In developing countries like Ghana, people with serious psychiatric disorders do not have equal access to health care as normal non-mentally challenged people do. Moreover, mental health care generally focuses on physical health screening, health education, and improving access to treatment in primary and secondary care to the detriment of sexual health needs including prevention of sexually transmitted infections. Studies have shown the risk of blood-borne virus infections such as HIV, hepatitis B virus, and hepatitis C virus has increased in the last few decades among people with psychiatric disorders. This study sought to determine the prevalence of HIV, HCV, HBV and syphilis infections in patients with psychiatric disorders.
In a cross-sectional study, 200 inpatients of Ankaful psychiatric hospital, aged ≥ 18 years diagnosed with schizophrenia, bipolar disorder, depression, psychiatric disorders, and substance abuse and dependence disorders formed the study population. Questionnaire interviews were conducted to obtain personal information and socio-demographic characteristics. Serological tests were performed on serum and plasma samples of participants to determine the prevalence of HIV, HCV, HBV and syphilis.
Seroprevalence for HIV was 5% (10/200), HBV was 9.5% (19/200), syphilis was 13.5% (27/200) and HCV was 2% (4/200). Results indicated a significant association between Schizophrenia diagnosis and the seropositivity for anti-HIV antibodies, anti-HBV antibodies and anti-T. pallidum antibodies. Co-infections and multiple infections among study participants showed 1.5% (3/200) seroprevalence of HBV and HIV co-infections. HBV and syphilis co-infections was 1.0% (2/200) and HIV and Syphilis co-infection was 0.5% (1/200). HCV and syphilis co-infection was also 0.5% (1/200). One patient had HIV, HBV and Syphilis 0.5% (1/200). The majority of the study subjects who tested positive for HBV, HCV and syphilis had no history of sex trafficking.
The current study shows that people with psychiatric disorders in Ghana are at increased risk of blood-borne viruses and STIs compared to the general population. Our results could form the baseline data for decision making by the health authorities, as there is an urgent need for developing prevention and care strategies for psychiatric patients in Ghana.
Psychiatric disorders, HIV, Hepatitis B, Hepatitis C, Syphilis, seroprevalence, Psychiatric hospital, Ghana
Reports by the World Health Organization (WHO) indicate that approximately 2.2 million Ghanaians suffer from mental disorders, and 650,000 of that suffer from severe mental disorder [1]. These include mental disorders such as schizophrenia, schizoaffective disorder, bipolar disorder, or psychosis. Notwithstanding the significant number and importance of psychiatric healthcare, there exists a huge deficit in terms of treatment and access to healthcare [2]. Current estimates predict about 98% treatment gap i.e. persons who need treatment but do not have access to adequate treatment.
In Ghana, mental health care generally focuses on physical health screening, health education, and improving access to treatment in primary and secondary health centers [3]. Sexual health needs of psychiatric patients receive little or no attention thus increasing the risk of psychiatric patients to sexually transmitted infections. While no representative epidemiological studies have been conducted to calculate the prevalence of HIV and other sexually transmitted diseases among people with different types of mental illness, a number of studies utilizing secondary data in different parts of sub-Saharan Africa have found high rates of HIV and sexually transmitted diseases (STDs) among people who were treated in specialty mental health settings [4].
Studies have shown the risk of blood-borne virus infections such as Human Immune-deficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV) has significantly escalated in the last few decades among people with psychiatric disorders [5]. The most common of these psychiatric disorders include major depressive disorders, dementia, substance use disorders, post-traumatic stress disorders (PTSDs), childhood conduct disorders, and cognitive and generalized anxiety disorders [6]. A major cause for this increased risk is due to the association of psychiatric disorders and substance abuse [7]. Substance use disorders are a critical issue among psychiatric patients, as they are not only risk factors for HIV and other viral transmissions but are also factors associated with reduced antiretroviral therapy adherence, clinical progression, reduced virological response and mortality [8]. Viral diseases such as HIV, HBV and HCV are transmitted by parenteral contact with contaminated body fluids (blood and blood products; contaminated instruments and needles; semen and vaginal fluids) and through unprotected sex (anal, vaginal, or oral) or by congenital transmission from mother to baby [9].
