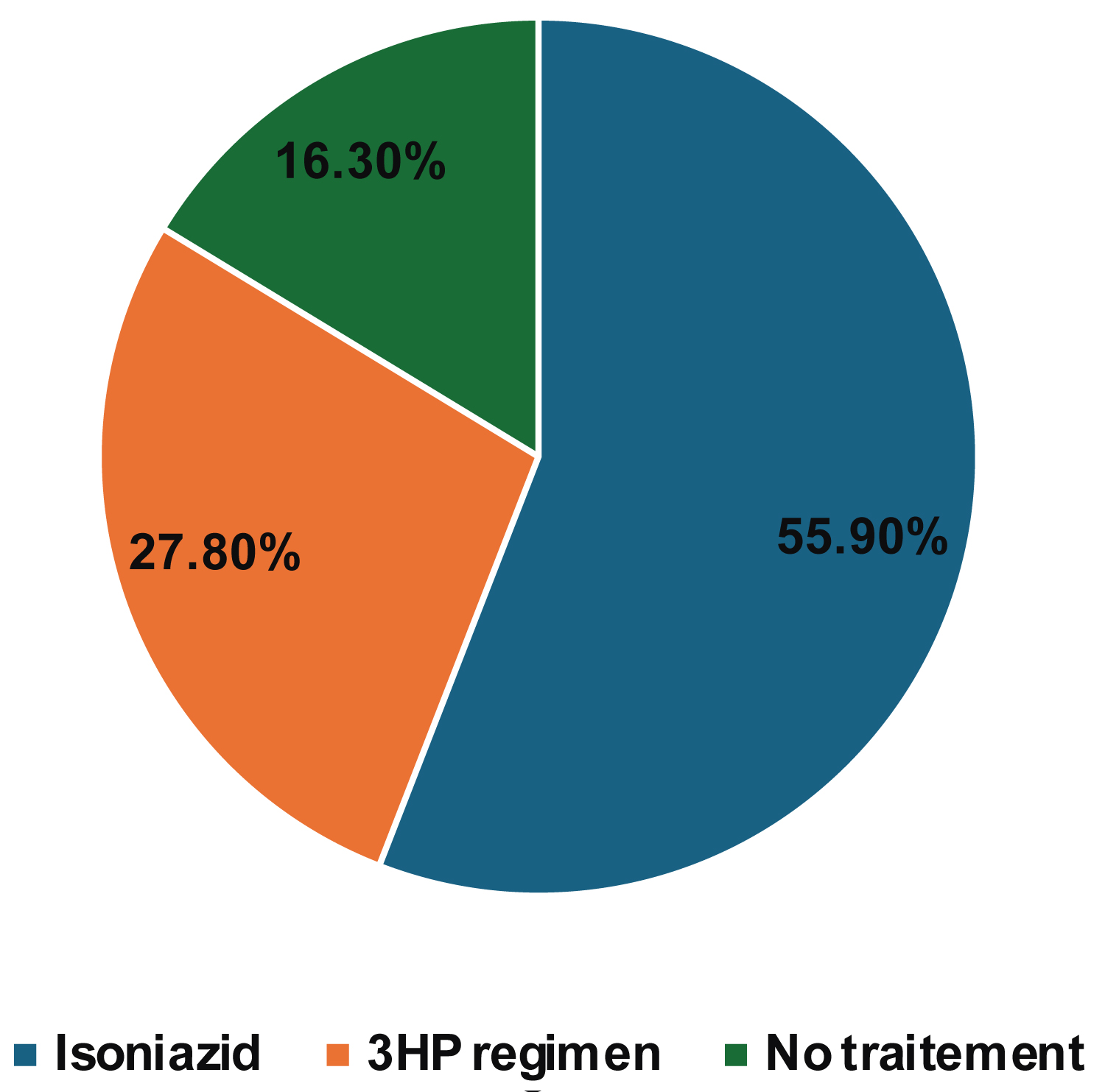 Figure 4: Breakdown of PLHIV by type of preventive treatment received in the past at care facilities.
View Figure 4
Figure 4: Breakdown of PLHIV by type of preventive treatment received in the past at care facilities.