In Ghana, approximately 17% of HIV-infected individuals are also chronically infected with hepatitis B virus [10]. In direct contrast to developed countries, most HBV infections are acquired during early childhood, so patients with HIV/HBV co-infection have usually had chronic HBV infection for many years by the time they present with (or are tested for) HIV infection [11]. Although there is currently a national control strategy and action plan for HIV, there is none for the prevention and control of HBV, HCV and Syphilis in Ghana. Current STI control efforts usually target symptomatic patients and have failed to identify individuals with psychiatric disorders until serious complications develop.
This research thus sought to determine the prevalence of HIV, HCV, HBV and syphilis infections in patients with psychiatric disorders. Additionally, we analyzed the related risk factors associated with STI prevalence in psychiatric patients. The objective of this research is to provide comprehensive data to aid in policy decisions in providing a national control plan for psychiatric healthcare in Ghana.
A hospital based cross-sectional study was conducted at Ankaful psychiatric hospital in Central Region, Ghana. The hospital functions as one of the three (3) psychiatric hospitals in the country with additional responsibilities as a teaching hospital for both medical students and nurses in mental health and psychiatry. Persons aged 18 years and above, diagnosed with schizophrenia, bipolar disorder, depression, psychiatric disorders, substance abuse and dependence disorders admitted as in-patients at the hospital were considered eligible for the study. A well-structured questionnaire was used to obtain information on background characteristics, knowledge about HIV, HBV, HCV, and syphilis and vaccination. Information on history about forced sex and sex work, substance use/abuse behavior of all participants was collected. Confidentiality was assured at all times with the questionnaire given unique alphanumeric identifiers.
All in-patients of Ankaful psychiatric hospital, aged ≥ 18 years diagnosed with schizophrenia, bipolar disorder, depression, psychiatric disorders, and substance abuse and dependence disorders formed the study population. For calculation of the sample size, we assumed a minimum of 10% and a maximum 90% for STI sero-prevalence as expected frequency of the factor under study and a confidence level of 95%. The result of the calculation was a minimum of 138 subjects for accurate statistical inference [12]. A convenience sampling method was used to sample for the participants and elements of bias were controlled by ensuring that the sample was a miniature of the whole population under study. A total of 246 patients were initially recruited for the study out of which 233 were passed as psychologically stable by the Medical Officer-in-charge to partake in the study. Thirty-three (33) persons representing 14.2% of total eligible persons did not give consent to be part of the study and were duly excluded.
The Committee on Human Research, Publications and Ethics of the Kwame Nkrumah University of Science & Technology (CHPRE/KNUST) and the ethics board of the Ankaful Psychiatric hospital respectively, approved the study protocol. Written informed consent was also obtained from the participants before enrollment into the study. Emphasis was placed on the fact that participation was voluntary and there was the liberty of withdrawing from the study at any time without further obligation.
All patients who tested positive for HIV, HCV, HBV and syphilis were referred to the resident medical doctor at Ankaful Psychiatric Hospital for the appropriate disease treatment and management.
Close-ended questionnaires were administered to collect demographic as well as STI-related risk factors data. Questionnaires were administered in an interview format in participants' mother language for easy understanding. Questions sought personal information on participants including their knowledge about various STIs and related infection transmission risk factors. The possible infection transmission risk factors considered in the questionnaire included sexual orientation and sexual preferences, multiple sexual partners, substance abuse and condom usage.
From the cubital veins of participants, approximately 3 ml of blood was drawn using a sterile butterfly hypodermic syringe and needles and dispensed into a serum separator tube and transported on ice to the laboratory. The samples were centrifuged at 1500 rpm for 10 minutes to obtain serum and stored at -80 ℃ until analyzed.
Serum obtained from the study subjects were screened using two commercial test kits recommended for use nationwide by the Ministry of Health in Ghana. Antibodies to HIV were detected using Ora Quick ADVANCE Rapid HIV-1/2 antibody (first line screening) and the positive test results were confirmed with the One Step Anti-HIV (1 and 2) Tri-line Test. In the event of a discordant results between the two test kits, a commercially available Western Blot Assay kit (HIV BLOT 2.2) supplied by MP Diagnostics was used to decide the results. The One Step Anti-HIV (1 and 2) Tri-line Test is a colloidal gold enhanced rapid immuno-chromatographic assay for detecting antibodies of all isotypes (IgG, IgM, IgA) to HIV 1 and HIV-2. All reactive samples from the One Step Anti-HIV1 and 2 Tri-line Test (First Response) were retested with OraQuick® ADVANCE Rapid HIV-1/2 Antibody Test (OraSure Technologies, Inc. USA) for confirmation. All tests were performed strictly according to the manufacturer's instructions.
Serum samples from the study subjects were tested for hepatitis B surface antigens (HBsAg) using the Accu-Tell® One Step HBsAg rapid test (AccuBio Tech Co., Ltd.). The Accu-Tell® One Step HBsAg rapid test employs sandwich immunoassays in the detection of HBsAg in serum or plasma. Antigens in sample bind to recombinant anti-HBsAg antibodies conjugated to colloidal gold particles in the sample well and resulting mixture move alone the cellulose membrane which contains the test region and the control region. The HBsAg-HBs antibody-conjugate complex binds to the anti-HBsAg antibodies immobilized in the test region and a color develops which indicates positive results. Color development at both test and control region indicates valid positive test results and color development at the control region alone is an indication of valid negative test results. All positive samples were confirmed using Roche COBAS e411 analyzer with elecsys HBsAg II quant test (Roche Diagnostics, Germany).
Serum samples from the study subjects were tested for hepatitis C virus (HCV) using Rapid Test kits (Cortez Diagnostics, California USA). The test kit operates on the principle of double antigen sandwich immunoassay. Purified recombinant antigens identify anti-HCV antibodies specifically. Negative test results show only one colored band on the control C region with no apparent band on the test (T) region. Positive HCV Rapid test results show a pink-colored control C band, with a distinct pink-coloured band in the test (T) region.
Samples were screened for syphilis using Accu-Tell® One Step Anti-Treponema pallidum test (AccuBio Tech Co., Ltd.). This rapid test employs the sandwich principle in detecting antibodies to Treponema pallidum in serum. The test card has a sample well in which Treponema pallidum antigen (TP Ag 1) conjugated with colloidal gold particles has been immobilized. Recombinant Treponema pallidum antigens (TP Ag 2) has been immobilized in the test region and anti-Treponema pallidum antibodies in the control region. On application of the test sample, the anti-Treponema pallidum antibodies bind to the conjugated TP Ag 1 which forms a colored mixture. As the colored mixture migrate chromatographically along the nitrocellulose membrane in the card, if the test sample contains anti- Treponema pallidum antibodies, the antibodies bind to the TP Ag 2 in the test region and a color develops indicating a positive result. No color development is an indication of negative results. As the mixture migrate to the control region the TP Ag 1 in the conjugate binds to the immobilized antibodies in the control region and a color develops. Color development in the control region is an indication that the TP Ag 1/colloidal gold conjugate is potent. Color development at the test and control region is an indication of valid positive results. Color development at the control region alone is an indication of valid negative results; however, color development at the test region alone indicates invalid test results.
Data analysis was performed using SPSS version 16.0. Difference in non-scalable variables such as age and sex of the study populations were assessed by Mann-Whitney U rank sum with p values < 0.05 considered significant (CI: 95%). Chi-square (χ2) test was used to determine associations between categorical variables. p values < 0.05 was considered statistically significant. Univariate analysis was used to predict the association between HIV, HBV, HCV and Syphilis infections among people with psychiatric disorders among the study population and risk factors.
A total of two hundred (200) psychiatric patients (Mean age (35.60 ± 12.06 years) admitted at the Ankaful psychiatric hospital participated in this study. They comprised of 55% males {110/200 (mean age 33.3 ± 10.9 years)} and 45% females {90/200 (mean age 38.4 ± 12.9 years). Factors such as marital status, educational level and number of children showed significant differences whiles age and employment status showed no significant differences. Results of general characteristics of participants is presented in Table 1.