View Figure 4
Table 3: Biological and therapeutic characteristics of PLWHA followed up at care facilities in the Lingwala HZ from 2021 to 2023 (n = 281). View Table 3
A total of 277 or 98% of the PLWH enrolled in the study had at least one viral load before or at the first visit during the study period. The proportion who did not have their viral load suppressed was 12.9%. The proportion of PLHIV with an unsuppressed viral load in the cases was significantly higher than in the controls. PLHIV with knowledge of tuberculosis preventive treatment represented more than three-quarters of the PLHIV enrolled. The proportion of PLHIV with no knowledge of preventive treatment among the cases was high compared with the controls. Almost 46% of the PLHIV had poor compliance, but there were more of them among the cases than among the controls (Figure 4).
Of all these factors, only a history of tuberculosis, viral load, 5 to 9 years of HIV infection and BMI < 18.5 kg/m 2 were associated with co-infection in HIV care facilities. Preventive treatment was not associated with co-infection after adjustment in the model (OR = 0.353; 95% CI; 0.963-8.320, p = 0.059). The presence of a history of tuberculosis among the PLHIV enrolled in the study was 20 times more frequent in co-infected patients than in those with no history of tuberculosis (OR = 20.84; 95% CI; 8.6-50.3, p < 0.01). The study showed that the duration of 5 to 9 years was observed almost 14 times in co-infected PLHIV (OR = 13.65; 95%CI; 2.19-85, p = 0.005). Non-suppression of viral load in PLHIV was five times higher than in co-infected PLHIV (OR = 5.34; 95% CI; 1.8-15.82, p = 0.002). The association between adherence to ARVs and co-infection was not statistically proven after adjustment of the model. Underweight PLHIV were three times more affected by co-infection than those of normal weight (OR = 3.26; 95% CI; 1.07-9.97, p = 0.038).
Bivariate analysis showed that smoking was about three times more common among co-infected patients than among other PLHIV enrolled in the study (OR = 2.83; 95% CI; 1.37-5.83, p = 0.005). Being divorced was a factor associated with the occurrence of co-infection among PLHIV in bivariate analysis (OR = 2.65; 95%CI; 1.14-6.15, p = 0.022). However, neither smoking nor marital status was associated with co-infection after adjustment of the model with other variables (Table 4).
Table 4: Factors associated with HIV/TB co-infection among PLHIV followed up in HIV care facilities in the Lingwala health zone from 2021 to 2023 (n = 281). View Table 4
The main factors associated with HIV/TB co-infection identified after multivariate analysis were a history of tuberculosis, viral load, 5 to 9 years of HIV infection and being underweight. CD4 lymphocyte count and haemoglobin were omitted from the list of variables due to data limitations. Stage of infection was removed from the logistic regression analysis because of inadequate reporting of data from patients' medical records.
The study showed that no socio-demographic factors were associated with co-infection. This would appear to be due to the composition of the sample, which approximately distributed the values of the variables in the two groups. However, Awachana Jiamsakul, et al. showed that low educational attainment was associated with HIV/TB co-infection [9]. The methodological approach used in this study, which included a large number of people living with HIV in 12 Asian countries, could explain this difference, apart from the composition of the populations. Nor have other studies demonstrated a link between age, sex and HIV/TB co-infection [10-13]. However, Nana ayegua, et al. found that in Florida, age 50 and over was associated with co-infection [14]. In Brazil, Thiago, et al. showed that the 20-39 age group was associated with co-infection [15]. In Africa, several studies have shown the link between co-infection and socio-demographic characteristics [16-18]. The trends could change if the study were extended to other health zones, in this case rural and semi-rural health zones. These results remain within the limits of the study area and cannot be extrapolated to all the DPS Kinshasa health zones. Carine Nkembi, et al. in the Nzanza HZ in the province of Kongo Centrale in Matadi in the DRC also did not establish an association between socio-demographic characteristics and co-infection. Only alcohol consumption was associated with HIV/TB co-infection [19].