Table 1: General characteristics of study participants. View Table 1
The overall sero-prevalence for HIV was 5% (10/200) out of which 70% (7/10) were females with the remaining 30% (3/10) being males (Table 2). Sero-prevalence for HBV was 9.5% (19/200) (comprising 52.6% (10/19) males and 47.4% (9/19) females) and the total prevalence for HCV was 2% (4/200). Overall sero-prevalence for syphilis among study participants was 13.5% (27/200) which comprised of 44.4% male (12/27) and 55.6% female (15/27). Results are presented in Table 2.
Table 2: Sero-prevalence of HIV, HBV, HCV and Syphilis of participants categorized by gender and age. View Table 2
Co-infections and multiple infections among study participants showed 1.5% (3/200) sero-prevalence of HBV and HIV co-infections (Figure 1). HBV and syphilis co-infections was 1.0% (2/200) and HIV and Syphilis co-infection was 0.5% (1/200). HCV and syphilis co-infection was also 0.5% (1/200). Prevalence of patients who had HIV, HBV and Syphilis was 0.5% (1/200).
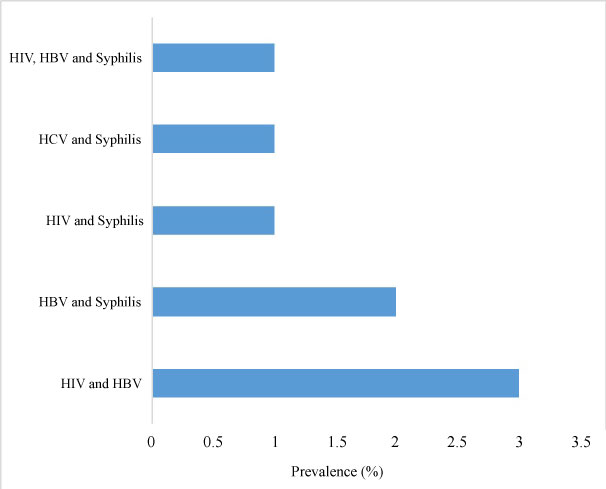 Figure 1: Prevalence of co-infections and multiple infections among study participants. View Figure 1
Figure 1: Prevalence of co-infections and multiple infections among study participants. View Figure 1
Psychotic diagnosis of the participants was related to sero-positivity of HIV, HBV, HCV and syphilis by univariate analysis. Results indicated a significant association between Schizophrenia diagnosis the sero-positivity for anti-HIV antibodies, anti-HBV antibodies and anti-T. pallidum antibodies (Table 3). Additionally, the results also indicated a significant association between psychotic disorder, bipolar and depression diagnosis association with anti- T. pallidum antibodies. There was however no significant association between HCV sero-positivity and psychotic diagnosis.
Table 3: Psychiatric diagnosis associated with HIV, HBV, HCV and Syphilis sero-positivity in participants by univariate analysis. View Table 3
To understand the association of sexual lifestyles and sero-positivity of HIV, HBV, HCV and syphilis, we performed a univariate analysis. Results obtained indicated that heterosexuality was significantly associated with HIV, HBV, HCV and syphilis sero-positivity (Table 4). In addition, we found out that participants who had regular sex partners were significantly associated with HIV infections. Majority of the study subjects who tested positive for HBV, HCV and syphilis had no history of forced sexual activity such as exchange of sex for money, food, shelter or drugs. However, there was no significant difference in terms of condom usage and infections with HIV, HBV, HCV and syphilis although a greater number of participants admitted to the use of condoms during sex (Table 4).
Table 4: Association of sexual lifestyles with HIV, HBV, HCV and Syphilis sero-positivity in participants by univariate analysis. View Table 4
In this study, we show the prevalence of HIV, HCV, HBV and syphilis infections in patients with psychiatric disorders. This is the first published study of its kind in a psychiatric hospital in Ghana.