The history of tuberculosis in the present study was related to patients having been declared tuberculosis patients at least once before the study period. Notification of tuberculosis was strongly associated with HIV/TB co-infection before and after adjustment for other variables in the logistic regression model. Several studies conducted in African regions and worldwide have established an association between the occurrence of tuberculosis in the past and HIV/TB co-infection [20-23]. Patients with a history of TB remain a risk group for developing TB because of pre-existing lesions. Racil, et al. found that in Tunisia, only hepatic cytolysis and tuberculin skin test (TST) were independent factors in recurrence [24]. Adherence to antiretroviral treatment in the study was not associated with HIV/TB co-infection. However, several studies have shown that adherence to ART is an important factor in the occurrence of HIV/TB co-infection [12,20]. The study period allowed us to increase the chance of recruiting cases meeting the inclusion criteria, although the risk of recall bias was not negligible. Nevertheless, we noted an association in the bi-variate analysis. The study showed that the duration of HIV infection between 5 and 9 years was associated with HIV/TB co-infection, whereas the other durations were not. The duration of HIV infection is a factor that exposes the patient to complications, particularly opportunistic infections, especially in patients with an unstable viral load. Chronic exposure to drugs can also lead to complications. However, this study does not establish a causal link. Several studies have also demonstrated this association between duration and co-infection. Zhezhe Cui, et al. found in the Guangxi region of China that the duration of infection beyond 5 years was associated with co-infection [25].
Bivariate analysis showed that taking preventive treatment was associated with a reduction in the number of co-infected patients, although this was not demonstrated after adjustment for other variables. Semu M, et al. found that in Ethiopia, isoniazid-based preventive treatment reduced the risk of tuberculosis in PLHIV [26]. The present study, however, found no association.
The study showed that co-infection was approximately five times higher in patients who had not suppressed their viral load compared with those who had suppressed their viral load. The paucity of patients who did not have a viral load allowed us to exclude them from the analysis, although we felt that this could not seriously affect the results. Lukas Fenner, et al. in South Africa established an association between the failure to suppress viral load and the occurrence of opportunistic infections in PLHIV on ART [27]. The strength of the association was weak compared with that found in the present study. Viral load was categorised into three classes in the study by Lukas, et al., which could dilute the strength of this association compared with ours. Several studies have demonstrated the relationship between increased viral load and the occurrence of opportunistic infections. Abdu M, et al. found a strong association between viral load and HIV/TB co-infection in Ethiopia [20]. The results of this study in relation to viral load are almost similar to those found in the present study.
Although the study period allowed us to recruit cases meeting the study criteria, this entailed a risk of recall bias among the patients surveyed. However this was minimised by the pretest of the data collection tool. The absence of data on certain variables prevented us from analysing certain factors.
This study showed that the factors associated with HIV/TB co-infection in PLHIV after initiation of ART in state-run HIV care facilities in the Lingwala Health Zone were a history of tuberculosis, 5 to 9 years of HIV infection, underweight and viral load. This study revealed certain shortcomings in the surveillance systems of HIV and TB care facilities. It thus paves the way for other studies to assess the effectiveness of certain therapeutic approaches. The detection of these factors in patients should encourage providers to actively search for tuberculosis so that it can be treated early. The fact that the study was carried out in the Lingwala HZ limits the extrapolation of the results obtained throughout the Kinshasa PHD.
We would like to thank the authorities of the Kinshasa Provincial Health Division, the Lingwala Health Zone and the authorities of the HIV care structures in the Lingwala Health Zone for accepting and facilitating the collection of data in the field. We would also like to express our gratitude to the team in the care division of the National HIV and STI Control Programme (PNLS), led by the Head of Division, Dr Patricia, for their comments and guidance during the course of this work. This work was made possible under the direction of Professor Nyandwe Kyloka, to whom we pay tribute for his efforts in providing guidance and direction throughout the process. We would also like to thank Dr Tacite, Dr Espérant Ntambwe and Dr Fabrice Sewolo for their contributions to this article.
The conception and design of the study were made by the author and approved by the Director, Prof. Nyandwe Kyloka of the School of Public Health at the University of Kinshasa. The data collection tool was designed by the author following the literature review and in line with the study's objectives, and was validated by the Director. The manuscript was successively reviewed by Dr Tacite from the medical imaging research centre, Dr Espérant Ntambwe and Dr Fabrice Sewolo from the 8 th FELTP cohort.
There were no competing of interest in this study.