We found a trend towards a higher HIV-prevalence among this population, with a prevalence of 5%, which was significantly higher than the national prevalence of 1.6% [13]. Psychotic symptoms in HIV positive patients have been associated to the direct neuropathic effect of the virus on the brain or may be secondary due to the effect of medication or substance abuse, secondary due to opportunistic infections or from the psychological impact of the knowledge of an HIV diagnosis [14]. There are reports that suggest that mental illness is a risk factor for developing HIV infection [15-18]. Psychiatric patients may show high-risk sexual behaviour, suffer less often from social exclusion that may lead to exchange of sex for money or goods, and have less severe cognitive deficit that impairs judgement or the ability to negotiate safe sex [9]. It is well established that drugs of abuse alter judgment, induce loss-of-inhibition, and play a massive role in the spread of HIV by leading to engagement in impulsive and unsafe behaviors [20].
In Ghana, available evidence shows that viral hepatitis is ten times more common than human immune deficiency virus (HIV) infection [11]. However, there is no comprehensive viral hepatitis prevention and control programme analogous to that of HIV/AIDS that provides public awareness of the disease and access to treatment. Previous studies on Ghanaian blood donors show HBV prevalence at > 10%, increasing in the rural and deprived areas [21,22], while that of HCV was estimated at more than 3% in some rural communities [23].
Additionally, we analyzed the related risk factors associated with blood-borne viruses and syphilis infections. Factors such as intravenous drug use and sexual behaviour, history of alcohol abuse, lack of condom use, having multiple sexual partners, sex trading, partner with a blood-borne virus were analyzed. There was no significant association between the blood-borne viruses, syphilis and forced sexual activity such as the exchange of sex for money, food, shelter or drugs. Consistent with our observation, majority of the participants were aware of the risk factors influencing the acquisition and spread of HIV, HBV, HCV and syphilis. The high level of awareness of blood borne viruses and syphilis infections exhibited by our study population could be associated with the vigorous HIV/AIDS awareness campaign ongoing in Ghana [24].
Patients with severe mental illness who are HIV positive may have more than one psychiatric diagnosis, as well as an elevated prevalence of co-morbid medical disease such as TB and hypertension [25]. From this study, co-infection with other blood borne viruses and syphilis thus raises questions of possible extreme susceptibility of these patients. This therefore underscores the need for clinicians to be vigilant in detecting various neuropsychiatric manifestations of HIV infection. If detected timeously, co-morbidities addressed; and antiretroviral therapy and psychotropic initiated early, this would have a positive impact on the prognosis of a patient resulting in an improved quality of life. Staff at HIV treatment clinics should also have sufficient expertise in assessing the signs and symptoms of mental illness and realize the importance of referrals to specialists when necessary.
A possible study limitation, which merits discussion, is that participants were recruited from a treatment site and results may not be generalizable to all people with mental illness. However, we estimate that this limitation had minimal effects on our findings since most people consented, and the sample exceeded the calculated sample size.
From our study, we propose the need for routine HIV, HBV, HCV and syphilis screening over targeted, risk-based testing in psychiatric settings in Ghana. This routine screening in mental health settings will provide an opportunity for counselling and enhancing patients' knowledge of risk factors and prevention. Additionally, it will possibly identify many seropositive patients who may be overlooked in a system reliant on self-identified risk [26]. People with severe mental illness have higher all-cause mortality than those without [27]. It is possible that people with severe mental illness are not receiving recommended HIV, HCV, HBV and syphilis-related healthcare, since there is no regular testing of such infections.
In conclusion, mental health services in Ghana, which has a generalized HIV epidemic, need to take into account the frequent co-morbidity of HIV, viral hepatitis and syphilis. Periodic risk assessment, counselling and testing, and treatment and care of HIV, HCV, HBV and syphilis should be integrated with mental health services. Conversely, HIV treatment programs should take into account the high burden of mental illness among persons with HIV and integrate mental health assessments and interventions with routine HIV care. Our results could form the baseline data for decision making by the health authorities, as there is an urgent need for developing STI prevention and care strategies for this population in Ghana.